For a complete denture to be successful, it should be retentive, stable, and optimally supported by the denture-bearing tissues.1 Despite following the best prosthodontic practices, the presence of certain patient conditions, such as poor quantity and quality of saliva, extensive loss of volume of hard- and soft-tissues, and/or neuromuscular disorders may negatively affect the retention and stability of complete dentures.2-6 A prosthesis that dislodges at rest or during functional movements may lead to dysfunctional oral activities, tissue trauma,7 social embarrassments, and deterioration of the quality of life of the patient.8,9 Several studies have reported an improvement in the retention and stability of the prosthesis and the patient’s masticatory efficiency and force with implant therapy.9-12 Also, implants help maintain the bone dimensions in locations where they are placed.13 However, not all patients are candidates for implant therapy and few patients refuse implants due to financial limitations or fear of invasive surgical procedures.14-17
Denture adhesives have been recommended for improving the retention and stability of the conventional complete denture.18 Owing to the improved retention of the prostheses following adhesive application, the masticatory efficiency and force, load distribution, patient comfort, and confidence are enhanced.19-21 Adhesives augment the seal of the dentures, thereby inhibiting the ingress of food debris underneath the denture, tissue trauma, and malodor.19 They provide a cushioning effect that aids in decreasing the incidence of ulcers, tissue irritation, inflammation, and compression in patients with sensitive tissues/xerostomia.19 Denture adhesives may also be indicated for partial dentures.22 Finite element studies have concluded that adhesives not only help improve the fit between the partial denture and oral mucosa but also enhance the patient comfort.22 Adhesives can also be used to improve the stability and retention of trial denture bases during the jaw relation registration and wax-try-in appointment.23 Adhesives, however, are contraindicated in patients who are allergic to their components, have poorly fitting dentures or poor oral hygiene, and/or need an improvement in the occlusal vertical dimension (due to extensive ridge resorption).23 They should not be used to bond fractured dentures or improve the retention of dentures with lost flanges.23
Most modern adhesives are supplied as a powder, paste, or cream.23 They may be composed of a quick-acting adhesive (sodium carboxymethylcellulose), long-lasting adhesive (poly [methyl vinyl ether/maleic acid] partial calcium zinc salt), thickener (colloidal silicon dioxide), mineral oil/petrolatum (for turning powder into a convenient cream form), antimicrobial agents (hexachlorophene, sodium borate, sodium tetraborate, ethanol), and/or flavoring agents (peppermint).23, 24
Adhesives improve the retention of well-fitting, removable complete dentures by enhancing the interfacial surface tension;25 They augment the adhesive, cohesive, and viscosity of the interfacial surface layer.19, 23, 25 Adhesives swell by 50% to 150% by volume when hydrated, thus they fill the voids and improve the seal between the denture base and the denture-bearing tissues.19 However, it is important to educate the patients regarding the correct amount of usage and the technique for adhesive application and removal.19, 25
Patient Instructions for Adhesive Application
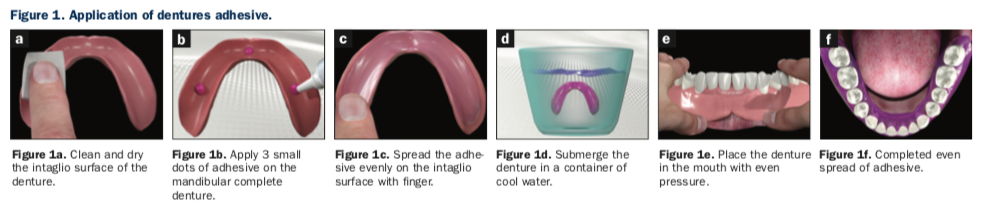
1. Clean and completely dry the intaglio surface of the denture (Figure 1a).
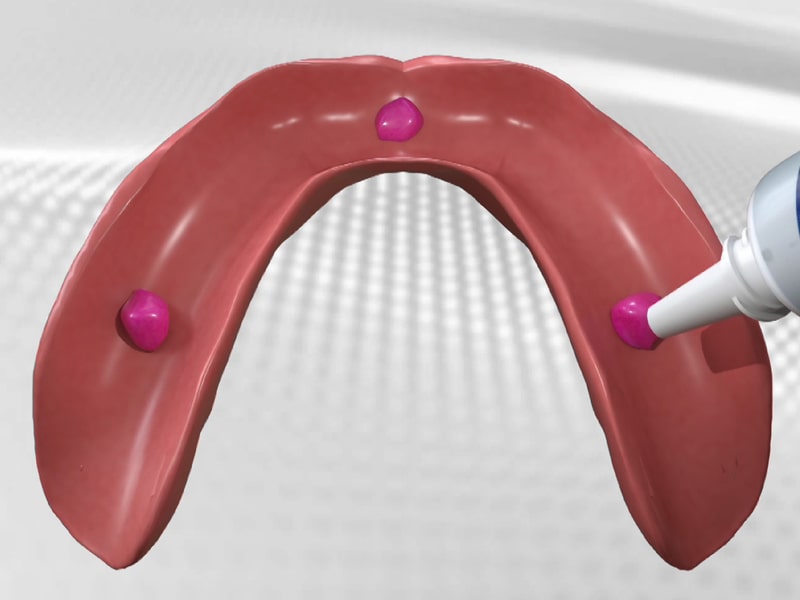
2. Apply 3 small dots of adhesive on the mandibular prosthesis (Figure 1b) and 4 small dots on the maxillary prosthesis.
3. Once dispensed onto the dentures, evenly disperse the paste over the entire intaglio surface of the prosthesis with a clean, dry finger (Figure 1c). This will result in a thin, even layer of adhesive.
4. Submerge the denture in a container of cool water or sprinkle water on the surface to maximally hydrate the adhesive (Figure 1d).
5. Quickly place the denture in the mouth and firmly seat it with finger pressure for approximately 5 seconds (Figure 1e). Maintenance of seating pressure will cause the adhesive to flow throughout the interfacial space between the denture base and the denture-bearing soft tissues (Figure 1f).
6. Inform the patient that the use of excessive adhesive indicates an inadequate fit, necessitating denture reline or remake procedures.
Patient Instructions for Adhesive Removal
It is important to teach patients an effective method for adhesive removal from denture surfaces and oral tissues. Appropriate denture and oral hygiene should be accomplished by edentulous patients at least 2 times each day.
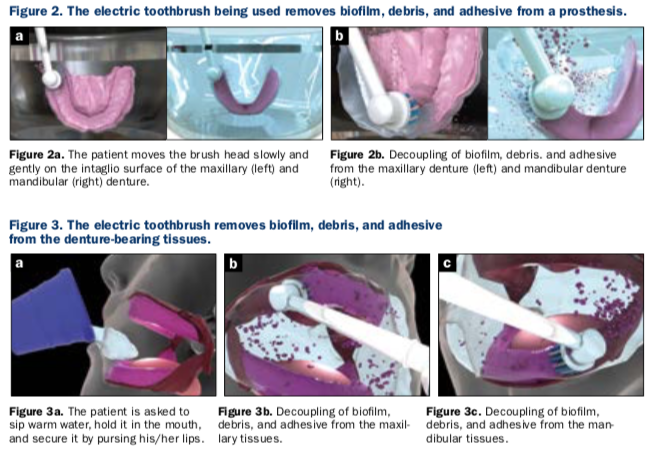
Removing biofilm, debris, and adhesive from the denture:
1. For removing biofilm, debris, and adhesive from the prosthesis, submerge the prosthesis in a container filled with warm water.
2. Place the brush head of an electric brush in the same container and slowly move it on the intaglio surface of the prosthesis (Figure 2a). Both the warm water and the oscillation-rotation-pulsation action of the brush aid in decoupling the biofilm, debris, and adhesive from the prosthesis (Figure 2b).
Removing biofilm, debris, and adhesive from the denture-bearing tissues:
1.Sip warm water, hold it in the mouth, and secure it by pursing lips (Figure 3a). Pursing of the lips prevents the water from dripping out of the oral cavity while inserting the toothbrush into the mouth.
2.Move the brush head slowly and gently on all the denture-bearing tissue surfaces. Both the warm water and the oscillation-rotation-pulsation action of the brush head aid in decoupling the biofilm, debris, and adhesive from the tissues (Figure 3b and 3c). Once all surfaces are clean, expectorate.
Summary
Adhesives play an important role in improving the retention of well-fitting, removable, complete dentures in patients prone to poor retention and their use should not be interpreted as a failure in the denture fabrication process.19 The prescription of conservative and appropriate denture adhesive application can substantially improve prosthesis retention and stability, as well as boost the confidence of the patient. The patients should be kept on a regular maintenance regimen (to keep a check on the amount of usage of the adhesive) and informed that after 5 to 7 years of clinical service the complete dentures may require re-adaptation to the denture-bearing tissues using standard reline or remake procedures.
REFERENCES
1. Patel J, Jablonski R, Morrow L. Complete dentures: an update on clinical assessment and management: part 1. Br Dent J 225, 707-714 (2018).
2. Bogucki ZA. Denture adhesives’ effect on retention of prostheses in patients with xerostomia. Adv Clin Exp Med. 2018 Sep;27(9):1247-1252.
3. Huumonen S, Haikola B, Oikarinen K, et al. Residual ridge resorption, lower denture stability and subjective complaints among edentulous individuals. J Oral Rehabil. 2012 May;39(5):384-90.
4. Saravanakumar P, Thirumalai Thangarajan S, Mani U, et al. Improvised Neutral Zone Technique in a Completely Edentulous Patient with an Atrophic Mandibular Ridge and Neuromuscular Incoordination: A Clinical Tip. Cureus. 2017 Apr 24;9(4):e1189. doi: 10.7759/cureus.1189.
5. Gul M, Ghafoor R, Nazeer MR. Prosthetic rehabilitation of edentulous mandible with two-implant retained fixed hybrid prosthesis: A case report. J Pak Med Assoc. 2018 Dec;68(12):1828-1832.
6. Vere J, Bhakta S, Patel R. Implant-retained overdentures: a review. Dent Update. 2012 Jun;39(5):370-2, 374-5.
7. Emami E, de Grandmont P, Rompré PH, et al. Favoring trauma as an etiological factor in denture stomatitis. J Dent Res. 2008 May;87(5):440-4.
8. Jain P, Rathee M. Stability In Mandibular Denture. 2021 Feb 13. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan.
9. Batisse C, Bonnet G, Bessadet M, et al. Stabilization of mandibular complete dentures by four mini implants: impact on masticatory function. J Dent. 2016 Jul;50:43-50.
10. Sadowsky SJ, Zitzmann NU. Protocols for the maxillary implant overdenture: a systematic review. Int J Oral Maxillofac Implants. 2016;31 Suppl:s182-91.
11. Boven GC, Raghoebar GM, Vissink A, et al. Improving masticatory performance, bite force, nutritional state and patient’s satisfaction with implant overdentures: a systematic review of the literature. J Oral Rehabil. 2015 Mar;42(3):220-33.
12. Turkyilmaz I, Company AM, McGlumphy EA. Should edentulous patients be constrained to removable complete dentures? The use of dental implants to improve the quality of life for edentulous patients. Gerodontology. 2010 Mar;27(1):3-10.
13. Greenstein G, Cavallaro J. Dental implants typically help retain peri-implant vertical bone height: evidence-based analysis. Compend Contin Educ Dent. 2013 Jul-Aug;34(7):502-11; quiz 512.
14. Hwang D, Wang HL. Medical contraindications to implant therapy: part I: absolute contraindications. Implant Dent. 2006 Dec;15(4):353-60.
15. Hwang D, Wang HL. Medical contraindications to implant therapy: Part II: Relative contraindications. Implant Dent. 2007 Mar;16(1):13-23.
16. Kullar AS, Miller CS. Are there contraindications for placing dental implants? Dent Clin North Am. 2019 Jul;63(3):345-362. doi: 10.1016/j.cden.2019.02.004. Epub 2019 Apr 15.
17. Lalabonova CK. Impact Of dental anxiety on the decision to have implant treatment. Folia Med (Plovdiv). 2015 Apr-Jun;57(2):116-21.
18. Grasso JE. Denture adhesives. Dent Clin North Am. 2004 Jul;48(3):721-33, vii.
19. Bartlett D, Carter N, Felton D, et al. White paper on guidelines for the use of denture adhesives and their benefits for oral and general health: Oral Health Foundation; 2019. https://www.dentalhealth.org/Handlers/Download.ashx?IDMF=aa48e389-9c7f-40b1-9d47-ac1dcb599897. Accessed 29 March 2021.
20. Papadiochou S, Emmanouil I, Papadiochos I. Denture adhesives: a systematic review. J Prosthet Dent. 2015 May;113(5):391-397.e2. doi: 10.1016/j.prosdent.2014.11.001. Epub 2015 Mar 4.
21. de Oliveira Junior NM, Rodriguez LS, Mendoza Marin DO, et al. Masticatory performance of complete denture wearers after using two adhesives: a crossover randomized clinical trial. J Prosthet Dent. 2014;112(5):1182–1187.
22. Ramakrishnan AN, Röhrle O, Ludtka C, et al. Finite element evaluation of the effect of adhesive creams on the stress state of dentures and oral mucosa. Appl Bionics Biomech. 2021;2021:5533770.
23. Kumar PR, Shajahan PA, Mathew J, et al. Denture adhesives in prosthodontics: an overview. J Int Oral Health. 2015;7(Suppl 1):93-95.
24. Apostolov N, Todorov R, Yordanov B, et al. Denture adhesives – implementation and advantages. J of IMAB. 2020 Apr-Jun;26(2):3177-3182.
25. Massad JJ, Cagna DR. Prosthesis retention and effective use of denture adhesive in complete denture therapy. dentalcare.com. Accessed 04.13.21.
ABOUT THE AUTHORS
Dr. Massad is an associate professor in the department of graduate prosthodontics at the University of Tennessee Health Science Center (UTHSC) College of Dentistry in Memphis; a clinical professor at the University of Oklahoma College of Dentistry in Oklahoma City; an associate faculty at the Tufts University School of Dental Medicine in Boston; an adjunct associate faculty of the department of comprehensive dentistry at the University of Texas Health Science Center at San Antonio (UT Health San Antonio) School of Dentistry; and an adjunct professor in the department of restorative dentistry at Loma Linda University in Loma Linda, Calif. He has a private practice in Tulsa, Okla. He can be reached at joe@joemassad.com.
Dr. Garcia is dean and a professor at the University of Nevada, Las Vegas School of Dental Medicine. She was in private practice in Denver early in her career, then served as department chair of restorative dentistry at the University of Colorado Health Sciences Center School of Dentistry, as the department chair of prosthodontics at UT Health San Antonio, and as professor and associate dean for education at the University of Iowa College of Dentistry. She can be reached at lily.t.garcia@unlv.edu.
Dr. Ahuja worked at the UTHSC in Memphis as an assistant professor in department of prosthodontics for 3 and a half years. She has lectured nationally and internationally on various prosthodontic topics at various dental conferences. She has more than 50 publications in peer-reviewed national and international journals and is also the co-author of the textbook Applications of the Neutral Zone in Prosthodontics. She is a consultant scientific writer and a consulting prosthodontist for several private dental clinics in Mumbai, India, and also for NYU Langone Medical Center in New York. She can be reached via email at swatiahuja@gmail.com.
RELATED ARTICLES
Everyday Direct Composites in a New Technological Era
Using the Penguin RFA Implant Stability Monitor
Icon Smooth Surface: Minimally Invasive Treatment With Maximal Results











