The UCLA Center for Health Policy Research has identified three of the most important factors that have led to disparities in access to dental care in California:
- There are fewer dentists per capita in some parts of the state.
- About 79% of the state’s dentists do not provide care for low-income patients who rely on Medi-Cal.
- Only 8% of the state’s dentists are Latino or Black, compared with 60% of the state’s low-income adult population overall.
Also, a shortage of dentists is looming, according to the researchers. Approximately 23% of dentists are 60 years old or older and nearing retirement age, while only 9% of dentists have graduated from dental school within the past five years.
This imbalance is likely to place additional strain on access to oral healthcare for all Californians, the researchers said, and for lower-income residents in particular.
According to the center’s 2019 California Health Interview Survey, 32% of the state’s residents are adults with incomes under 200% of the federal poverty level.
Additionally, the researchers reported in previous studies that lower-income Californians have poorer oral health and less access to oral healthcare than residents with higher incomes.
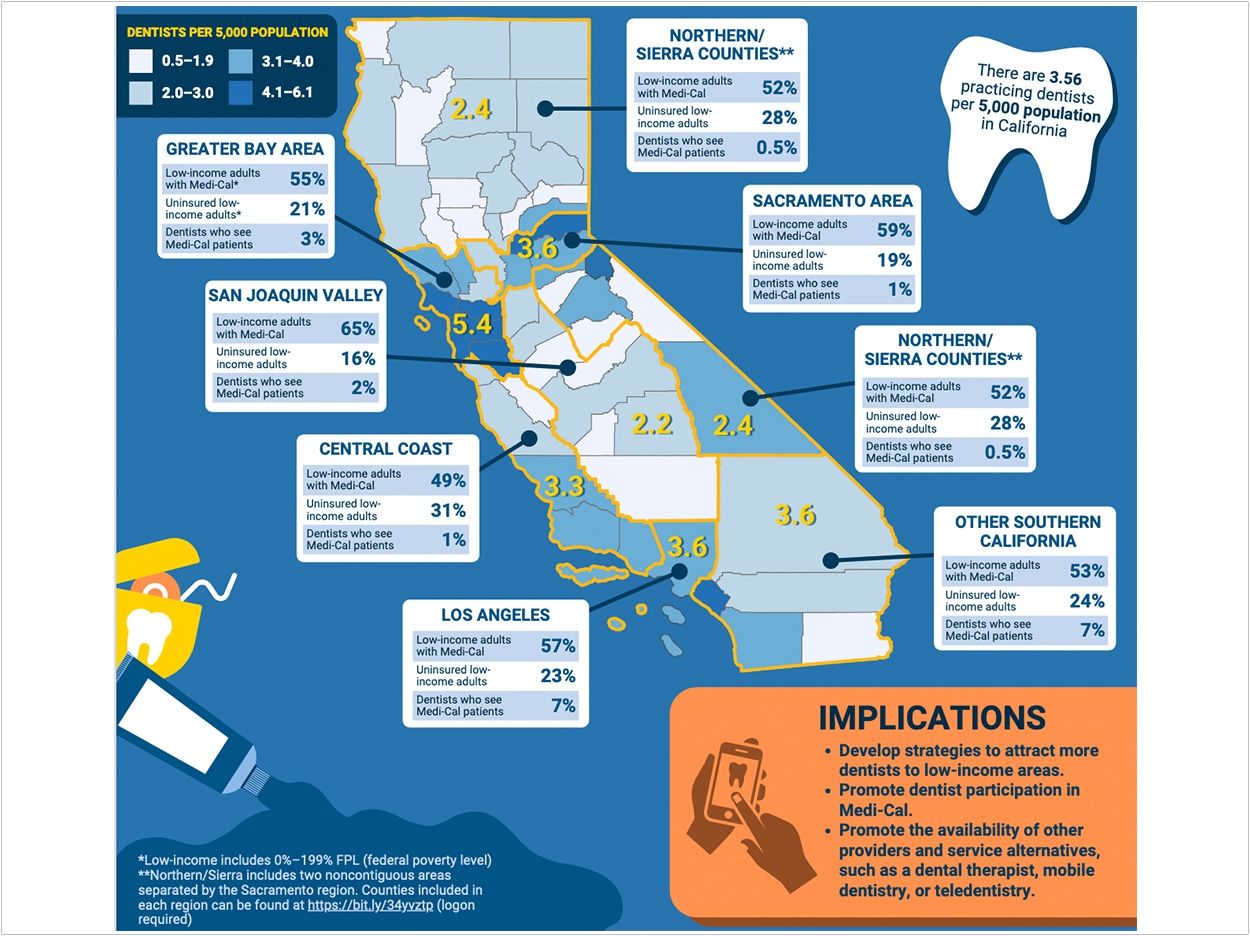
The recent study notes regions where there is a relatively small number of dentists per capita, a large proportion of low-income adults, and a small percentage of dentists who see patients with Medi-Cal.
In San Joaquin County, for example, there are just 2.2 dentists per 5,000 residents. And while 65% of the area’s low-income adults have Medi-Cal, only 2% of dentists see Medi-Cal beneficiaries.
“The availability of dentists willing to provide care to the low-income and uninsured population of California is crucial in ensuring access to oral healthcare and improved oral health status,” said Nadereh Pourat, PhD, the center’s associate director and lead author.
“Our findings indicate regional disparities in where low-income populations live and where California dentists practice. We also found low participation of dentists in Medi-Cal and limited numbers of dentists from communities of color,” Pourat said.
“These factors perpetuate income disparities in both access to oral healthcare and oral health status of low-income Californians,” said Pourat.
The researchers analyzed data from the Dental Board of California, the California Dental Association, and California Health and Human Services. They also found:
- 39% of low-income California adults reported that their oral health was fair or poor.
- 41% of low-income California adults had not visited the dentist in the previous year.
- 23% of the state’s dentists were 60 years old or older.
- Although 53% of the state’s low-income adults were Latino and 7% were Black, only 6% of practicing dentists were Latino, and 2% were Black.
“The data clearly show the importance of increased participation of dentists in Medi-Cal,” Pourat said. “Policy tools to incentivize participation have been used for low-income children and can be tailored for low-income adults.”
The researchers suggest expanding the roles of hygienists and dental therapists to reduce the burden on dentists.
Also, the researchers suggest that dentists use mobile clinics to bring oral healthcare into underserved neighborhoods and offering at least some appointments, particularly for consultations or basic diagnoses, through web-enabled devices for people who cannot immediately visit a dentist’s office.
The policy brief, “The Challenge of Meeting the Dental Care Needs of Low-Income California Adults With the Current Dental Workforce,” was published by the UCLA Center for Health Policy Research.
Related Articles
Delta Dental of Arkansas to Award $340,000 in Oral Health Education Grants
Pipeline Program Introduces Underrepresented Students to Dental School
ADA Asks Centers for Medicare and Medicaid Services to Prioritize Oral Health












