The role of attached keratinized gingiva (AKG) around a healthy dental implant cannot be overemphasized. AKG forms an important seal between the oral cavity and the integrated dental implant beneath the soft-tissue junction. It also contributes to thickness and robustness of the peri-implant soft tissue which, in turn, contributes to blood flow and immune support in the crucial soft- and hard-tissue interface. More recent evidence reminds us that the thickness and quality of the peri-implant tissue are much more important factors that influence preservation of crestal bone around the dental implant than known previously.
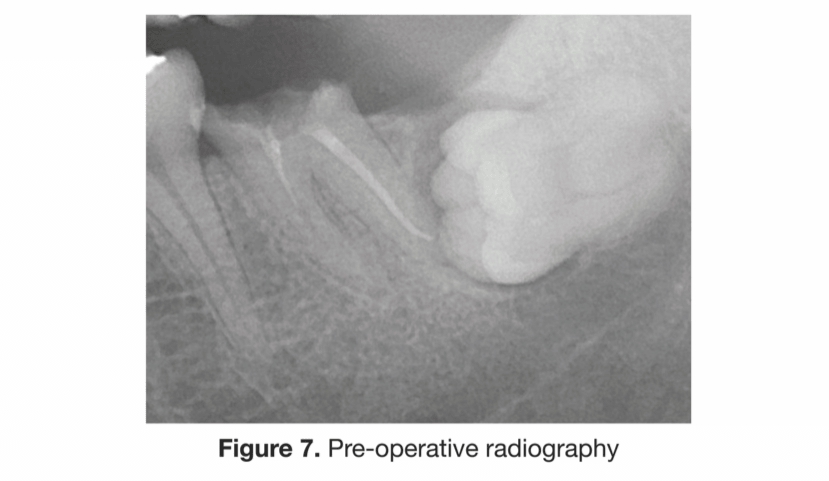
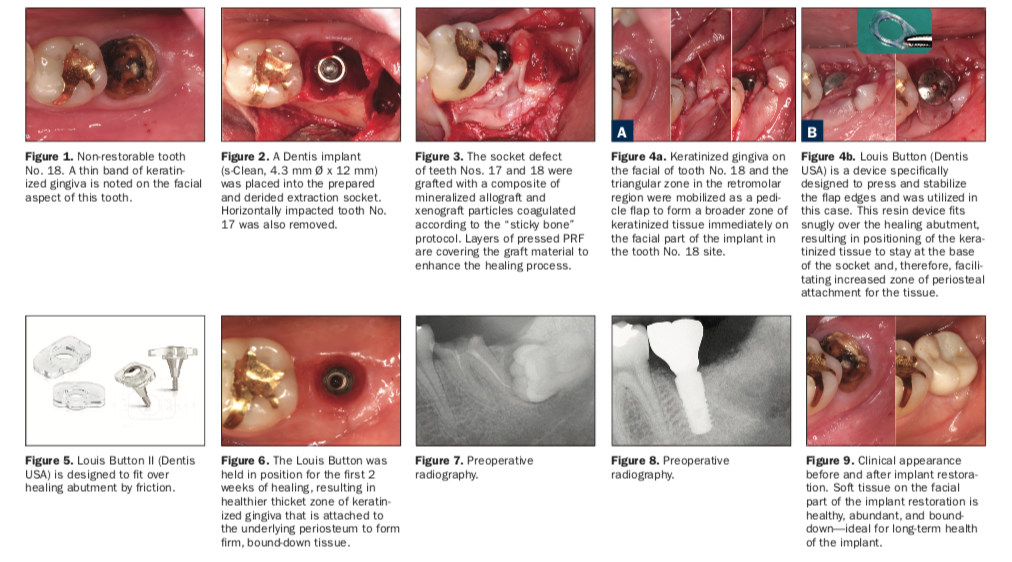
This case illustrates a surgical technique and use of a novel device in aiding the flap management around an immediate implant placement situation. The patient is a 41-year-old healthy male who presented with a non-restorable tooth No. 18.
A horizontally impacted tooth No. 17 was in the vicinity and was surgically removed. A conical connection dental implant (s-Clean [Dentis USA]) was placed in a one-stage surgical protocol concurrently with removal of teeth Nos. 17 and 18. The extraction socket defects were grafted utilizing “sticky bone” consisting of a composite of mineralized allograft and xenograft coagulated by autologous fibrin glue (Figure 5). The graft was enhanced with layers of pressed autologous platelet-rich fibrin (PRF), which accelerated the healing response and acts as a quasi barrier membrane. PRF tends to promote enhanced soft-tissue healing and tends to regenerate more voluminous soft tissue.
A small band of AKT on the facial aspect of tooth No. 18 was preserved and allowed to be pressed to be stable during the healing period. The triangular zone of AKT in the retromolar area distal to tooth No. 18 was mobilized and repositioned to the facial aspect of that tooth. A pre-formed resin structure Louis Button (Dentis USA), designed to adapt to facial soft tissue, was fixated to the healing abutment used in the surgery. The resin device fits over the healing abutment by friction and is removed after initial healing in approximately 14 days. Although this device makes suturing simple, suturing is necessary in many cases, as illustrated in this case, where complex repositioning of the keratinized gingiva was attempted.
REFERENCES
1. Sohn D, Huang B, Kim J, et al. Utilization of autologous concentrated growth factors (CGF) enriched bone graft matrix (Sticky bone) and (CGF) enriched fibrin membrane in Implant Dentistry. J. Implant Adv. Clin. Dent. 2015, 7, 11–18.
2. Linkevicius T, Puisys A, Linkevicius R, et al. The influence of submerged healing abutment or sub-crestal implant placement on soft tissue thickness and crestal bone stability. A 2-year randomized clinical trial. Clin Implant Dent Relat Res. 2020;22:497-506.
3. Berglundh T, Lindhe J, Ericsson I, et al. The soft tissue barrier at implants and teeth. Clin Oral Implants Res. 1991;2(2):81-90.
ABOUT THE AUTHOR
Jin Y. Kim, DDS, MPH, MS, FACD is a board-certified periodontist with practices in Diamond Bar, Calif and Garden Grove, Calif. A graduate of the University of Sydney School of Dentistry and trained in periodontics at UCLA, Dr. Kim has been lecturing on the topics of periodontics, dental implants, and soft-tissue grafting. He holds university positions at several dental schools around the globe and is a founder and co-director of Global Dental Implant Academy (GDIA).
RELATED ARTICLES
Adhesives: An Invaluable Asset for Managing Denture Patients











