What if you had technology that could reduce your patients’ pain, improve their wound healing, relieve muscle tension, and regenerate nerves, all without pharmaceuticals or side effects? Although it may sound unbelievable, such a tool does exist!
Photobiomodulation (PBM) has been used clinically since 1967, when Endre Mester of Hungary published his first articles on the topic. Historically, other terms have been used to describe these PBM devices, including low-level lasers, soft lasers, and cold lasers.
The term photobiomodulation is derived from:
- Photo: Light from either a laser or LED
- Bio: Eliciting a biological response
- Modulation: Response to the light energy, resulting in either stimulation or inhibition
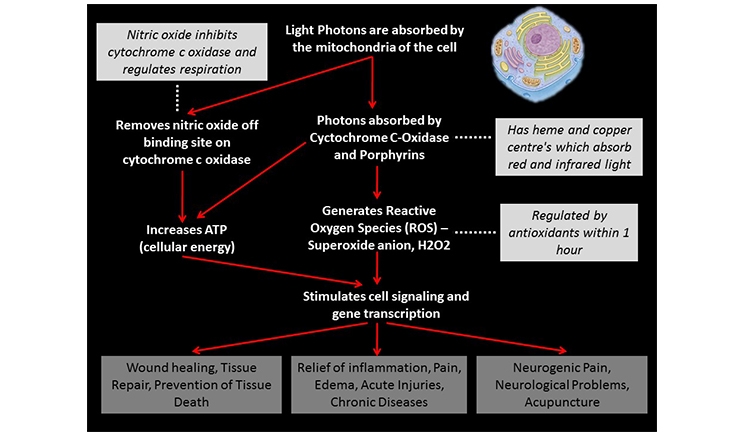
PBM is the use of light energy from lasers or LEDs to elicit cellular and biological responses in the body. Light photons act on several cell processes to stimulate the release of cellular energy (in the form of adenosine triphosphate, or ATP), which can be used to facilitate the restoration of normal cell morphology and function (Figure 1).
 |
|
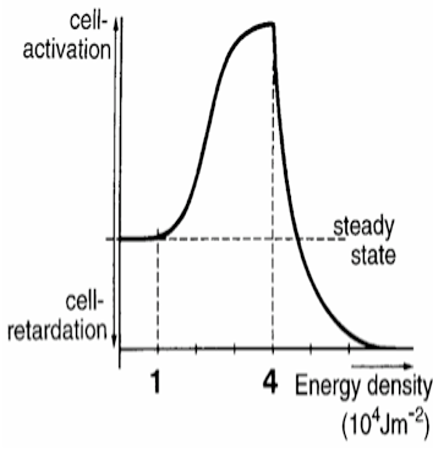
Figure 2. The biphasic dose response means that a low dose of light energy will result in cellular stimulation (eg, stimulation of fibroblasts for improved tissue healing), whereas a higher dose of light energy results in a cellular inhibition (eg, reduction of inflammatory chemicals). |
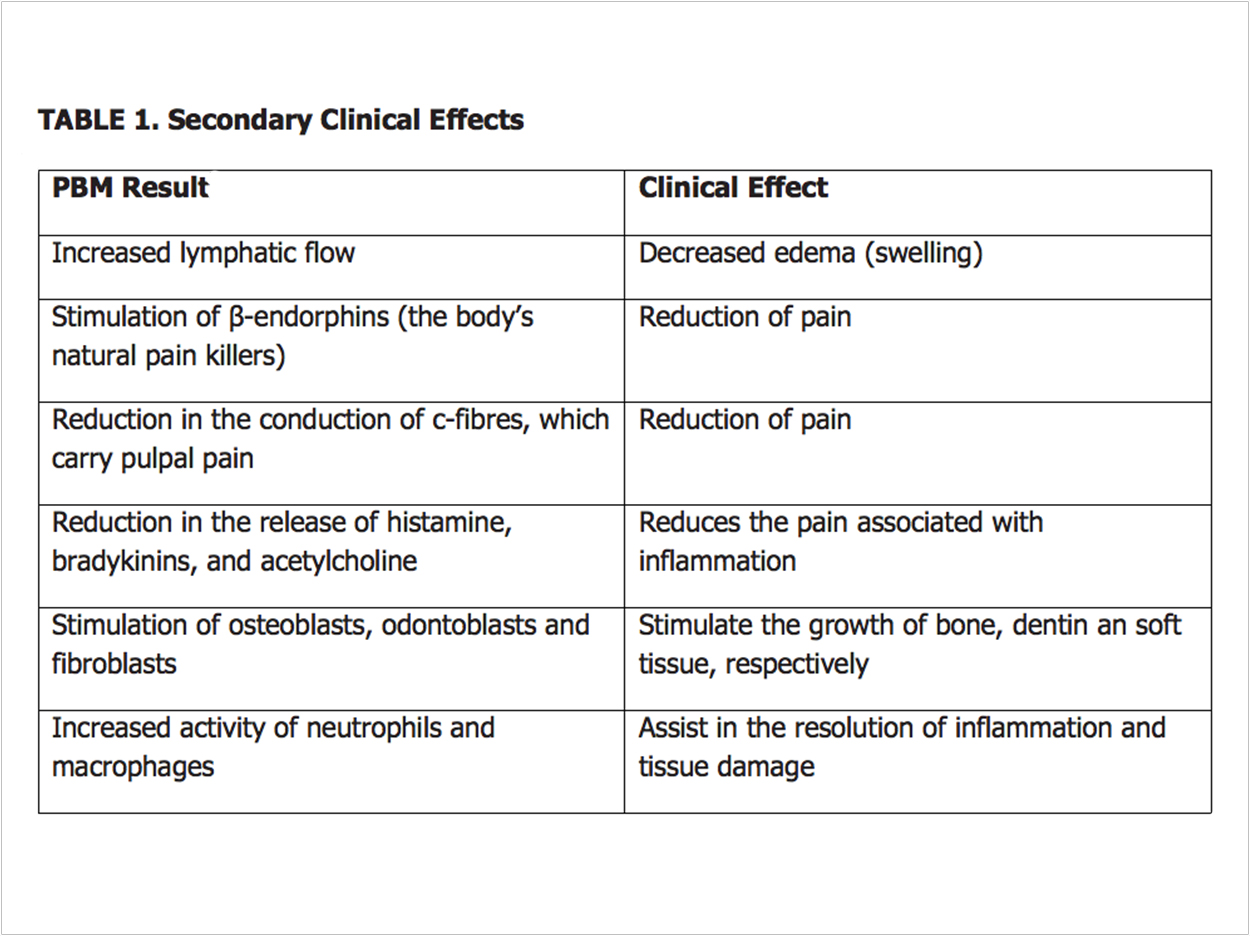 |
The cellular response from cells, which follows the Arndt-Schultz law, is called the biphasic dose response.1 From a clinical standpoint, the biphasic dose response means that a low dose of light energy will result in cellular stimulation (eg, stimulation of fibroblasts for improved tissue healing), whereas a higher dose of light energy results in a cellular inhibition (eg, reduction of inflammatory chemicals) (Figure 2). This additional cellular energy is also available to power many secondary side effects (table).
PBM in Dentistry
Most dentists think of hard-tissue or soft-tissue lasers that are used to cut enamel or soft tissue when they hear the word laser. Though many dental practitioners know little about them, low-level lasers and LEDs also can be invaluable tools.
In fact, almost every aspect of a dental practice can benefit from PBM, whether it’s a general dental or a dental specialty practice. Applications include stimulation of endorphins; reduction in the conduction of nerve fibers that carry pulpal pain (C-fibers); stimulation of fibroblasts, osteoblasts, and odontoblasts (which create soft tissue, bone, and dentin, respectively); and increased circulation and lymphatic drainage. All of these uses can help improve clinical outcomes and decrease patient pain after treatment.
Post-Surgical Benefit: Pain Reduction
Pain, swelling, bruising, and inflammation after an extraction all can be significantly reduced with laser irradiation, reducing or eliminating the need for post-operative analgesics.2 Clinically, the use of PBM allows difficult surgical extractions to be performed without the need for post-operative narcotic analgesic prescriptions. This can have a large societal impact due to the growing epidemic of opioid addiction. The healing of the extraction site also is accelerated, primarily due to the stimulation of fibroblasts.
Case Study
Recently, I saw a patient who needed multiple extractions for a mandibular denture. In addition, he had two large mandibular tori (2 cm long and 1 cm out into the tongue space). With tori this large, it would be impossible for him to wear a full denture.
There were nine teeth to be extracted. Unfortunately, one of the roots of a molar had fractured, so it was necessary to remove bone interproximally and mesially so the root tip could be elevated out.
Large bilateral flaps were made so the tori could be exposed. A surgical bur was used to cut two thirds of the way through the tori, which were then fractured off with an elevator. A bone file was used to smooth the lingual surface of the mandible, and the flaps were then sutured.
Before suturing, the low-level laser was placed in the socket and an inhibitory dose of 8J/cm2 was given to each tooth (Figure 3). Also, 8J/cm2 was applied to the lingual of the mandible where the tori were removed.
I used an 808-nm, 250-mw laser with a 1-cm diameter tip size. Under normal circumstances, I would have expected the patient to experience severe pain and would have prescribed 25-mg Percocet tablets immediately with one every four to six hours.
Today, I do not use any opioids thanks to PBM, so I prescribed 10 mg of Toradol. I told the patient to take one when he got home and every four to six hours as needed. I also warned him about possible swelling and bruising.
I called him the next day to follow up. After taking the one Toradol, he did not need to take any more and said he was not in pain. I addition, there was no swelling or bruising. When I removed the sutures the following week, the healing was excellent, and the flaps were fully closed.
An article by Kahramanet et al in the peer-reviewed journal Photomedicine and Laser Surgery compared applying the laser energy extra-orally and intra-orally to a placebo. The intra-oral placement was superior to extra-oral, but both were better than a placebo.2
Other Dental Applications
There are many other applications of PBM in a dental office:
- Creating analgesia in teeth so more restorations can be completed without the need for needles3
- Prevention of nausea and gagging using the P6 acupuncture point4
- Treatment of soft-tissue lesions, cold sores, aphthous ulcers, and denture sores5
- Better bone healing for better and faster healing in implants and bone grafts6
- Prevention and treatment of mucositis, a common side effect of chemotherapy7
- Nerve regeneration8
- Treatment of facial pain, temporomandibular joint problems, neuropathic pain, and neuralgias.9,10
Is PBM Safe?
In several thousand studies done on photobiomodulation, no clinical side effects have been reported. Photobiomodulation merely restores ATP levels in the mitochondria to normal levels, so it is the cellular response that is delivering a clinical result.
Where Can I Learn More?
- Journals: The two leading PBM journals are Photomedicine and Laser Surgery and Lasers in Medical Science. Both are evidence-based, peer-reviewed journals that are a tremendous resource for any practitioners utilizing, or thinking of including, PBM in their practices.
- Textbooks: Two of the best PBM textbooks are Handbook of Low-Level Laser Therapy9 and The New Laser Therapy Handbook.10
- Organizations: The World Association of Laser Therapy, North American Association for Photobiomodulation Therapy, and Academy of Laser Dentistry all have extensive PBM tracks at their meetings.
Conclusion
A huge benefit of PBM is that patients see their dental practitioner doing something extra to reduce the pain or discomfort that may have been caused during the appointment. The very nature of what dentists do causes pain and inflammation.
PBM requires a paradigm shift. Instead of using drugs to treat the pain after it has started, a dentist now can treat the pain immediately and without the use of narcotics in the dental office and, in many cases, mitigate the pain before the patient feels it.
In an aging population that often relies on multiple medications, this is a huge positive result. PBM is an effective alternate or adjunctive tool to achieve improved clinical effects. It is a benefit to the dental practitioner and patient to investigate PBM, an untapped and underutilized resource in the dental industry.
Disclosure
Dr. Ross lectures and teaches training courses for Zolartek, which produces surgical/low-level lasers. A fee is paid for conducting these courses. However, Dr. Ross has no financial interest in the company. Dr. Ross also contributes to the development of training manuals and instructional videos for MedX Health, which produces several PBM devices. A fee is paid for these activities. However, Dr. Ross has no financial interest in the company. Neither Zolartek nor MedX Health has remunerated Dr. Ross for writing this article.
References
- Huang YY, Chen AC, Carroll JD, et al. Biphasic dose response in low level light therapy. Dose Response. 2009;7:358-383.
- Kahraman SA, Cetiner S, Strauss RA. The effects of transcutaneous and intraoral low-level laser therapy after extraction of lower third molars: a randomized single blind, placebo controlled dual-center study. Photomed Laser Surg. 2017;35:401-407.
- Chow R, Armati P, Laakso EL, et al. Inhibitory effects of laser irradiation on peripheral mammalian nerves and relevance to analgesic effects: a systematic review. Photomed Laser Surg. 2011;29:365-381.
- Ezzo J, Streitberger K, Schneider A. Cochrane systematic reviews examine P6 acupuncture-point stimulation for nausea and vomiting. J Altern Complement Med. 2006;12:489-495.
- Almeida-Lopes L, Lopes A, Tunér J, et al. Infrared diode laser therapy-induced lymphatic drainage for inflammation in the head and neck. Laser Ther. 2005;14:67-74.
- Zein R, Selting W, Benedicenti S. Effect of low-level laser therapy on bone regeneration during osseointegration and bone graft. Photomed Laser Surg. 2017;35:649-658.
- Yoshida K. Current considerations for low-level laser therapy/photobiomodulation therapy in the management of side effects of chemoradiation therapy for cancer. Photomed Laser Surg. 2017;35:457-458.
- Guarini D, Gracia B, Ramírez-Lobos V, et al. Laser biophotomodulation in patients with neurosensory disturbance of the inferior alveolar nerve after sagittal split ramus osteotomy: a 2-year follow-up study. Photomed Laser Surg. 2018;36:3-9.
- Hamblin MR, Pires de Sousa MV, Agrawal T, eds. Handbook of Low-Level Laser Therapy. Singapore: Pan Stanford Publishing; 2017.
- Tunér J, Hode L. The New Laser Therapy Handbook. Coeymans Hollow, NY: Prima Books; 2010.
Dr. Ross has been practicing general practice dentistry with a special interest in facial pain in Tottenham, Ontario, since 1971 and has been using lasers in his practice since 1992. He has given over 200 courses and lectures on the subject both nationally and internationally and has published 15 articles. He has written chapters for two textbooks and is a peer reviewer for four laser journals. He holds Advanced Certification and is a Certified Course Provider from the Academy of Laser Dentistry (ALD) and has fellowship status in the American Society of Laser Medicine and Surgery. In 2016, he received the Leon Goldman Award from ALD as that year’s outstanding laser clinician. Contact Dr. Ross at ddsross@rogers.com.
Related Articles
Researcher Uses Lasers to Regenerate Dental Tissue
Commemorating 25 Years of Lightwave Innovation
Laser Dentistry Requires Bright Practice Management











