INTRODUCTION
When restoring adjacent implants in the partially edentulous patient, the decision on whether or not to splint them is a common clinical question. Although this situation has been researched by several biomechanical models and clinical studies, there remains much controversy, and many times, the decision is made based on misconceptions, outdated dogma, and/or clinician preference.1
RATIONALE FOR SPLINTING—BIOLOGIC COMPLICATIONS
The influence of splinting vs non-splinting dental implants has been evaluated by several biomechanical models. In general, stress analysis models show that splinting crowns leads to a better distribution of stresses in the implants and bone compared to non-splinted restorations.2 However, an important consideration is that in vitro models are static and do not mimic the adaptive properties of living supporting bone. Wolff’s Law states that bone will adapt to the loads under which it is placed. Bone adapts its mechanical properties according to the needed mechanical function.3 Under overload conditions, bone mass and strength increase. Early theories on the cause of marginal bone loss around dental implants focused on biomechanics and theorized that greater forces and higher stresses would cause overload, resulting in bone loss.4 However, there is a lack of substantive evidence that occlusal overload is a primary etiology of marginal bone loss.5,6 On the contrary, in conditions that would increase peri-implant stress, such as narrow or short implants, tilted implants, cantilevered pontics, or fewer implant numbers for full-arch prostheses, studies have not shown an increase in marginal bone loss or a decrease in implant survival.7-11 Two systematic reviews and meta-analyses on splinting vs non-splinting adjacent implants with internal connections concluded there was no difference in marginal bone loss or implant survival.12,13 Current literature does not support the routine splinting of dental implants to prevent bone overload.
Many patients prefer individual implant crowns that mimic their natural dentition. A clinical study that restored adjacent implants with splinted prostheses on one side and non-splinted crowns on the contralateral side found many preferred the non-splinted crowns, reporting that hygiene was easier.14 If implant crowns are splinted, the restoration must be well-designed with adequate access for oral hygiene. Patients must be educated on the use of hygiene aids, such as floss threaders and/or interproximal brushes. Some studies have found greater marginal bone loss around splinted, short implants.15-17 This may be due to more difficulty with oral hygiene and the development of peri-implantitis.
RATIONALE FOR SPLINTING—TECHNICAL COMPLICATIONS
Regardless of implant length, stress distribution is highest in the crestal region.18 Finite element stress analyses show that, independent of implant length, the maximum bone stress is virtually constant.19 The moment of force, or torque, is a product of the force applied multiplied by the distance from the pivot point. As such, an off-axis or lateral load on a taller implant crown will have a greater moment of force. Biomechanical studies have concluded that placing a longer implant to improve the C/I ratio will not offset a tall implant crown. Therefore, the term “crown-to-implant ratio” is a misnomer and should not be used in the discussion of implant mechanics. Some clinicians recommend routine splinting of short implants (<8 mm), but this is unnecessary if the crown-abutment height is not excessive (Figures 1 to 5). The main focus should be on the crown-abutment height, not implant length.

Figure 1. Preoperative view of a failed bridge and an atrophic ridge.
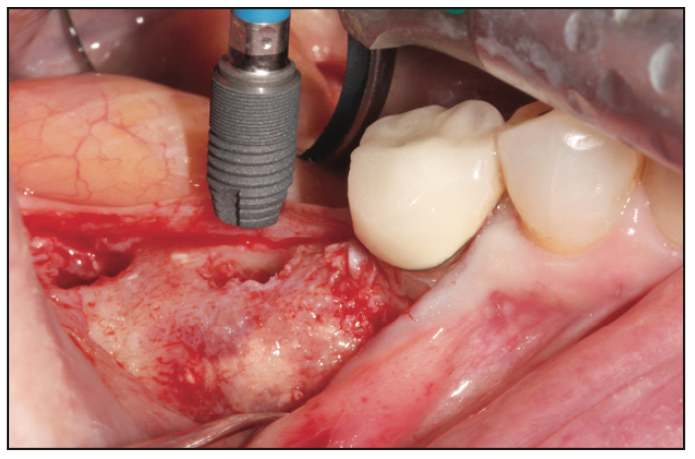
Figure 2. Placement of an 8.0-mm implant in the grafted ridge.
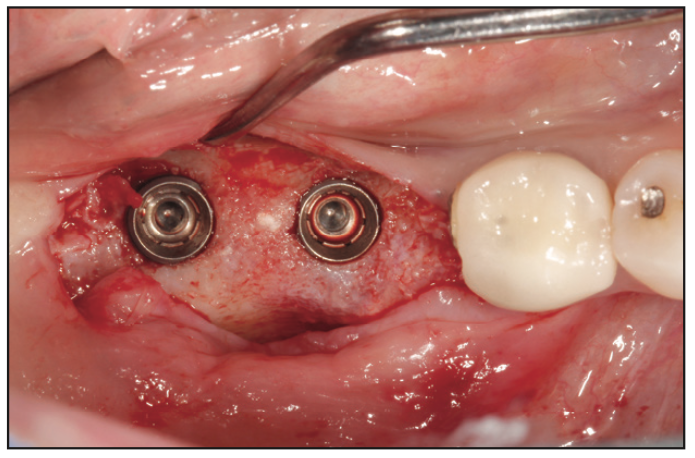
Figure 3. Occlusal view of the 2 implants in grafted bone.

Figure 4. The implant crowns were not splinted as the crown height was ≤ 10 mm.
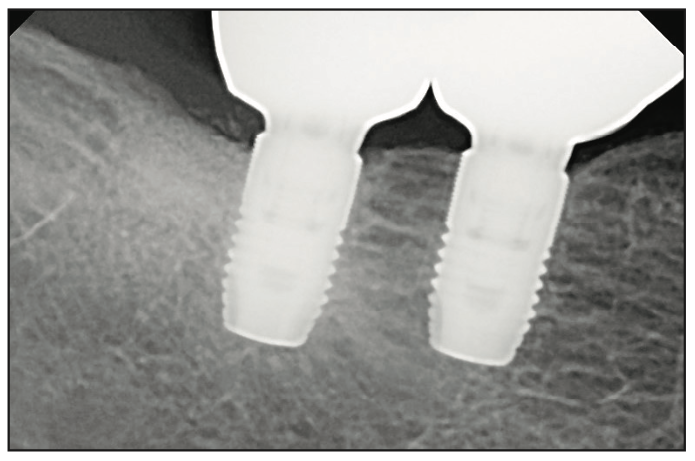
Figure 5. Periapical radiograph of the individual implant crowns.
One of the main indications for splinting adjacent implants is when jaw atrophy results in more prosthetic space that requires a greater crown-abutment height. Excessive crown-abutment height will place greater stress on the implant-abutment connection, especially when there is off-axis or lateral loading. This can cause technical complications, such as screw loosening, component fracture, and even implant neck fracture. A photoelastic study evaluated the effect of splinting implants with different crown heights using gauges to measure the strain.20 Under non-axial loads, a significant increase in strain around the implants when the crown height increased from 10 to 15 mm was found. Splinting did not prevent prosthetic failure when the crown height was greater than 15 mm. Therefore, when the implant-abutment crown height is greater than 10 mm, implant splinting should be considered (Figures 6 to 11). An additional advantage of splinting in this scenario is the ability to reduce spaces that collect food debris. Besides splinting, another option to improve the mechanics of excessive prosthetic space is to use a tissue-level implant. The supra-bony component of the tissue-level implant reduces the crown-abutment height by 1.8 mm. It also provides a wider prosthetic platform than a bone-level implant (Figures 12 to 17).

Figure 6. Pre-op view of the atrophic right maxilla.
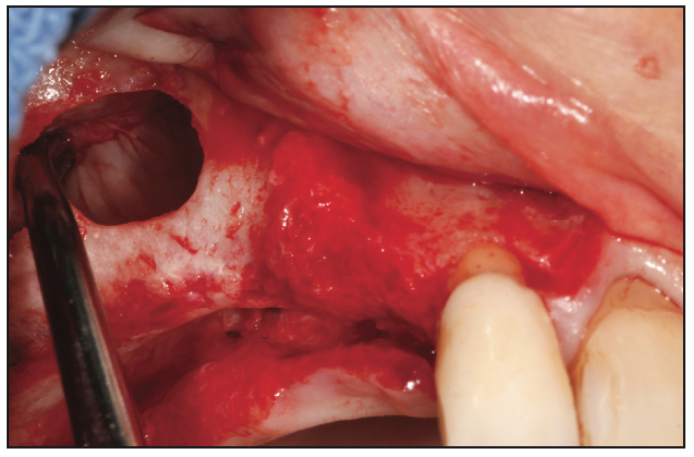
Figure 7. Sinus and ridge bone grafting were performed to increase the bone volume.
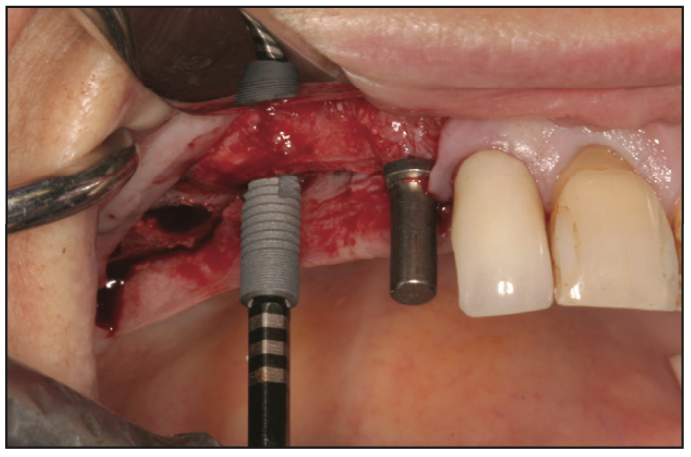
Figure 8. After 6 months of healing, implants were inserted into the healed graft.
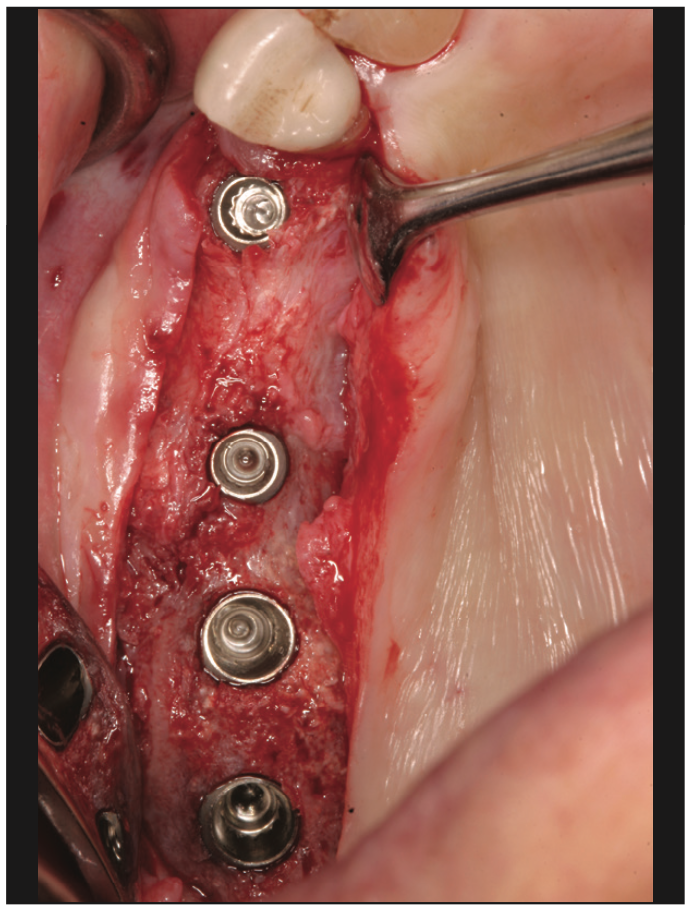
Figure 9. Occlusal view of the 4 implants placed into the healed graft.

Figure 10. The 4 implants were all splinted as the crown height was > 10 mm.
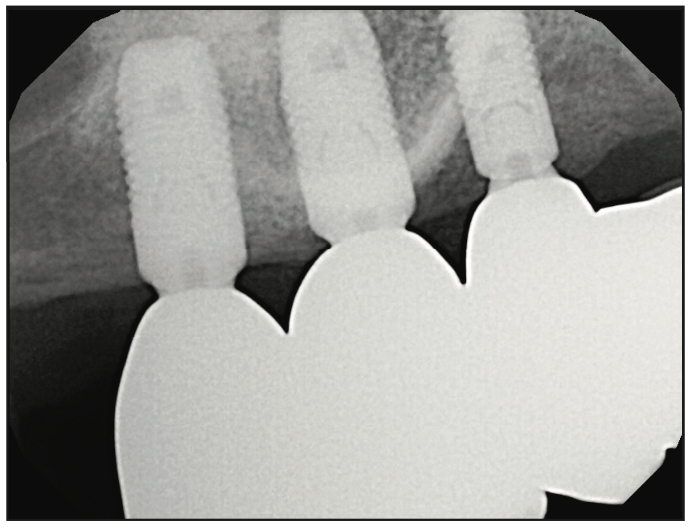
Figure 11. Periapical radiographs of the splinted implant restoration.

Figure 12. Pre-op view of the atrophic posterior mandible.
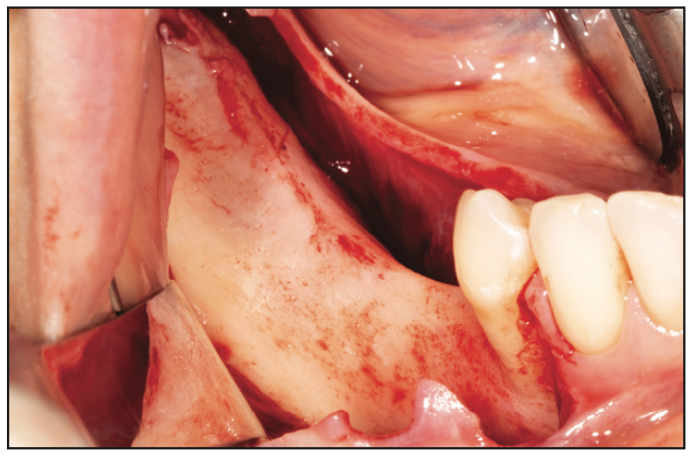
Figure 13. The atrophic ridge requires bone width and height augmentation.

Figure 14. Guided bone regeneration using autogenous bone and a dense PTFE membrane.
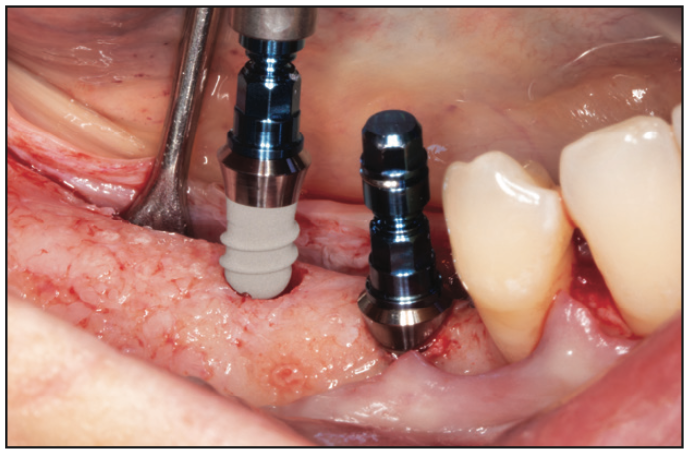
Figure 15. Two short tissue-level implants (6.0 mm) are inserted into the reconstructed mandible.
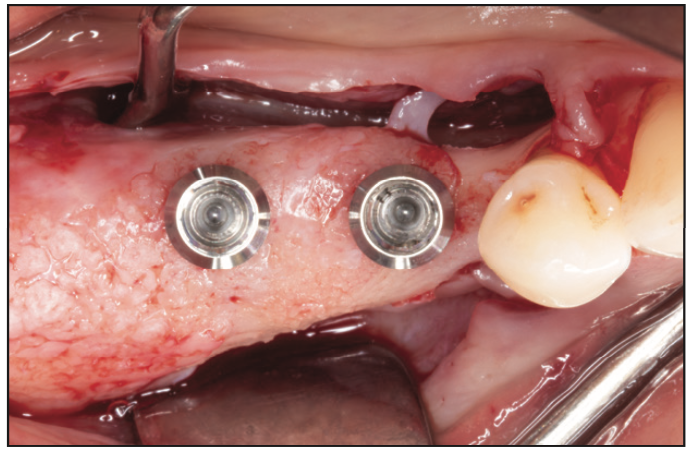
Figure 16. Occlusal view of the 2 tissue-level implants.
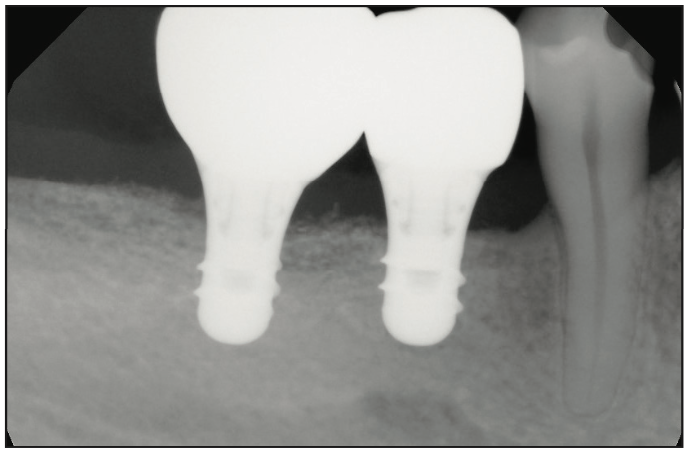
Figure 17. Periapical radiograph of the individual unsplinted implant crowns.
Parafunctional habits may be associated with greater technical and mechanical complications.21 Even when crown-abutment heights are not excessive, it may be prudent to consider splinting in patients with bruxism, especially if dental wear has compromised their protective anterior guidance. The implant position can also influence the decision to splint. With tooth loss and bone remodeling, the facial plate resorbs medially. As such, a dental implant may be placed more palatal or lingual than ideally. This medial position of the implant can create greater off-axis occlusal loading on the implant crown resulting in a higher risk of mechanical complications. If adjacent posterior implants are located medial to the center of the crowns, then splinting is suggested to counteract non-axial forces. Splinting may also be recommended if the implant angulation significantly deviates from the direction of the occlusal load. Although an angled abutment can correct the path of prosthetic retention or screw access, it does not change the increase in stress at the connection.
When the ridge width is diminished, a narrower-diameter implant may be used. A smaller diameter could challenge the mechanical support of the implant crown as the abutment connection is reduced. When using a smaller-diameter implant (≤ 4.0 mm) to replace a molar, splinting to an adjacent implant should be considered. Another option to manage the ridge discrepancy is to perform horizontal bone augmentation to allow the placement of a wider-diameter implant in a more ideal location. One particular advantage of splinting multiple adjacent implants is that if an implant failure occurs, the existing prosthesis may still function after its removal.
It is easier to achieve a passive fit of individual implant crowns vs multiple splinted implant crowns, especially when screw retention is used. A misfit of the prosthesis can generate forces that may result in the loosening of abutment screws or fracture of implant components, superstructure, veneering porcelain, or the implant. If multiple implants are planned for splinting with a screw-retained prosthesis, it is prudent to use abutments as opposed to fabricating the splinted crowns directly to the implants. Any misfit and microgap between the prosthesis and the implant would allow ingrowth of microflora, resulting in inflammation and bone loss. By using an abutment, any prosthetic misfit is moved away from the bone level. It may also allow the clinician to better visualize the fit of the crown margins. If the crowns are removed, this does not disrupt the soft-tissue attachment on the implant abutment. The use of abutments has been shown to better maintain marginal bone levels around splinted implants compared to a direct connection.22 If cement-retained splinted crowns are planned, custom abutments should be utilized to improve the emergence profile of the restoration and optimize the margin position for cement removal.
Another advantage of single crowns is the impact if a porcelain fracture occurs. The incidence of porcelain fracture with implant restorations is higher than with natural teeth, and the presence of a screw-access opening further increases the risk of this complication.23 If porcelain fracture occurs on a crown, it only impacts one unit instead of an entire splinted restoration.
CONCLUSION
Dentists should reserve the splinting of implant crowns to clinical situations that may risk technical complications, such as excessive crown height (> 10 mm), parafunctional habits, loss of anterior guidance, malposed or angled implant positions, or narrower-diameter implants replacing molars. Whenever possible, splinting should be avoided for easier oral hygiene, passive prosthetic fit, and easier repair.
REFERENCES
1. Resnik R. Chapter 7: Stress Treatment Theorem for Implant Dentistry. In: Resnik R, ed. Misch’s Contemporary Implant Dentistry, 4th ed. Elsevier; 2020:152–74.
2. Hauchard E, Fournier BP, Jacq R, et al. Splinting effect on posterior implants under various loading modes: a 3D finite element analysis. Eur J Prosthodont Restor Dent. 2011;19(3):117–22.
3. Frost HM. The Utah paradigm of skeletal physiology: an overview of its insights for bone, cartilage and collagenous tissue organs. J Bone Miner Metab. 2000;18(6):305–16. doi:10.1007/s007740070001
4. Bidez MW, Misch CM. Chapter 6: Clinical Biomechanics in Implant Dentistry. In: Misch CE, ed. Contemporary Implant Dentistry, 2nd ed. Mosby; 1999:310–4.
5. Afrashtehfar KI, Afrashtehfar CD. Lack of association between overload and peri-implant tissue loss in healthy conditions. Evid Based Dent. 2016;17(3):92–3. doi:10.1038/sj.ebd.6401193
6. Sadowsky SJ. Occlusal overload with dental implants: a review. Int J Implant Dent. 2019;5(1):29. doi:10.1186/s40729-019-0180-8
7. Lemos CA, Ferro-Alves ML, Okamoto R, et al. Short dental implants versus standard dental implants placed in the posterior jaws: A systematic review and meta-analysis. J Dent. 2016;47:8-17. doi:10.1016/j.jdent.2016.01.005
8. Schiegnitz E, Al-Nawas B. Narrow-diameter implants: A systematic review and meta-analysis. Clin Oral Implants Res. 2018;29 Suppl 16:21-40. doi:10.1111/clr.13272
9. Daudt Polido W, Aghaloo T, Emmett TW, et al. Number of implants placed for complete-arch fixed prostheses: A systematic review and meta-analysis. Clin Oral Implants Res. 2018;29 Suppl 16:154–83. doi:10.1111/clr.13312
10. Freitas da Silva EV, Dos Santos DM, Sonego MV, et al. Does the presence of a cantilever influence the survival and success of partial implant-supported dental prostheses? Systematic review and meta-analysis. Int J Oral Maxillofac Implants. 2018;33(4):815–23. doi:10.11607/jomi.6413
11. Lin WS, Eckert SE. Clinical performance of intentionally tilted implants versus axially positioned implants: A systematic review. Clin Oral Implants Res. 2018;29 Suppl 16:78-105. doi:10.1111/clr.13294
12. de Souza Batista VE, Verri FR, Lemos CAA, et al. Should the restoration of adjacent implants be splinted or nonsplinted? A systematic review and meta-analysis. J Prosthet Dent. 2019;121(1):41-51. doi:10.1016/j.prosdent.2018.03.004
13. Li QL, Yao MF, Cao RY, et al. Survival rates of splinted and nonsplinted prostheses supported by short dental implants (≤8.5 mm): a systematic review and meta-analysis. J Prosthodont. 2022;31(1):9-21. doi:10.1111/jopr.13402
14. Clelland N, Chaudhry J, Rashid RG, et al. Split-mouth comparison of splinted and nonsplinted prostheses on short implants: 3-year results. Int J Oral Maxillofac Implants. 2016;31(5):1135–41. doi:10.11607/jomi.4565
15. Rokni S, Todescan R, Watson P, et al. An assessment of crown-to-root ratios with short sintered porous-surfaced implants supporting prostheses in partially edentulous patients. Int J Oral Maxillofac Implants. 2005;20(1):69-76.
16. Cochran DL, Nummikoski PV, Schoolfield JD, et al. A prospective multicenter 5-year radiographic evaluation of crestal bone levels over time in 596 dental implants placed in 192 patients. J Periodontol. 2009;80(5):725–33. doi:10.1902/jop.2009.080401
17. Lee JB, Kim MY, Kim CS, et al. The prognosis of splinted restoration of the most-distal implants in the posterior region. J Adv Prosthodont. 2016;8(6):494-503. doi:10.4047/jap.2016.8.6.494
18. Geng JP, Tan KB, Liu GR. Application of finite element analysis in implant dentistry: a review of the literature. J Prosthet Dent. 2001;85(6):585–98. doi:10.1067/mpr.2001.115251
19. Pierrisnard L, Renouard F, Renault P, et al. Influence of implant length and bicortical anchorage on implant stress distribution. Clin Implant Dent Relat Res. 2003;5(4):254–62. doi:10.1111/j.1708-8208.2003.tb00208.x
20. Nissan J, Ghelfan O, Gross O, et al. The effect of crown/implant ratio and crown height space on stress distribution in unsplinted implant supporting restorations. J Oral Maxillofac Surg. 2011;69(7):1934–9. doi:10.1016/j.joms.2011.01.036
21. Zhou Y, Gao J, Luo L, et al. Does bruxism contribute to dental implant failure? A systematic review and meta-analysis. Clin Implant Dent Relat Res. 2016;18(2):410–20. doi:10.1111/cid.12300
22. Göthberg C, Gröndahl K, Omar O, et al. bone and soft tissue outcomes, risk factors, and complications of implant-supported prostheses: 5-years RCT with different abutment types and loading protocols. Clin Implant Dent Relat Res. 2018;20(3):313–21. doi:10.1111/cid.12587
23. Kinsel RP, Lin D. Retrospective analysis of porcelain failures of metal ceramic crowns and fixed partial dentures supported by 729 implants in 152 patients: patient-specific and implant-specific predictors of ceramic failure. J Prosthet Dent. 2009;101(6):388–94. doi:10.1016/S0022-3913(09)60083-4
ABOUT THE AUTHORS
Dr. Misch received his DDS degree from the University of Michigan in 1985. In 1991, he received certificates in postgraduate prosthodontics and oral implantology as well as a Master of Dental Science degree from the University of Pittsburgh. Dr. Misch then completed a residency in oral and maxillofacial surgery in Pittsburgh. He is board-certified by the American Board of Oral and Maxillofacial Surgery as well as the American Board of Oral Implantology/Implant Dentistry. He is a clinical associate professor at the University of Florida, University of Pennsylvania, and University of Michigan. Dr. Misch serves as editor-in-chief of the International Journal of Oral Implantology and is on the editorial boards of several other dental journals. He practices as a dual specialist at Misch Implant Dentistry in Sarasota, Fla. He can be reached at cmisch@umich.edu.
Disclosure: Dr. Misch reports no disclosures.
Dr. Misch-Haring received her DMD degree in 2019 from the University of Alabama at Birmingham (UAB) School of Dentistry, graduating as class valedictorian. She then completed a residency in periodontics at UAB in 2022 and now practices as a periodontist at Misch Implant Dentistry in Sarasota, Fla. Dr. Misch-Haring is a member of the Omicron Kappa Upsilon dental society, the American Academy of Periodontology, and the Academy of Osseointegration. She can be reached at mmischharing@gmail.com.
Disclosure: Dr. Misch-Haring reports no disclosures.











