Probably one of the first things to pop into a dental patient’s head, other than a throbbing toothache, is if the recommended treatment is covered by their insurance. Quality dental care can come at a substantial price, and neglecting treatment is a gamble that’s all risk and no reward.
But dental insurance isn’t always a seamless experience, particularly when the patient requires extensive treatment and their insurance coverage is uncertain. If treatment can’t wait, up-front payment may be the only way to go. And with claims processing taking as long as two to three weeks to complete, who can wait? But if the claim is denied, the patient gets an out-of-pocket expense they may not have prepared for.
Conversely, a patient may choose to wait until approval before moving forward with the procedure. This, however, often results in prolonged waiting periods and delayed treatment that can affect the patient’s quality of life and even result in avoidable pathology progression.
The Role of AI
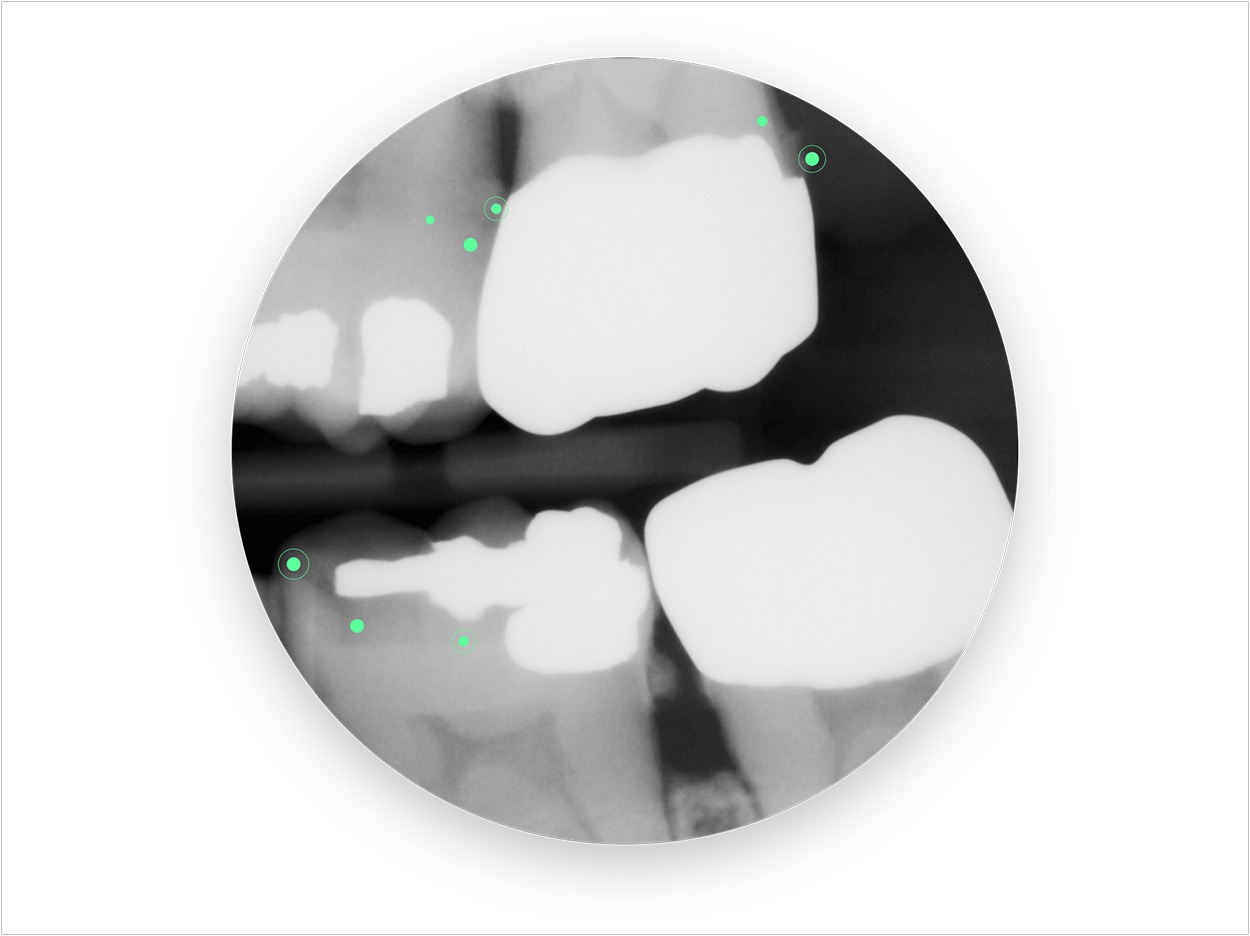
Artificial intelligence (AI) is addressing the gap between patients, providers, and insurers to reduce waiting periods and help process claims faster and more accurately, creating an uninterrupted experience that gives patients access to much needed treatment without the wait.
Traditionally, dental insurance claims include attachments complete with the patient’s information, claim information, and other necessary details about the narrative, procedures, costs, and so on.
Before a claim is submitted, this information must be compiled by the patient or the provider, who is essentially making a case on the patient’s behalf. Submission typically involves some digging around in the practice management system (PMS) and patient history, an assessment, and then presenting the information in the best interests of the patient.
When everything is compiled and submitted to the insurance company, its representatives and dental consultants are tasked with reviewing the contents and determining the medical necessity of the procedure.
Most of these steps are manual processes. Those that aren’t are run through arbitrary math models that do little to factor in legitimate variables, which may leave valid claims behind. As far as the data goes, everything from submission to review is performed by hand, with very little input from databases themselves, other than simply offering manual access to the data.
As such, important decisions have to be made by people based on information compiled by people based on data input from, you guessed it, people. And like so many tedious processes that stand to benefit from automation, insurance claims submission and processing is prone to inefficiency and human error.
With AI, virtually every one of these steps can be automated and performed by algorithms designed to access, identify, and process data with the end goal of providing accurate and valuable output—namely the patient’s qualification for coverage.
One of the most time-consuming hurdles faced by insurance companies during the claims process is determining if the treatment is a medical necessity. With the dental insurance industry beset by cases of overdiagnosis and fraud, human underwriters are the only ones standing in the way between detection and some crook’s big break.
Big Changes Ahead
AI is changing all of that and more. As far as the payer-provider experience goes, AI has the power to revolutionize dental care efficiency by giving patients access to claims pre-authorization and immediate care. Not only can this mean life-changing implications for patients, but it also will result in streamlined financials for clinics, who can churn out happy patients as fast as they come through the door.
Insurance companies also stand to benefit immensely from AI, with optimized fraud detection and automated underwriting processes that could reduce costs and give people time for more valuable tasks, like determining the basis of such algorithms and how to validate every single legitimate claim.
With millions of claims to process every year, a fair system was never really an option in the dental insurance business. But with AI, every claim will be able to get a fair shake while weeding out the bad apples in near real-time.
Insurance companies will also enjoy AI’s customer service capabilities, which eliminate countless manual processes and allow patients to receive personalized, automated service anytime. Before we know it, much of the dental experience may be automated to everyone’s benefit, with insurance companies essential to the financial efficiency of the entire process.
Mr. Hillen is the founder and CEO of VideaHealth, an MIT spinout and leading dental-AI company working with leading DSOs, insurers, and other companies in the dental industry. Previously, he conducted research at the intersection of engineering and social science at MIT’s Institute for Data, Systems and Society and at Harvard Business School. He also worked for McKinsey & Company and founded Ninu, a digital healthtech startup. He holds two master’s degrees from MIT in computer science and technology policy and a bachelor’s in management and technology. He completed the first German State exam in medicine as well. This article is the product of a discussion between Mr. Hillen and Dr. Paul Feuerstein, editor in chief of Dentistry Today.
Related Articles
How Will Artificial Intelligence Affect Dentists?
AI and Dentistry: Envisioning the Dental Clinics of the Future—And Today
Overjet Execs Discuss AI’s Potential to Transform Dentistry












