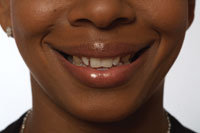
For many years, an association between denture wear and denture stomatitis (eg, denture sore mouth) has been recognized.1-4 Most of the studies suggested that the etiology of the lesion was a yeast infection associated with Candida albicans. In the early 1980s, denture patients presenting with stomatitis (burning mucosa, erythema, and clinical leukoplakia) were evaluated in part by obtaining cultures of both the inflamed mucosa and the dentures (Figure 1). While many of these patients and their dentures were positive for Candida spp., other microorganisms were also present. When the patients were treated with appropriate antimycotic and antibiotic agents, the symptoms and clinical manifestations resolved. When the antimycotic and antibiotic treatment was terminated, the patients’ symptoms and/or clinical manifestations reappeared with positive cultures again for the same microorganisms. The result of these initial clinical observations prompted a series of in vitro and in vivo studies concerning the role of denture contamination in denture stomatitis.
 |
| Figure 1. A typical example of denture stomatitis. The mucosa of this patient was cultured and found positive for Candida glabrata. |
DENTURE STUDIES
A series of in vitro experiments were conducted using strips of methyl-methacrylate that were approximately the same thickness as a standard complete denture, partial denture saddle, or occlusal splint.5 Each strip was processed in the same manner as a complete denture (8 hours of curing under heat and pressure). The denture strips were immersed in media containing known concentrations of C. albicans for 24 hours and subsequently cultured. All denture strip surfaces were found to be positive for C. albicans. Using aseptic technique, the denture strips were fractured and the internal surfaces cultured. The internal aspect of the strips was also found to be positive for C. albicans. While these were in vitro studies that lacked the hydraulic forces associated with a denture in function, they demonstrated that not only did the surface of the denture become contaminated, but the depths or subsurfaces of the denture material were also infected with C. albicans. Recognizing that porosities are created during the curing of methyl-methacrylate dentures, it was postulated that the cured denture material must be porous. This porosity allowed for attachment of microorganisms with subsequent contamination of the depths of the denture material (Figure 2).
 |
| Figure 2. A scanning electron micrograph of the interspaces of a typical methyl-methacrylate denture. Note the porosities in which microorganisms can attach and proliferate (original magnification: 16,000x). |
| Table. The Microorganisms Isolated From Dentures That Had Been Worn for 12 Days to 48 Years and the Related Diseases the Microorganisms Caused.12 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Once this problem was identified, the length of time needed for contamination was studied. Methyl-methacrylate denture strips were exposed to candida in vitro for various intervals of time. This study determined that after 8 hours of denture strip exposure to candida, the surface and subsurface were contaminated to the point that they could not be disinfected using denture cleansers. A comprehensive review of the problem posed by contaminated dentures and attempts at decontamination was published in 1992.6
Once the denture contamination problem was recognized, studies were performed to determine the best approach to decontaminate the C. albicans-contaminated denture material.7-10 These studies indicated that the available denture cleansers were ineffective at decontaminating the denture strips, and this was particularly true for the porosities. Procedures such as placing the denture strips in mouthwash solutions, cleansing them in a dishwasher, and allowing the denture strips to dry completely were all ineffective at decontamination. Interestingly, microwaving the denture strips was also ineffective; however, microwaving the strips in water for more than 2 minutes and boiling the strips for 8 hours reduced but did not eliminate candida contamination.
When all of the decontamination procedures were compared, the best results were obtained by using a series of pH changes. The denture strips were initially submerged in equal parts of 6% sodium hypochlorite (Clorox, Clorox Company), an enzymatic dishwasher soap (Cascade, Procter & Gamble), and water for 2 hours. The denture strips were removed from the first solution, rinsed in plain water, and soaked in a 1:1 mixture of 5% acetic acid (vinegar) and water for one hour. Again, the denture strips were rinsed in plain water and placed in a 100% sodium bicarbonate (Arm and Hammer baking soda) solution (one-half teaspoon of baking soda to 4 ounces of water) for storage or for at least one hour.9
A few years ago, in vivo studies of denture contamination were performed. Twenty complete maxillary and mandibular dentures that had been worn for periods ranging from 12 days to 48 years were studied.11 The dentures were taken from the patient’s mouth and then carefully transported to the laboratory for analysis. Both the surfaces and the cut edges were cultured (Figure 3). After 24 hours of growth, the predominating microorganisms were identified. While some microorganisms cultured were Gram positive, Gram negative microorganisms were also found, including those that are associated with bacterial endocarditis, upper respiratory tract infections, wound infections, meningitis, and gastrointestinal infections (Table).12
 |
| Figure 3. Four Sabouraud Dextrose agar microbiological plates demonstrate the microbial colonization of a typical denture that had been worn for several years. The 3 patterns on the left of each plate are touches of the denture surface, while the 3 “u-shaped” patterns on the right side of the plates are touches of the cut surfaces. Note that repeated treatment of the dentures with water did not substantially change the microorganism pattern, indicating that soaking the dentures in water had no antimicrobial effect. |
These same denture fragments were treated by drying and subsequently freezing for 1.5 years at -80°C. When the fragments were thawed and cultured, Bacillus cereus and Clostridium perfringens, both of which are known spore-formers, were the predominant organisms.12 B. cereus has 2 exotoxins associated with gastrointestinal symptoms (nausea, vomiting, and diarrhea). C. perfringens is a primary pathogen involved in wound infections and gangrene.12
Using the same dentures studied above, a decontamination study was performed.13 Denture fragments were placed into sterile water, sterile water plus a single tablet of a commercially available denture cleanser (Double Action Polident Overnight Denture Cleaner with Polishield, GlaxoSmithKline—active ingredients proprietary), or sterile water containing an experimental denture cleanser (MicroDent Sanitizing and Cleaning System—active ingredients proprietary) that was subsequently microwaved for 2 minutes. Sterile water alone had no effect on the survival of bacteria. The use of sterile water containing a single tablet of a commercially available denture cleanser had little or no effect on the number or species of microorganisms. However, the combination of the experimental denture cleanser with microwaving for 2 minutes produced either a marked decrease in the number of microorganisms or complete sanitization (no bacterial growth on the media). Use of the experimental denture cleanser alone (without microwaving) was no more effective at denture sanitization than the commercially available cleanser.
Additional studies with the commercially available denture cleanser (Double Action Polident Overnight Denture Cleaner with Polishield—active ingredients proprietary), with and without microwaving, revealed that when the dentures were immersed in sterile water containing the cleanser and subsequently microwaved for 2 minutes, effective sanitization was achieved.14 Again, the commercially available denture cleanser alone had little effect on denture sanitization. The data suggested that microwaving drives the disinfecting chemicals into the porosities where the microorganisms are sequestered and is responsible for the sanitization effects. While this study did not consider whether microwaving disrupts the bacteria, microwaving in water alone did not have the same effect on decreasing the numbers of bacterial colonies. The results supported the concept that the basic ingredients of the denture cleaners were being forced by the action of the microwaves into the denture interspaces, where the chemicals could inhibit growth or kill the microorganisms.
Microwaving cannot be used if the appliances contain any metal. When metal is present (ie, partial dentures), microwave arcing will occur with dimensional failure of the denture material.7 For the studies noted above, no detectable changes in the integrity of the denture material were found. Similarly, studies of repeated microwaving of dentures did not reveal any detectable changes in the integrity and dimensional stability of the denture.
Recently, an in vitro study was performed on a denture-sanitizing product from Liechtenstein (Medical Tablets, Bonyf AG, Heiligkreuz 16Fl-9490 Vaduz—active ingredients proprietary).15 The European-made dentures supplied by the company requesting the study appeared to be more difficult to contaminate with the test microorganisms (Staphylococcus aureus, Pseudomonas aeruginosa, B. cereus, C. albicans, and herpes simplex virus 1) than previous in vitro studies. Ultrastructural examination of the European denture material appeared similar to that seen in previous studies of domestic dentures, with both materials having substantial porosity (both product name and material were unknown, except they were defined as methyl-methacrylate). The difference between the 2 materials was there were no synthetic fibers that simulate vessels (personalizing fibers) in the European denture material. It was postulated that these fibers, found in most domestic dentures, may act as pathways for contamination. The study demonstrated that the European denture cleanser (without microwaving) completely eliminated C. albicans and herpes simplex virus 1 from the dentures and reduced the numbers of S. aureus and P. aeruginosa. B. cereus was not substantially affected by the European denture cleanser, probably due to the ability of B. cereus to produce protective endospores. Also, this study was the first to recognize that dentures could be contaminated with virus.
ADDITIONAL STUDIES
Two additional studies suggest the importance of the systemic impact of denture wear. Appollonio and coworkers looked at the relationship between dental status, quality-of-life profiles, and mortality rates in a 10-year prospective study of an isolated village in northern Italy.16 This study of 1,137 individuals (25.2% dentate, 14.3% edentulous without dentures, and 60.4% edentulous with dentures) used univariate analysis and found that the dentate and edentulous with dentures subjects had better quality of life and self-image than those who were edentulous without dentures. However, using a multiple logistic regression analysis, the study found that the mortality rates of the dentate subjects were less than the edentulous without dentures, but the edentulous with dentures had the highest mortality rate. These investigators attributed the increased mortality rate of the edentulous with dentures to poor nutrition. A corollary prospective study of 611 older adults by Locker et al found that poorly perceived oral health, poor psychological well-being, and lower levels of life satisfaction coexisted as a unique subgroup. These negative findings were accentuated in denture wearers.17
CONCLUSIONS
Based on the data cited above, several recommendations for denture care can be made. First, it is important to recognize that methyl-methacrylate dental appliances (dentures, partial dentures, and splints) are porous and contaminate rapidly (within 8 hours of exposure) with microorganisms from the mouth and from the environment. Because these dental appliances are bathed in both residual food and water, microbial proliferation would be expected. These microorganisms may be responsible for not only dental diseases, but also for systemic diseases.12
Routine soaking of the dentures in Double Action Polident Overnight Denture Cleaner with Polishield alone does not substantially reduce this microbial contamination.12 However, for complete dentures without metal, microwaving the dentures for 2 minutes in Double Action Polident Overnight Denture Cleaner with Polishield does substantially reduce the number of microorganisms on and in contaminated dentures.13 For dentures constructed with metal, the best hygienic method appears to be soaking the appliances in a strong base/surface-tension breaker solution for 2 hours, followed by neutralizing the base with a weak acid solution for one hour, followed by storing the dentures in a weak basic solution. For patients with obvious clinical changes in their mucosa, daily sanitization procedures are recommended. For those patients who have normal appearing mucosa, clinical experience has found that sanitization procedures 3 to 4 times per week is sufficient.
References
1. Cahn LR. The denture sore mouth. Ann Dent. 1936;3:33-36.
2. Neill DJ. Symposium on denture sore mouth. I. An aetiological review. Dent Pract Dent Rec. 1965;16:135-138.
3. Cawson RA. Symposium on denture sore mouth. II. The role of Candida. Dent Pract Dent Rec. 1965;16:138-142.
4. Lehner T. Symposium on denture sore mouth. 3. Immunofluorescent investigation of Candida. Dent Pract Dent Rec. 1965;16:142-146.
5. Wendt S, Glass RT. The infected denture: how long does it take? Quintessence Int. 1987;18:855-858.
6. Glass RT. The infected toothbrush, the infected denture, and transmission of disease: a review. Compendium. 1992;13:592-598.
7. Rohrer MD, Bulard RA. Microwave sterilization. J Am Dent Assoc. 1985;110:194-198.
8. Rohrer MD, Bulard RA. Sterilization by microwaves. J Okla Dent Assoc. 1985;75(3):29-31.
9. Wendt S, Glass RT, Glass MC. Decontamination of Candida albicans infected denture material. IADR. Abs 311, p. 151, 1988.
10. Glass RT, Belobraydic KA. Dilemma of denture contamination. J Okla Dent Assoc. 1990;81:30-33.
11. Glass RT, Bullard JW, Hadley CS, et al. Partial spectrum of microorganisms found in dentures and possible disease implications. J Am Osteopath Assoc. 2001;101:92-94.
12. Collier L, Balows A, Sussman M, et al. Topley & Wilson’s Microbiology and Microbial Infections. 9th ed. New York, NY: Oxford University Press; 1998: Vol 2, 3, 4.
13. Glass R, Conrad R, Goodson L, et al. Spectrum of microorganisms found in dentures and a comparison of the effectiveness of several denture-sanitizing systems: a clinical study. Compend Contin Educ Dent. 2001;22:1093-1108.
14. Goodson LB, Glass RT, Bullard JW, et al. A statistical comparison of denture sanitation using a commercially available denture cleaner with and without microwaving. Gen Dent. 2003;51:148-151.
15. Glass RT, Bullard JW, Conrad RS, et al. Evaluation of the sanitization effectiveness of a denture-cleaning product on dentures contaminated with known microbial flora. An in vitro study. Quintessence Int. 2004;35:194-199.
16. Appollonio I, Carabellese C, Frattola A, et al. Dental status, quality of life, and mortality in an older community population: a multivariate approach. J Am Geriatr Soc. 1997;45:1315-1323.
17. Locker D, Clarke M, Payne B. Self-perceived oral health status, psychological well-being, and life satisfaction in an older adult population. J Dent Res. 2000;79:970-975.
Dr. Glass is a professor of forensic sciences, pathology, and dental medicine; adjunct professor of microbiology; chairman, department of forensic sciences; and director of the Forensic Sciences Graduate Program at Oklahoma State University Center for Health Sciences. He can be reached at (918) 561-8240 or glassrt@chs.okstate.edu.