|
|
Five to 10 percent of patients with asthma have disease that can be classified as severe, meaning it is difficult to treat and often causes life-threatening breathing problems. |
Five to 10 percent of patients with asthma have disease that can be classified as severe, meaning it is difficult to treat and often causes life-threatening breathing problems. Typically these patients are treated with the aim of reducing lung inflammation, but treatment often leads to devastating consequences due to steroid side effects.
As reported in the American Journal of Respiratory and Critical Care Medicine, researchers dubbed the condition “asthmatic granulomatosis” after the characteristic small areas of focal inflammation that can be found in the lungs of those who have it.
“We’re now learning that all severe asthma is not the same, but is in fact the result of different problems,” said Sally E. Wenzel, professor, division of pulmonary, allergy, and critical care medicine at the University of Pittsburgh School of Medicine. “If we better understand the underlying mechanisms that are causing the symptoms, we can offer better treatments.”
For the study, the team examined a group of patients with severe asthma who were being treated at the Difficult Asthma Clinic at the Comprehensive Lung Center of UPMC during a four-year period. Each of the patients met with a certified asthma educator; were taking high doses of inhaled steroids, with or without ingested steroids; and had been monitored for three to 24 months to optimize therapy.
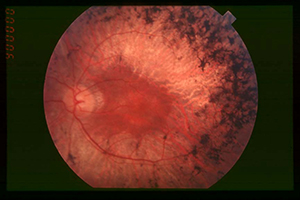
Nineteen patients then underwent biopsies of their lung tissue using a video-assisted, fiberoptic scope. Ten of them not only had airway changes typical of asthma, but also lesions called granulomas, which are nodules of inflammation sometimes seen with certain infections or with autoimmune diseases. None of the patients had a history of hypersensitivity pneumonitis, an acute illness caused by inhalation of foreign particles such as dust, molds, and fungi, which can also lead to granuloma formation.
However, 70 percent of the patients had a personal or family history of autoimmune-like disease such as lupus and rheumatoid arthritis. Because granulomas can be produced by an overactive immune system, the team treated the 10 cases with drugs that suppress it, including azathioprine, mycophenolic acid, methotrexate or infliximab. Nine of them reduced their steroid doses and had improvements in standard lung-function tests while one has experienced difficulty tolerating the powerful immune-suppressants.
Of the other nine patients who had biopsies, six had tissue changes that reflected asthma, but no granulomas, and three had other issues, including indications of aspiration, pneumonia and small blood clots.
“The unexpected finding of granulomas in a subset of patients with severe asthma warrants approaching it as a newly described disease, which we’ve named asthmatic granulomatosis,” Wenzel said. “It is a condition that has overlapping features of asthma, autoimmunity, and granulomas, and it appears to respond better to immune-suppressants than to high-dose steroid treatment.”
Asthma specialists should consider getting tissue biopsies in atypical severe asthmatics. More research is needed to determine the immunological pathways that contribute to the disease and develop biomarkers that will simplify diagnosis of asthmatic granulomatosis.
“These studies advance our division’s focus on precision, or personalized, medicine—an effort to better refine specific patient diagnoses and tailor more effective therapies,” said Mark T. Gladwin, chief of the Pulmonary, Allergy and Critical Care Medicine Division.
The project was funded by the Dellenback Research Fund.