
Sponsored Editorial
Within every challenge lies distinct opportunity. The pandemic has taken its toll on dentistry, and every practice is working diligently to see its total patient base safely return.
Herein lies the opportunity. There has never been a more powerful time to effectively communicate the essential role of oral health and how it impacts overall health.
Oral health has never mattered more. How could dentistry even for a fleeting moment be deemed non-essential? Our world provides us with many unique opportunities to effectively impact the quality of the lives of every patient seated in our treatment rooms.
The Power of Patient Perception
So, what is your practice messaging? As dental professionals, we know the implications of the burden of chronic inflammation. The public is very aware of the importance of keeping healthy while living in a viral world. But they probably don’t fully understand the overwhelming burden that chronic inflammation places on the body and the function of immune response.
Most of today’s dental websites still carry a predominance of information focused on aesthetic dentistry, the attainment of a perfect smile, financing options, direct billing to insurance, and so on. Yes, this is all part of the appeal. But are we missing the mark in today’s world?
 |
In order to develop engagement strategies with on point messaging, we need to understand the mind of the public. What are the current perceptions of dental care and oral health, and what are the major factors dictating hesitancy in returning to the dental office?
Many of our patients are mindfully looking for ways to reduce exposure and transmission risk of SARS-CoV-2. Dentistry isn’t the only sector that has been profoundly impacted. Many people have delayed routine medical visits, which all helps to form the collateral damage of COVID-19.
The Centers for Disease Control and Prevention (CDC) confirmed the declining number of emergency visits in the pandemic era in its Morbidity and Mortality Weekly Report (MMWR). In fact, emergency visits declined 42% during the early COVID-19 pandemic.1 Virtual consultations through telehealth in both medicine and dentistry have become an alternate and often preferred method of care, according to academic and private researchers alike.2,3
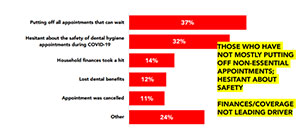
The Canadian Dental Hygienists Association recently commissioned Abacus Data to study the impact of COVID-19 on consumers’ dental hygiene care. The results of the public opinion poll confirmed that most adults have delayed seeing their dental hygienist since the pandemic began. But the 40% who have sought dental hygiene care have felt safe, and 92% reported receiving the same or better care than they would normally experience (Figure 1, above).4
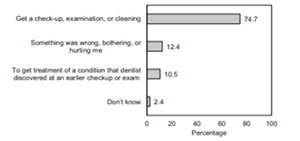 |
In another study, nearly three out of four adults (74.7%) reported delaying care for a checkup, exam, or professional cleaning, implying that most who delayed care were unlikely to have any perceived urgent need (Figure 2, above).5 The primary reason for delayed dental visits was the COVID-19 pandemic.
It’s now time to look beyond treating urgent dental care needs and resume routine dental care.6 The distinct opportunity to employ a comprehensive whole-body approach to dentistry is at our fingertips, yet many practitioners are fearful of embracing this paradigm shift and advocating for our patient’s overall health and wellness.
But our mindset must change if we are going to protect our patients. We need to shift from the mechanical aspect of dentistry to employing inflammation reduction strategies where the ideal outcome is a lack of inflammation.
Communicating the Risks
Our objectives are twofold. First we need to educate. Second, we need to mitigate risk.
COVID-19 has instigated an abundance of compelling research. Much of the focus has been on the impact of a chronic underlying inflammatory disease with increased incidence of COVID-19 complications. In fact, studies in New York, San Francisco, and Germany have named poor oral health and the presence of periodontal disease a risk factor in COVID-19 severity.7,8,9
Here’s the connection. Periodontal disease is the most common chronic inflammatory disease known to mankind, with far reaching systemic consequences. The burden of an ongoing inflammatory disease such as periodontal disease directs our immune system to an ongoing release of pro-inflammatory mediators or cytokines to an excessive level. COVID-19 is an illness characterized by dangerous levels of inflammation and an intense immune reaction that can lead to a storm of cytokines.
Researchers from around the world have joined forces to try and further understand the potential role of “cytokine storms” in dictating the severity of this viral infection. One such cytokine, the protein interleukin-6 (IL-6), is a recognized mediator of periodontal destruction that has risen to the research forefront.
According to recent research published in the Journal of the California Dental Association, researchers were shocked by their “discovery of the protein’s devastating, life-threatening impact to patients once they’re hospitalized. One tiny, inflammatory protein [IL-6] robbed them of their ability to breathe.”10
Researchers in Brazil, including the University of Sao Paolo, agree that the role of the dental hygienist in reducing the pathogenic bacterial load and levels of IL-6 accomplished through periodontal therapy is not to be underestimated.11,12 An abundance of research supports this outcome and benefit. We have a critical and essential role in mitigating risk for the patients we treat through reducing the inflammatory burden.
The same objective of inflammation reduction needs to be carried forward to self-care protocols. It has been proven repeatedly that power toothbrushes provide superior benefits to a manual toothbrush. How do they fare specifically when it comes to inflammation reduction?
A study to compare the effects of Philips Sonicare DiamondClean Smart toothbrush to an ADA reference manual toothbrush in reducing gingival inflammation, gingival bleeding and surface plaque following two and six weeks of home use concluded that Philips Sonicare DiamondClean Smart was statistically and significantly superior to the manual toothbrush and its competitors in reducing inflammation on all three evaluated indices.13,14 Another study positioned Philips Sonicare toothbrushes as significantly superior to manual toothbrushes in reducing gingival inflammation, gingival bleeding, and surface plaque.
In addition, the integration of “smart” technology accomplished through built-in sensors and real-time feedback allows Philips Sonicare DiamondClean Smart to evaluate and adjust our patients’ oral health habits to more effectively clean and in turn reduce inflammation daily at home.
BrushSync technology automatically synchronizes a smart brush head and a smart handle to truly provide a customized and superior brushing experience to manual toothbrushing. The microchip-enabled technology also informs users of its needs and orders new brush heads based on the individual’s actual brush head usage and brushing pressure, ensuring your patient is experiencing optimal results. It’s essentially an oral healthcare coach when we can’t be there!
The goal of care after the pandemic won’t be to place us back where we started. Rather, it will be an opportunity to evaluate, prioritize, learn and improve. We have an opportunity to create solutions that will enable our patients to feel supported in living their healthiest lives.
References
- Hartnett KP, Kite-Powell A, DeVies J, et al. Impact of the COVID-19 Pandemic on Emergency Department Visits — United States, January1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:699–704.
- Ghai S. Teledentistry during COVID-19 pandemic. Diabetes Metab Syndr. 2020;14(5):933-935.
- Varshneya R. Future of Teledentistry in the Post-Pandemic World. Feb 2021. https://www.oralhealthgroup.com/blogs/future-of-teledentistry-in-the-post-pandemic-world
- Abacus Data. Dental hygiene during the pandemic: Survey conducted for CDHA, 15-18 January 2021 [Full report]. Ottawa, ON: Canadian Dental Hygienists Association; 2021. Available from: https://files.cdha.ca/NewsEvents/SafetyAlerts/CDHA_COVID-19_Omnibus_Survey_Results.pdf
- Kranz AM, Gahlon G, Dick AW, et al. Characteristics of US Adults Delaying Dental Care Due to the COVID-19 Pandemic JDR Clin & Transl Res January 2021 Vol(6); Iss 1.
- Kalenderian E, Xiao Y, Spallek H et al. COVID-19 and Dentistry: Challenges and Opportunities for Providing Safe Care. Department of Health and Human Services. August 2020. https://psnet.ahrq.gov/primer/covid-19-and-dentistry-challenges-and-opportunities-providing-safe-care
- Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area. JAMA. 2020;323:2052–2059
- Botros N, Iver P, Ojcius DM. Is there an association between oral health and severity of COVID-19 complications? Biomed J. 2020 May 29.
- https://www.dentistrytoday.com/news/industrynews/item/6778-covid-19-patients-with-periodontitis-face-greater-risk-of-dying
- Molayem S, Pontes CC. The Mouth-COVID Connection. IL-6 Levels in Periodontal Disease – Potential Role in COVID-19 Related Respiratory Complication. Published online ahead of print July 30, 2020. J Calif Dent Assoc.
- Vidal F, Figueredo CM, Cordovil I, Fischer RG. Periodontal therapy reduces plasma levels of interleukin-6, C-reactive protein, and fibrinogen in patients with severe periodontitis and refractory arterial hypertension. J Periodontol. 2009 May;80(5):786-91.
- Marcaccini AM, Meschiari CA, Sorgi CA, Saraiva MC, de Souza AM, Faccioli LH, Tanus-Santos JE, Novaes AB, Gerlach RF. Circulating interleukin-6 and high-sensitivity C-reactive protein decrease after periodontal therapy in otherwise healthy subjects. J Periodontol. 2009 Apr;80(4):594-602.
- Milleman J, Milleman K, Olson M et al. Comparison of plaque and gingivitis reduction by Phliips Sonicare DiamondClean Smart toothbrush with Premium Gum Care brush head in Gum Health mode or Clean mode and a manual toothbrush. J Clin Dent 2019;30(Spec Iss A)A16-23.
- Mirza F, Argosino K, Ward M, et al. Comparison of the reduction in gingivitis and plaque following home-use of Philips Sonicare DiamondClean Smart with Premium Plaque Control brush head and Oral-B Genius 8000 with FlossAction Brush head. J Clin Dent 2019;30(Spec Iss A)A9–15.
Disclosure
Jo-Anne Jones is a returning Dentistry Today CE leader and consultant/key opinion leader with Philips Oral Healthcare.
Ms. Jones is an award-winning speaker who has given over a thousand presentations across the United States, Canada, England, Ireland, and Bermuda. She also joins the Dentistry Today’s Leaders in Continuing Education for the eleventh consecutive year. With her frank and open lecture style, focus on direct knowledge translation to practice, and educational and clinical resources, she has earned many loyal followers both nationally and internationally. She may be reached at jjones@jo-annejones.com.
Related Articles
Saving a Life from Oral Cancer Only Takes Five Minutes











