 |
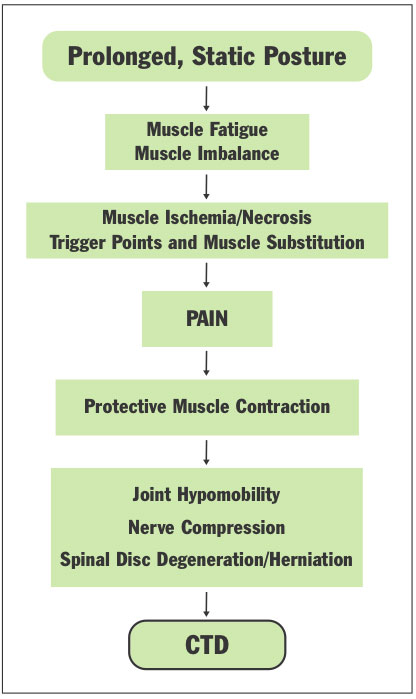
| Figure 1. Flowchart showing how prolonged, static postures (PSPs) can progress to pain or a cumulative trauma disorder (CTD). |
INTRODUCTION
According to a 2010 study, women who sit more than 6 hours each day have approximately a 40% higher death rate and men a 20% higher death rate than those who sit less than 3 hours a day.1 This is not good news for dentists, who tend to sit in excess of 6 hours during an average 8-hour day.2
The human body was designed for movement. Over thousands of years, the human body has depended on movement for its survival. But industrial and technological advances have done much to impede Mother Nature. With the onset of the Industrial Revolution, increasing numbers of workers performed relatively stationary tasks. With the advent of computers, the number of sedentary jobs has increased, as have the number of musculoskeletal disorders. One study showed the prevalence of low-back pain has increased by 2,700% from 1980 to 1993;3 a British study found that nearly one third of dentists who retire early are forced to, due to a disability;4 and numerous dental studies report that an average of 2 out of 3 dentists experience musculoskeletal pain.5-16 It is reasonable to infer that changes in the way we use our bodies has contributed to this dramatic increase in work-related pain. In short, the body must move—and move properly—to stay healthy.
Since the introduction of seated (4-handed) dentistry, dentists tend to work for longer periods of time without taking a break, and they perform longer procedures.12 Consider that when you sit in a static operating posture without leaning on your chair’s backrest, more than 50% of your body’s muscles must contract to hold the body motionless while resisting gravity. The static forces resulting from these prolonged, static postures (PSPs) are much more taxing on the body than dynamic (moving) forces.13
The resultant microtrauma from these PSPs include muscle imbalances, muscle ischemia, trigger points and spinal disc degeneration. This microtrauma develops through a series of events (Figure 1).
PROBLEMS ASSOCIATED WITH PROLONGED STATIC POSTURES
Muscle Imbalances
Even with the best ergonomic equipment, dentists frequently find themselves slightly leaning, usually more in one direction than the other. For example, most right-handed dentists tend to lean forward and to the right when they leave their neutral operating posture.17 Over time, the muscles can adaptively shorten on one side of the body, spine, or joint. This imbalance can exert asymmetrical forces, causing misalignment of the spinal column or in joints, with loss of range of motion in one direction over the other.18
Over time, the body’s musculature can adapt to the abnormal posture caused by these muscle imbalances and tend to maintain this unbalanced posture not only at work, but in leisure activities as well.
Muscle Ischemia
Maintaining static postures in dentistry requires sustained muscle contraction. When a muscle is contracted for a prolonged period of time, intramuscular pressure rises. This pressure compresses the blood vessels within the muscle, and during strong static contractions, can almost completely obstruct blood flow through the muscle.19 As lactic acid accumulates, muscular pain and fatigue result.19-21 Even in the best working postures, dentists’ bodies perform static muscle work in the dental operatory.
Dynamic muscle work, on the other hand, creates a healthier environment for bodily repair. The rhythmic, pump-like contraction and relaxation of the muscles ensures adequate blood flow and oxygen to the muscles, as well as lactic acid removal.
Recovery time is relatively rapid after brief periods of high-level intensity muscle work, such as 20 minutes of uphill bicycling. However, recovery time from low-level muscle fatigue after working a 7- to 8-hour day (as in dentistry) is much longer. There is a risk that muscles may not even recover by the following workday. Human muscles are not designed for continuous, long-lasting contractions. They require rest periods to recover from even low-level exertion.22 It is a physiologic certainty that if the rate of tissue damage exceeds the rate of repair due to insufficient rest periods, muscle necrosis can result.
Trigger Points
Most dentists are already painfully familiar with trigger points. A trigger point is a group of muscle fibers that are in a constant state of contraction. They feel like a hard knot, nodule, or small pea. When pressed upon, they may be painful locally or refer pain to a distant part of the body. They neither allow the muscle to contract nor relax, thereby effectively decreasing flexibility and range of motion. Trigger points may be active (painful) or latent (causing stiffness and restricting range of motion).23 Because they are caused by prolonged muscle ischemia, postural asymmetry and mental stress, it is easy to see why trigger points are so common among dental professionals.
Disc Degeneration
By adulthood, there is no blood supply to the inside of your spinal disc, and its only means of nutrition is via imbibition.24 Think of the disc as a sponge. At rest, it absorbs no water; however, when compressed and released, it imbibes water. This is similar to the mechanism of the spinal disc. It requires alternate compression and relaxation to stay healthy. Sustained contractions in the muscles that extend your spine (as during active sitting) also reduce disc nutrition by compressing the discs, increasing intradiscal pressure.25
Finally, lumbar disc pressures are generally higher when sitting than when standing. Compared to standing, lumbar disc pressures increase by 40% when you sit “actively” (without leaning on a backrest), and by 200% when sitting and leaning forward 40°.26 This has particular relevance to dentistry, since dentists tend to sit for 78% of their working hours.2
PREVENTION THROUGH MOVEMENT
Movement is imperative in your operatory to decrease the structural damage from PSPs. You can incorporate the following movement strategies to help you move the workload from one group of muscles to another, prevent painful muscle ischemia, and reduce static spinal disc loading.
 |
 |
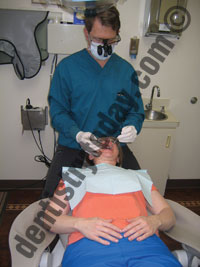 |
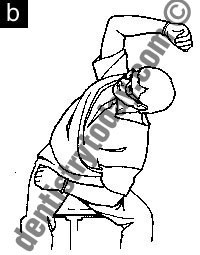
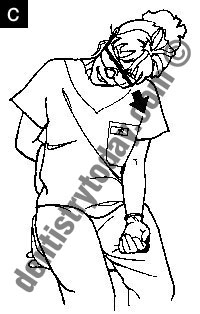
| Figures 2a to 2c. Dentists should frequently utilize different clock positions to move the muscle workload, keeping in mind that the line of sight (perpendicular to the occlusal surface) should dictate the ideal clock position. |
1. Change operating positions— Moving frequently between the 8 to 12 o’clock positions around the head of the patient is important; as you move around the patient’s head, the workload shifts slightly from one area in your body to another (Figures 2a to 2c). Your clock position will largely depend upon which position enables you a line of sight that is perpendicular to the occlusal surface.27 The 12 o’clock position provides the most neutral, ergonomic operator posture, and should be utilized whenever possible. Note that when the patient chair is reclined, there should be at least 20″ of clearance between the headrest of the patient chair (when reclined) and counter.28 If access in the 12 o’clock position is blocked, swivel the patient chair to improve access. A common ergonomic error among dentists is not positioning the patient properly when working on the upper arch, causing forward leaning and twisting. The occlusal plane of the upper arch should be up to 25° backward in relation to the vertical plane.27,29 (For a full article on patient positioning, please read “Ergonomic Positioning: A Few Degrees Can Add Years to Your Career,” Dentistry Today, September 2010 available at dentistrytoday.com).
2. Switch stools—Research shows that regularly changing your seated posture can reduce low back pain.30 Consider placing a traditional stool with armrests in one operatory, and a saddle-style stool in another (Figure 3). The saddle stool will place the dentist halfway between standing and sitting; this position uses different muscles than traditional seating, also decreasing spinal disc pressure.
 |
| Figure 3. The ideal sitting posture is one that changes. Try using one type of chair in one operatory and a different style in another. |
Saddle stools have additional ergonomic benefits for the dentist. By placing the pelvis in a neutral position, the natural spinal curves are more easily maintained.31 Since they open the hip angle, saddle stools are ideal for gaining close proximity in the 9 o’clock position (especially helpful when working with wide patient chairs), and a good choice for dentists with short torsos who frequently find themselves working with elevated arms. The saddle stools allow for lower positioning of the patient and more relaxed arm and shoulder posture. They are also very easy to move around the patient’s head and great for confined operatory spaces. (For an in-depth article on operator ergonomic considerations when selecting operator stools, read the Dentistry Today September 2008 article, “Operator Stools: How Selection and Adjustment Impact Your Health” available at dentistrytoday.com.)
3. Moving seats—Studies show that seats that allow movement help prevent low-back pain and have positive ramifications for spinal health.30 There are several styles on the market today. The new Virtu Dental Stool (Crown Seating) has dynamic movement technology that enables both the seat pan and backrest to follow the movement of the user. Brewer Design makes a dental stool with an air-filled bladder under the seat that may be inflated to allow varying degrees of movement. An air-filled, wedge-shaped seat cushion retrofits a nontilting operator stool and also offer the benefits of movement in the lumbar spine.32
 |
| Figure 4. Alternating between standing and sitting has been shown to reduce lower back pain. Consider standing for extractions, injections, exams, denture adjustments, and impression-making. |
4. Alternate between standing and sitting—One study reveals that dentists who alternate between standing and sitting have less low back pain than dentists who worked solely in a seated position.13 Dentists tend to spend more than three quarters of their total working hours seated, which places increased pressure on the lumbar discs.2 Consider standing for extractions, exams, denture adjustments, injections and impression-making (Figure 4). You will need to ensure that your patient chair elevates to a height that enables a neutral standing posture when working. When standing, and especially for extractions, the mouth should be just below elbow level.
| Stretching Safely |
| It is important to know how to stretch safely. The following is an excerpt from the Smart Moves in the Operatory: Chairside Stretching DVD by Ms. Valachi: To avoid injury during stretching, keep the following tips in mind: • Assume the starting position for the stretch • Breathe in deeply and exhale as you slowly increase the intensity of the stretch up to a point of mild tension or discomfort • Hold the stretch for 2 to 4 breathing cycles (10 to 20 seconds) • Slowly release the stretch—come back to neutral position. Repeat the stretch, if time allows. • Try the stretch in both directions, and determine which side is tightest. Perform the directional stretch primarily toward the tightest side throughout the workday, and place stretching charts where you can easily reference them. • Never stretch in a painful range. If stretching increases your pain, stop immediately. |
5. Reposition the feet—Contrary to what many dentists learned in dental school, the feet need not be statically placed in a tripod position throughout a procedure. The newest research in spinal biomechanics supports frequent repositioning during sitting.30 Alternate between the following: both feet in tripod position, placing one foot (then the other), up on the stool pedestal, straddling the patient, or a runner-up position (one leg slightly down, behind and back). Shifting the rheostat from one foot to the other is also an effective way to move the muscle workload from one side of the low back to the other.
6. Chairside stretching—Research reveals that taking frequent breaks and moving are integral to an effective injury prevention program and pain control in dentistry (Figures 5 a to 5c).15
 |
 |
 |
| Figures 5a to 5c. Chairside stretching is the only operatory ergonomic intervention that addresses every microtrauma resulting from PSPs. (a) Neck and shoulder combo, (b) Untwister, and (c) Upper trapezius stretch. (Photos from Smart Moves in the Operatory: Chairside Stretching DVD. All 20 stretches available at posturedontics.com.) |
Frequent chairside stretching addresses every microtrauma that results from prolonged, static postures in dentistry: ischemia, trigger points, muscle imbalances, joint hypomobility, nerve compression, and disc degeneration.28 The time commitment is minimal (only 10 to 20 seconds) and the benefits of stretching are numerous and include: increasing blood flow to muscles; increasing production of joint synovial fluid; reducing the formation of trigger points; maintaining normal joint range of motion; and increasing nutrient supply to spinal discs.
An effective chairside stretching program in dentistry targets those muscles and structures that are prone to ischemia and tightness. Not all stretches are appropriate for dental professionals.
Stretching During Microbreaks
It is important to know how to stretch safely (Sidebar). Chairside stretches should be performed every 45 to 60 minutes throughout the day22 and able to be performed easily at chairside while wearing gloves. Since men tend to be more prone to injuries related to tightness, it is especially imperative for male dentists to incorporate stretching into their daily regimen. Take advantage of 10 to 20 second microbreaks throughout the workday to stretch: while the assistant is light-curing or taking impressions, waiting for anesthetic to take effect, between patients, during a missed appointment, or during a recall exam.
CLOSING COMMENTS
Dentists know the importance of prevention, and you teach it to your patients on a daily basis. I challenge you to make a resolution in 2011 to implement movement prevention strategies to protect the significant investment you’ve made in your career and ensure a high quality of life, prevent disabling injuries and extend your career.
References
- Patel AV, Bernstein L, Deka A, et al. Leisure time spent sitting in relation to total mortality in a prospective cohort of US adults. Am J Epidemiol. 2010;172:419-429.
- Marklin RW, Cherney K. Working postures of dentists and dental hygienists. J Calif Dent Assoc. 2005;33:133-136.
- Pope M. Muybridge lecture. In: Proceedings of the International Society of Biomechanics XIVth Congress. Paris, France. July 1993.
- Burke FJ, Main JR, Freeman R. The practice of dentistry: an assessment of reasons for premature retirement. Br Dent J. 1997;182:250-254.
- Akesson I, Schütz A, Horstmann V, et al. Musculoskeletal symptoms among dental personnel;-lack of association with mercury and selenium status, overweight and smoking. Swed Dent J. 2000;24:23-38.
- Alexopoulos EC, Stathi IC, Charizani F. Prevalence of musculoskeletal disorders in dentists. BMC Musculoskelet Disord. 2004;5:16.
- Augustson TE, Morken T. Musculoskeletal problems among dental health personnel. A survey of the public dental health services in Hordaland [in Norwegian]. Tidsskr Nor Laegeforen. 1996;116:2776-2780.
- Chowanadisai S, Kukiattrakoon B, Yapong B, et al. Occupational health problems of dentists in southern Thailand. Int Dent J. 2000;50:36-40.
- Fish DR, Morris-Allen DM. Musculoskeletal disorders in dentists. N Y State Dent J. 1998;64:44-48.
- Finsen L, Christensen H, Bakke M. Musculoskeletal disorders among dentists and variation in dental work. Appl Ergon. 1998;29:119-125.
- Lalumandier JA, McPhee SD, Parrott CB, et al. Musculoskeletal pain: prevalence, prevention, and differences among dental office personnel. Gen Dent. 2001;49:160-166.
- Marshall ED, Duncombe LM, Robinson RQ, et al. Musculoskeletal symptoms in New South Wales dentists. Aust Dent J. 1997;42:240-246.
- Ratzon NZ, Yaros T, Mizlik A, et al. Musculoskeletal symptoms among dentists in relation to work posture. Work. 2000;15:153-158.
- Rucker LM, Sunell S. Ergonomic risk factors associated with clinical dentistry. J Calif Dent Assoc. 2002;30:139-148.
- Rundcrantz BL, Johnsson B, Moritz U. Cervical pain and discomfort among dentists. Epidemiological, clinical and therapeutic aspects. Part 1. A survey of pain and discomfort. Swed Dent J. 1990;14:71-80.
- Shugars D, Miller D, Williams D, et al. Musculoskeletal pain among general dentists. Gen Dent. 1987;35:272-276.
- Kihara T. Dental care works and work-related complaints of dentists. Kurume Med J. 1995;42:251-257.
- Saunders HD, Saunders RL, Kraus SL, et al. Evaluation, Treatment and Prevention of Musculoskeletal Disorders. Volume 1. The Spine. 3rd ed. Bloomington, MN: Educational Opportunities, A Saunders Group Company; 1993:47, 100-101.
- Kroemer KHE, Grandjean E. Fitting the Task to the Human: A Textbook of Occupational Ergonomics. 5th ed. Philadelphia, PA: Taylor & Francis; 1997:8.
- Kumar S. Biomechanics in Ergonomics. Philadelphia, PA: Taylor & Francis; 1999:12.
- Cailliet R. Soft Tissue Pain and Disability. 3rd ed. Philadelphia, PA: FA Davis; 1996:71-72.
- Sjogaard G and Jensen BR. Low-levels of Static Exertions. In: Marras WS and Karwowski W (Eds). Fundamentals and Assessment Tools for Occupational Ergonomics. Boca Raton, Fla: CRC Press; 2006:14-1-14-13.
- Simons DG, Travell JG, Simons LS. Travell & Simons’ Myofascial Pain and Dysfunction: The Trigger Point Manual. Volume 1. Upper Half of Body. 2nd ed. Baltimore, MD: Lippincott Williams & Wilkins; 1999:4,12,19,35,329-396.
- Cailliet R. Low Back Pain Syndrome. 5th ed. Philadelphia, PA: FA Davis; 1995:10, 94-143, 279.
- Ortengren R, Andersson GB, Nachemson AL. Studies of relationships between lumbar disc pressure, myoelectric back muscle activity, and intra-abdominal (intragastric) pressure. Spine (Phila Pa 1976). 1981;6:98-103.
- Nachemson AL. Disc pressure measurements. Spine (Phila Pa 1976). 1981;6:93-97.
- Hokwerda O, de Ruijter R, Shaw S. Adopting a healthy sitting working posture during patient treatment. optergo.com/uk/images/Adopting.pdf. Accessed February 18, 2011.
- Valachi B. Practice Dentistry Pain-Free: Evidence-Based Strategies to Prevent Pain and Extend Your Career. Portland, OR: Posturedontics Press; 2008:102.
- Murphy DC, ed. Ergonomics and the Dental Care Worker. Washington, DC: American Public Health Association; 1998:246-249, 306.
- McGill S. Low Back Disorders: Evidence-Based Prevention and Rehabilitation. Champaign, IL: Human Kinetics; 2002:40, 51, 53-55,116, 175, 210-213.
- Andersson GBJ, Chaffin DB, Martin BJ. Occupational Biomechanics. 3rd ed. New York, NY: Wiley; 1999:365-382.
- FitBALL Wedge Ergonomic Cushion. posturedontics.com/fit_sit.php. Accessed February 18, 2011.
Ms. Valachi is a physical therapist, dental ergonomic consultant and CEO of Posturedontics, a company that provides research-based dental ergonomic education. She is a clinical instructor of ergonomics at OHSU School of Dentistry in Portland, Ore, and she lectures internationally at dental meetings, schools, and study clubs. She covers the above topics and much more in her book, Practice Dentistry Pain-Free: Evidence-based Strategies to Prevent Pain and Extend Your Career. She can be reached at (503) 291-5121, posturedontics.com, or via e-mail at bethany@posturedontics.com.
Disclosure: Ms. Valachi reports no disclosures.












