A torus palatinus (TP) is a benign exostosis of the hard palate along the palatal suture involving the maxilla and palatine processes. A TP can be so large anteroposteriorly that it can reach the edge of the incisive papilla and the posterior border of the hard palate. The torus palatinus has been described as cancellous bone covered by compact bone and coated with a thin layer of mucoperiosteum, from which it receives the major portion of its blood supply.
The incidence of TP varies between 9.2% and 66%.1 Haugen found 9.2% of a population of 5,000 Norwegians had TP.2 Chew and Tan observed that 48% of Chinese patients had TP,3 while Kerdpon and Sirirungrojying found that 61.7% of Thai patients had a torus palatinus. They observed that TP might be related to parafunctional activity.4
Traditional management of a torus palatinus when fabricating a complete denture involves either surgical removal of the torus or construction of a window in the denture to accommodate the torus. Surgical removal is recommended when one or more of the following conditions exist: interference with the construction of a prosthesis, interference with oral function, irritation or pathology of the overlying tissue, inability of the patient to maintain proper oral hygiene, and fear of malignancy or other psychologic trauma.5-7
Nevertheless, surgical removal of the torus may result in the following complications: nasal perforation, oronasal or antral fistula formation, palatal tissue necrosis, and hematoma.8
Valentine described the design of a complete maxillary denture with a large midline window.9 This would be a viable option for management of a small, midline torus. A technique referred to as triple lamination has been described that allows a prosthesis to use a large mandibular torus for retention.10 This technique involves a combination of soft flanges and liner, allowing the denture to engage the soft-tissue undercut without pain or soft-tissue trauma. The denture can also be easily removed. Triple lamination has been adapted to help engage deep, soft-tissue undercuts in the anterior aspect of the maxilla.11
This article describes an adaptation of the triple lamination technique for the placement of a maxillary complete overdenture over a large torus palatinus.
CASE REPORT
A 58-year-old woman presented with a chief complaint that her maxillary cast removable partial denture was loose. The patient had worn a maxillary removable partial denture for more than 23 years. Over the years, there had been many repairs and the addition of denture teeth as natural teeth required extraction. At the present time, very few teeth were strategically placed to assist in the retention of a partial denture. The existing cast cobalt chromium maxillary removable partial denture had been designed with a horseshoe-shaped palate to accommodate a torus palatinus.
 |
 |
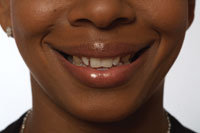
| Figure 1. Initial anterior view. | Figure 2. Initial maxillary right view. |
The patient’s overall oral hygiene was fair to poor. Generalized moderate gingivitis was present with only minimal bone loss. Gingival tissues were erythematous and edematous. The patient was concerned with the appearance of her natural teeth as well as the fit and long-term prognosis of her maxillary partial denture (Figure 1). She requested that all the maxillary teeth be removed and a complete maxillary denture be fabricated (Figure 2). Her maxillary dentition consisted of 4 heavily worn and heavily restored incisors, a right first bicuspid restored with a porcelain-bonded-to-metal crown, and a right second molar with a large, 4-surface amalgam restoration. The maxillary right bicuspid and molar also exhibited extensive caries at the gingival margin, extending almost completely around the crowns of these teeth.
The remaining mandibular dentition consisted of all the anterior teeth, right and left first bicuspids, left second bicuspid, and right second molar. The mandibular right second molar was badly fractured and was scheduled to be extracted upon insertion of the maxillary complete denture. The other mandibular teeth displayed moderate wear and were heavily restored. Specifically, the mandibular anterior teeth were restored with composite resins, and the margins were beginning to deteriorate. The mandibular cuspids were mildly rotated, and there was mild crowding of the incisors. There was a class II molar occlusal relationship with 100% overbite and a 5-mm overjet. The mandibular incisors impinged on the palatal tissues, traumatizing the area and causing some discomfort.
 |
| Figure 3. Palatal view of maxillary torus and posterior teeth. |
The patient had a large, multilobulated torus palatinus (Figure 3). It extended from the area adjacent to the first bicuspids to a point beyond the junction with the soft palate. The torus was oblong in shape, measuring 37.5 mm long, 16 mm wide, and 7 mm in height. It was covered with thin mucosal tissue and did not interfere with speech, chewing, or other oral functions.
A maxillary complete immediate overdenture was considered the treatment of choice. There were a number of issues to consider. The patient had an exaggerated gag reflex that would affect taking impressions and wearing a prosthesis that would cover the palate. Consideration was given to surgical removal of the torus palatinus, since it extended past the vibrating line (the junction of the hard and soft palate). The 4 maxillary incisors could be retained as overdenture abutments, since they had minimal mobility and good periodontal support. Considering the stability of the roots of the maxillary incisor teeth, it was decided to perform root canal therapy, reduce the occlusal height, and restore the remaining tooth structure with a compomer filling material (taking advantage of the material’s fluoride release). This would maintain the deep anterior undercut, which would aid in the retention of the immediate overdenture.
The maxillary bicuspid and molar were extracted. The preliminary and final impressions were made with alginate. To decrease the gag reflex, warm water was used to speed the set of the alginate. A border-molded (with impression compound) acrylic custom tray was used for the final impression. Adequate relief in the tray was provided to allow seating of the impression tray and capturing of the undercuts. The alginate impression material yielded a very good model of the maxillary torus.
Next, occlusal registration and tooth selection were completed. Then a wax occlusion rim was tried in with tooth set-up in the edentulous areas to verify the correct occlusion, shade, and mold. Vitapan (Vident) prosthetic teeth (20° [cuspal inclination] posterior teeth) were used. The patient’s class II occlusion and 5-mm overjet were duplicated in the new denture because of the position of the maxillary ridge.
 |
 |
|
Figure 4. Tissue surface of denture showing the extension of laminated soft materials. |
Figure 5. Tissue surface of denture showing various materials used. Black line indicates the border between Versacryl flange and SR Ivocap High Impact denture base. Blue line indicates the top of the flange. Tissue surface of the denture is lined with MOLLOPLAST-B. |
The triple lamination technique involves laminating 3 materials to form the denture. In the laboratory, SR Ivocap High Impact (Ivoclar Vivadent) injection-molded acrylic resin was used to fabricate the base and buccal flange. A thermoplastic material (Versacryl [Keystone Industries]) was used to fabricate the external portion of the palatal flange. A resilient material, MOLLOPLAST-B (Detax GmbH), was used to line the entire tissue surface of the denture including the palatal flange. This created a tissue surface with a large amount of soft lining material that actively engaged the undercuts in the maxillary torus (Figures 4 and 5). In sum, the bulk of the denture was rigid, with the flanges and tissue surface of the denture having some flexibility to engage the soft-tissue undercuts. The thermoplastic material on the edges of the flange (Figure 5) allowed the flange to engage the labial undercuts.
On the date of insertion, the maxillary incisors were reduced in height and a compomer filling material (Dyract [DENTSPLY Caulk]) was placed over the incisal endodontic access cavities. The maxillary right first bicuspid, maxillary right second molar, and mandibular left second molar were extracted, and the immediate maxillary complete over-denture was inserted. In order to prevent recurrent caries in the retained anterior roots, the patient was told to brush with a toothpaste with a high fluoride content (Prevident 5000 [Colgate Oral Pharmaceuticals]).
 |
 |
|
Figure 6. View of palatal surface of the denture showing soft material that engages undercuts in maxillary torus. Exterior portions of borders of the flanges are supported by Versacryl, providing flexibility so that the flange engages the undercut. |
Figure 7. Facial and right view of denture demonstrating occlusal relationship. |
The patient was seen the next day and was comfortable. All extraction sockets were healing well, and minor adjustments were made to the denture base in the maxillary cuspid regions. Recall appointments the following day and over the next 4 weeks showed no sign of any denture irritation. There were no complaints of irritation of the torus palatinus. Although the palatal aspect of the denture was slightly thicker, the patient did not experience gagging and was able to accommodate quickly to the palatal coverage (Figure 6). The patient immediately noticed that the mandibular incisors did not impinge on the palatal tissues (Figure 7). The patient reported excellent stability and retention; at times, the patient found it very difficult to remove the denture.
At 24 months follow-up the patient was satisfied and had no complaints.
DISCUSSION
The thermoplastic material Versacryl is relatively rigid at body temperature, but tempering in hot water softens the material. Adjustments are accomplished by first chilling the denture before polishing or grinding. It is a methyl-methacrylate and chemically bonds to the denture base and the resilient liner. The result is a semi-rigid flange that slides easily over the torus palatinus and into soft-tissue undercuts in the maxillary anterior area.
Resilient liners such as MOLLOPLAST-B are widely used as a cushion on the fitting surface of dentures in the management of trau-matized oral mucosa, bony undercuts, bruxism, ridge atrophy, and for congenital oral defects requiring obturation.12 Soft lining materials provide an even distribution of the functional load and avoid the concentration of local stress on the soft-tissue surface.13-14 There are 2 main types of resilient liners: (1) plasticized acrylics and (2) silicone elastomers. These materials differ in the percentage of crosslinking agents, catalysts, and fillers, and are available in autopolymerizing and heat-cured forms.15 Silicone-based polymers remain soft or rubbery at or below mouth temperatures.
This triple lamination of materials allowed the denture to fit onto the torus palatinus and engage the anterior undercut. The resilient liner prevented the thermoplastic material from locking around the torus, decreased the occlusal load on the torus, and acted as a shock absorber to distribute the occlusal load across the edentulous ridge. In the case described, this allowed the undercut to act as an active part of the retentive mechanism for the denture. It also reduced the incidence of sore spots and denture irritation (Figure 5). The semi-rigid exterior of the flange provided support and flexibility to allow the denture to engage the anterior undercut.
SUMMARY
A maxillary torus provides a challenge when restoring an edentulous arch. Tori tend to have very thin mucosa and can be intolerant of normal pressures from a denture base. The tori tend to have large undercuts and at times extend to the junction with the soft palate, preventing the creation of a good palatal seal. Triple lamination involves combining 3 materials to fabricate a denture base that utilizes the retentive aspects of the torus. The thermoplastic flange provides a measure of flexibility, allowing the denture to seat over the torus. The resilient liner provides a cushion to diffuse the occlusal load, while the rigid acrylic base provides the support for the denture teeth. Using this approach, a very retentive denture was fabricated using the maxillary torus as a key element in anchoring the prosthesis.
Acknowledgment
The authors would like to acknowledge Ron Klausz of Klausz Dental Laboratories. Dr. Abrams, in consultation with Mr. Klausz, developed the triple lamination technique and the criteria for its utilization.
References
1. Seah YH. Torus palatinus and torus mandibularis: a review of the literature. Aust Dent J. 1995;40:318-321.
2. Haugen LK. Palatine and mandibular tori. A morphologic study in the current Norwegian population. Acta Odontol Scand. 1992;50:65-77.
3. Chew CL, Tan PH. Torus palatinus. A clinical study. Aust Dent J. 1984;29:245-248.
4. Kerdpon D, Sirirungrojying S. A clinical study of oral tori in southern Thailand: prevalence and the relation to parafunctional activity. Eur J Oral Sci. 1999;107:9-13.
5. Rezai RF, Jackson JT, Salamat K. Torus palatinus, an exostosis of unknown etiology: review of the literature. Compend Contin Educ Dent. 1985;6:149-152.
6. Ogle RE. Preprosthetic surgery. Dent Clin North Am. 1977;21:219-236.
7. Blakemore JR, Eller DJ, Tomaro AJ. Maxillary exostoses. Surgical management of an unusual case. Oral Surg Oral Med Oral Pathol. 1975;40:200-204.
8. Costello BJ, Betts NJ, Barber HD, et al. Preprosthetic surgery for the edentulous patients. Dent Clin North Am. 1996;40:19-38.
9. Valentine DC. Conservative management of a pedunculated torus palatinus in an edentulous arch. Gen Dent. 1983;31:202-203.
10. Abrams S. Complete denture covering mandibular tori using three base materials: a case report. J Can Dent Assoc. 2000;66:494-496.
11. Abrams S. A technique for using maxillary anterior soft-tissue undercuts in denture placement: a case report. J Can Dent Assoc. 2002;68:301-304.
12. Baysan A, Parker S, Wright PS. Adhesion and tear energy of a long-term soft lining material activated by microwave energy. J Prosthet Dent. 1998;79:182-187.
13. Wright PS. The success and failure of denture soft-lining materials in clinical use. J Dent. 1984;12:319-327.
14. Bell DH Jr. Clinical evaluation of a resilient denture liner. J Prosthet Dent. 1970;23:394-406.
15. Jagger DC, Harrison A. Complete dentures–the soft option. An update for general dental practice. Br Dent J. 1997;182:313-317.
Dr. Abrams is a partner in a group practice in Scarborough, Ontario. He is a fellow of the Pierre Fauchard Academy and the Academy of Dentistry International. He has published more than 75 articles in various international publications and was recently awarded the Barnabus Day Award from the Ontario Dental Association for 20 years of distinguished service to the dental profession. He can be reached at (416)-265-1400 or dr.abrams4cell@sympatico.ca.
Dr. Hellen graduated from the University of Toronto Faculty of Dentistry in 1980. He is a partner in a group practice in Scarborough, Ontario, and a member of Alpha Omega and the Ontario Dental Association. He can be reached at (416)-265-1400 or wmph@sympatico.ca.