INTRODUCTION
Delivering a set of veneers can be a stressful procedure in a dental office. Patients invest a significant amount of both time and financial resources to enhance their smiles and have worn their temporary veneers for several weeks. As they eagerly anticipate the delivery of their permanent veneers, it becomes imperative to execute a technique that guarantees the thorough removal of the flowable composite used to bond the temporary veneers. This article introduces an effective method that ensures the elimination of all remnants of flowable composite prior to the try-in and cementation of the permanent veneers. By use of this method, it serves to benefit the practitioner in 3 crucial ways. Primarily, it allows the practitioner to selectively eliminate residual flowable composite without causing damage to the prepared tooth structure. This meticulous approach significantly minimizes the risk of inadvertent tooth structure removal, particularly at the margins, thereby mitigating the potential for open margins that could undermine the overall integrity of the restoration. Moreover, this technique’s application helps to ensure the removal of all remnants of flowable composite, which, if left by mistake, could exhibit sharp edges or angles that could lead to fracture of the veneers when trying them in. And lastly, this technique helps the practitioner rule out one of the factors that could be causing the veneers not to seat completely during the try-in step of the delivery procedure. The use of “The Scorpion Technique” leads to a more predictable and systematic way to deliver permanent veneers.
Delivery of Temporary Veneers
The author has found using “the spot-etch-and-bond technique” for bonding in temporary veneers to be the most predictable method. This technique involves etching (38% phosphoric acid) a small, 2-mm circular area in the center of the prepared tooth, followed by placing Gluma (Kulzer) and then applying Scotchbond Universal Plus Adhesive (3M) on the same circular area (Figure 1). The Scotchbond Universal Plus Adhesive is light-cured for 20 seconds. A flowable composite is then applied to the intaglio surface of the temporary veneers and placed on the prepared tooth structure. All excess flowable composite needs to be removed at the margins of the temporary veneers. A rubber tip GUM Stimulator (Sunstar Americas) works well to remove any excess flowable composite without causing any trauma to the gingiva. Once all excess flowable composite has been removed, the temporary veneers are light-cured for 10 seconds.

Figure 1. Etch placed on a 2-mm circular area in the center of each tooth.
The author has tried other techniques for the retention of temporary veneers. Temporary cements such as Temp-Bond Clear (Kerr) have been used. Still, the author found the retention to be insufficient when the patients had to wear the temporary veneers for any extended time period, such as 3 to 4 weeks. It can cause frustration for both the practitioner and patient when the temporary veneers debond prior to the delivery date. Another technique that the author has tried is the “shrink-wrap technique.”1 This technique involves using a silicone matrix filled with bisacryl material, which is seated onto the prepared teeth. The bisacryl material is allowed to completely polymerize before the silicone matrix is removed, and then the margins are refined using an extra-fine mosquito diamond bur. The author found this technique to be too retentive, and removal was time-consuming, especially if the interproximal contacts were open. There was also a concern about causing the papilla to become blunted if the linguogingival embrasures were not opened up enough during the refinement of the margins of the temporary veneers.
The Scorpion Technique
The spot-etch-and-bond technique provides the ideal amount of retention while also allowing for adjustment of the temporary veneers. The temporary veneers can be refined in the linguogingival embrasures prior to bonding, therefore decreasing the chance of blunting the papilla, but this technique is not perfect. With the spot-etch-and-bond technique, there is still the question of whether all of the flowable composite has been removed prior to trying in the permanent veneers.
Due to the nature of both temporary and permanent veneers being very thin, the shade of the flowable composite needs to be very close to that of the stumpf shade of the tooth. A noticeable disparity in color, whether darker or lighter, will manifest through the temporary veneer, undermining the desired aesthetics. At the same time, if one selects a shade of composite that is very close to that of the stumpf shade of the tooth, then this creates a challenge in discerning and eliminating residual composite. Failure to remove all remnants of flowable composite can precipitate 2 significant issues. Primarily, any residual flowable composite poses a risk of fracturing the delicate veneer during the try-in phase of the delivery appointment. Secondly, incomplete removal of the residual composite may prevent full seating of the veneer during insertion, prompting the practitioner to question the cause.
The practitioner needs to determine whether the culprit is lingering composite or interproximal contact concerns. The Scorpion Technique emerges as an answer, facilitating a comprehensive and meticulous approach to veneer placement. This technique ensures the elimination of any lingering flowable composite and refining the overall veneer delivery process.
The author uses what she calls “The Scorpion Technique” to bond in the temporary veneers and later remove them at the delivery appointment. The protocol for this technique involves spot-etching a small, 2-mm circular area on the prepared tooth, followed by using a desensitizer, such as Gluma, and a bonding agent, such as Scotchbond Universal Plus Adhesive, which is applied on this same small, 2-mm circular area. The Scotchbond Universal Plus Adhesive is light-cured for 20 seconds. Following the light-curing of the Scotchbond Universal Plus Adhesive, OMNICHROMA FLOW BULK (Tokuyama Dental) is placed on the intaglio surface of the temporary veneers and used as the bonding agent for the temporary veneers (Figures 2 and 3). It is crucial that the excess flowable composite at the margins of the temporary veneers be removed prior to light curing for 10 seconds.

Figure 2. A 2-mm circular area of OMNICHROMA FLOW BULK (Tokuyama Dental).

Figure 3. OMNICHROMA FLOW BULK.
This technique helps ensure that the temporary veneers will remain bonded for the time required for the patient to evaluate the aesthetics, along with testing phonetics, function, and occlusion. The margins of the temporary veneers are sealed, which helps to maintain the gingival health, which is paramount when delivering the permanent veneers. During the removal of the temporary veneers, the author prepares a thin vertical line through the facial of the temporary veneer and takes care not to touch the tooth structure with the bur. A crown splitter is then used to create a torquing force between the 2 pieces of the temporary veneer, which causes the temporary veneer to debond from the tooth.
The process is repeated until all the temporary veneers have been removed. After this process has been completed, residual flowable composite remains on the 2-mm circular area in the middle of the tooth that was spot-etched and bonded to during the delivery of the temporary veneers. This flowable composite is very difficult to see and detect.
The author lives in Arizona where scorpions are “invisible enemies” that blend in with almost any type of flooring. The sting of a scorpion is extremely painful and can cause numbness for several hours. The scorpions have what is called a “hyaline layer” in their exoskeleton that causes them to illuminate in the dark when a black light is shone on them. The author knows that some dental composites have glass fillers that impart a fluorescent property to them.2 Incorporating these artificial materials makes the composite appear more natural and lifelike. With some experimentation, the author was able to determine which flowable composites demonstrate the ability to illuminate when exposed to black light in a darker environment. After removing the temporary veneers, the overhead light is focused toward the patient’s feet to create a darker environment. If the practitioner uses loupes with a headlamp, then the headlamp needs to be turned off as well. There will still be ambient light in the room due to ceiling lighting, but no light will be directly shining on the prepared teeth. The black light is then shone on the patient’s teeth, and any residual flowable composite becomes illuminated (Figures 4 and 5). The practitioner then notes the exact location of the residual composite and removes it with a fine, flame-shaped diamond bur. It will take several sessions of shining the black light on the tooth to detect the exact location of the residual flowable composite and then going back to remove it. This very precise technique ensures only the residual flowable composite is completely removed and that the underlying tooth structure is not overly prepared, guaranteeing the veneer’s marginal fit. The practitioner is now able to rule out the residual composite as a possible cause for the permanent veneers improperly seating.

Figure 4. Photo of flowable composite on a tooth after temporary veneers have been removed.

Figure 5. Black Light (Gearlight).
During the development of this technique, several different brands of flowable composite were tested to evaluate their levels of fluorescence (Figures 6 and 7). Fluorescence, as defined, involves the absorption of light by a substance and its emission at the same time at a longer wavelength.3 Notably, OMNICHROMA FLOW BULK exhibited the most pronounced illumination when compared to the other 5 tested flowable composites. The luminescent quality of dental composites arises from the incorporation of rare earth oxides in their glass fillers.4
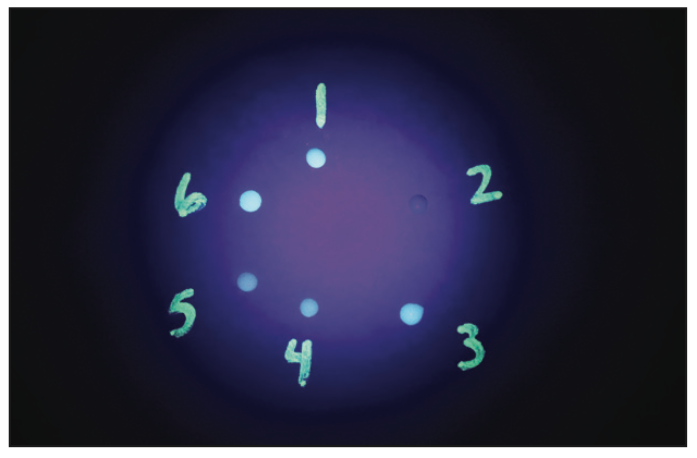
Figure 6. Evaluation of the level of fluorescence of multiple different brands of flowable composite.
Figure 7. Chart of names of flowable composites present in Figure 6.
The degree of illumination of the composite is based on the amount of rare earth oxides incorporated into the composition of the composite. When placing a composite restoration, a practitioner would want the amount of illumination to match that of the surrounding enamel and dentin, but with the Scorpion Technique, one would want the brightest level of illumination of the composite in order to easily detect it. Incorporating the Scorpion Technique will help make a veneer delivery appointment more predictable and less stressful.
CASE REPORT
A 42-year-old female had considerable damage due to severe acid reflux during her pregnancy with twins. She also had signs of damage due to bruxism. The patient expressed a desire to repair her damaged teeth and also to increase the length and fullness of her smile (Figures 8 and 9). A comprehensive evaluation was completed for this patient, which included radiographs, full-mouth periodontal probing, temporomandibular joint evaluation, and evaluation of her current occlusal scheme.

Figure 8. Preoperative frontal view full smile (1:2), non-retracted.

Figure 9. Pre-op frontal view of upper and lower teeth (1:2), retracted
After reviewing the information gathered at the comprehensive evaluation, it was determined that the patient’s central incisors were very “boxy” and did not display the ideal width-to-length ratio.5 The patient was presented with 2 options to correct this issue. The first option was orthodontic treatment in which the central incisors would be intruded. The second option presented was a crown-lengthening procedure. It was also discussed with the patient that she would need to have a connective tissue graft on tooth No. 6 to address the gingival recession that was present. The patient elected to have the crown-lengthening and connective tissue graft procedures completed along with having her teeth prepared for 10 porcelain veneers.
A surgical stent was fabricated from the diagnostic wax-up to act as a guide for altering the position of the gingiva on teeth Nos. 8 and 9. The patient presented for treatment, and a gingivectomy was performed on teeth Nos. 8 and 9 using the surgical guide. Teeth Nos. 4 to 13 were prepared for porcelain veneers (Figure 10). The Scorpion Technique was used to bond the temporary veneers in place. The patient was then sent to Dr. Brent Boyse at Arizona Maxillofacial Surgeons (Mesa, Ariz). Dr. Boyse used the temporary veneers as a guide for where to remove bone on teeth Nos. 8 and 9 in order to avoid having a biologic width violation with the permanent veneers. He also used the temporary veneers as a guide for the placement of the connective tissue graft on tooth No. 6. The patient remained in temporary veneers for 6 weeks while the gingiva healed. The temporary veneers were removed 6 weeks after the crown-lengthening procedure and connective tissue graft placement so that the margins could be refined. The author wanted to be sure the prepared margins were equigingival to the altered gingival tissues following the crown-lengthening and connective tissue grafting procedures. The use of the Scorpion Technique made removal of the residual flowable composite easier. It was imperative that all of the residue composite be removed because the impressions for the final veneers were taken after refinement of the margins. The patient remained in temporary veneers for 5 more weeks while the dental laboratory was fabricating the final restorations. The spot-etch-and-bond technique allowed for adequate retention of the temporary veneers and ensuring that the margins were closed.

Figure 10. Frontal view of upper and lower teeth (1:2), retracted view of prepared teeth and gingiva.
After the clinical crown-lengthening procedure, a connective tissue graft, and being in temporary veneers for almost 3 months, the patient was ready to have the permanent veneers tried in and delivered. By using the Scorpion Technique during the delivery appointment, the author was able to eliminate one of the factors that could create a problem during the trying in and seating of the permanent veneers. Even after having this patient wear 2 different sets of temporary veneers, the author could be confident that all residual flowable composite had been removed from the prepared teeth. If there were issues with the fit of the veneers, the interproximal contacts whould have been evaluated.

Figure 11. Postoperative frontal view of the full smile (1:2), non-retracted.

Figure 12. Post-op lateral view of the full smile (1:2), non-retracted.

Figure 13. Post-op frontal view of upper and lower teeth (1:2), retracted.

Figure 14. Post-op frontal view of upper and lower teeth (1:2), retracted, all teeth restored.

Figure 15. Pre-op full-face (1:10), non-retracted view.

Figure 16. Post-op full-face (1:10), non-retracted view.
This patient was so pleased with the aesthetic result of the porcelain veneers on her maxilla that she decided to proceed with having porcelain veneers placed on her mandibular arch to complete her smile makeover (Figures 11 to 16). Doing this type of dentistry demands that the practitioner display a high level of skill along with extreme attention to the smallest details. Incorporating techniques like the Scorpion Technique allows more control of the procedure and, therefore, creates a less stressful appointment for both the practitioner and the patient.
ACKNOWLEDGMENTS
The author would like to thank technicians Nelson Rego and Juan Rego of Smile Designs by Rego (Santa Fe Springs, Calif) for their laboratory support and ceramic artistry, which were critical components in the success and outcome of this case.
REFERENCES
1. Gürel G, Morimoto S, Calamita MA, et al. Clinical performance of porcelain laminate veneers: outcomes of the aesthetic pre-evaluative temporary (APT) technique. Int J Periodontics Restorative Dent. 2012;32(6):625–35.
2. Volpato CAM, Pereira MRC, Silva FS. Fluorescence of natural teeth and restorative materials, methods for analysis and quantification: A literature review. J Esthet Restor Dent. 2018;30(5):397-407. doi:10.1111/jerd.12421
3. Mualla S. Fluorescence and dentistry. IOSR-JDMS. 2016;15(3)v9:65-75. doi:10.9790/0853-1503096575
4. Leontiev W, Magni E, Dettwiler C, et al. Accuracy of the fluorescence-aided identification technique (FIT) for detecting tooth-colored restorations utilizing different fluorescence-inducing devices: an ex vivo comparative study. Clin Oral Investig. 2021;25(9):5189–96. doi:10.1007/s00784-021-03826-7
5. American Academy of Cosmetic Dentistry. AACD Guide to Accreditation Criteria: Contemporary concepts in smile design. American Academy of Cosmetic Dentistry; 2014.
ABOUT THE AUTHOR
Dr. Brauer earned her DDS degree from the University of Missouri, Kansas City, in 2003. She has been practicing dentistry in Arizona for the last 18 years. Since 2006, she’s worked in a dental practice that she opened with her husband, Dr. Howie Brauer. Her focus and passion over the last 10 years has been cosmetic dentistry. She is an accredited member of the American Academy of Cosmetic Dentistry. Outside of work, Dr. Brauer stays busy with the numerous activities that her 3 daughters are involved in. She can be reached at joyfulsmilesaz@gmail.com.
Disclosure: Dr. Brauer reports no disclosures.











