Local anesthesia (LA) forms the foundation of pain control techniques in dentistry. These drugs prevent the passage of noxious stimuli to the patient’s brain where it would be interpreted as painful. Other techniques of pain control are available, including general anesthesia, hypnosis, acupuncture, and electronic dental anesthesia, but none is as consistently reliable and as safe as LA.
THE LA CARTRIDGE
|
||
| Figure 1. LA cartridge. | ||
 |
||
| Figure 2. Chemical structure of Articaine HCI. |
The LA cartridge is a glass cylinder (plastic cartridges of LA are available in some countries) capable of holding 2.0 mL of solution (Figure 1). A thick silicone rubber stopper (plunger) seals one end of the cartridge. As a result, a filled cartridge contains 1.8 mL of anesthetic solution. (In some countries, such as Great Britain, Australia, and South Africa, LA cartridges contain 2.2 mL). The opposite end of the cartridge has a thin latex membrane through which the needle penetrates into the cartridge.
 |
 |
ALLERGY
LA Allergy
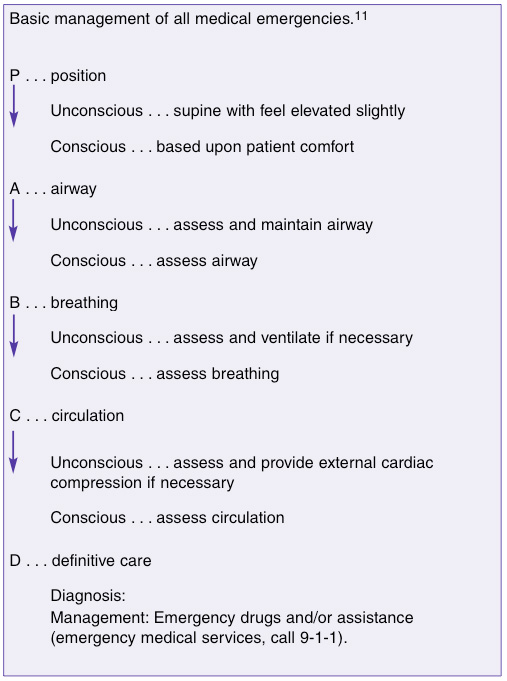 |
| Figure 3. Basic management of all medical emergencies.11 |
True, documented, and reproducible allergy to ester-type LAs is relatively common, while with amide-type LAs allergy is such a rarity as to be virtually nonexistent3 (Table 2). Reports of “alleged” allergy (eg, “Doctor, I am allergic to Novocain”) are more frequent. Confronted with an alleged LA allergy, the clinician must: (1) always believe the patient and not administer any LA, including (or perhaps, especially) topical anesthetic, and (2) determine what actually happened during their “allergic reaction.” Questions to ask of the patient (dialogue history) are presented in Table 3.
Allergy to Components of a LA Cartridge
 |
Though allergy to a LA drug is highly unlikely, allergy may occur to one of the components included in the cartridge.
 |
 |
Specific mention must be made of articaine HCl, an amide local anesthetic that contains a sulfur molecule in its chemical structure (Figure 2). As the sulfur molecule is an integral part of the thiophene ring of articaine HCl, it is not available to act as an allergen. Articaine HCl may safely be administered to patients with sulfur allergy. Introduced in 1975, and presently available in approximately 131 countries, there have been no reported cases of allergy to articaine HCl.5
Epinephrine Allergy
Allergy to epinephrine cannot occur. Questioning of the “epinephrine-allergic” patient (see dialogue history, above) immediately reveals signs and symptoms related to increased blood levels of circulating catecholamines (tachycardia, palpitation, sweating, nervousness), likely the result of fear of receiving injections (release of endogenous catecholamines [epinephrine and norepinephrine]).
Latex Allergy
 |
The thick plunger (also known as the “stopper”) on one end of the LA cartridge and the thin diaphragm on the other end of the cartridge (Figure 1) through which the needle penetrates may contain latex. As latex allergy is of growing concern among all healthcare professionals, the risk of provoking an allergic reaction in a latex-sensitive patient must be considered. A recent review of the literature on latex allergy and local anesthetic cartridges by Shojaei and Haas6 demonstrates that latex allergen can be released into the LA solution as the needle penetrates the diaphragm, but there were no reports or case studies in which an allergic response to the latex component of the cartridge containing a dental local anesthetic was documented.
OVERDOSE (TOXIC REACTIONS)
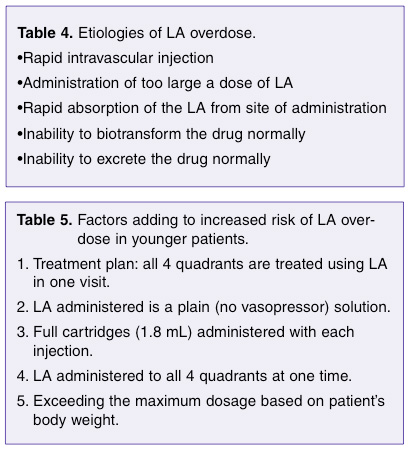
Overdose (also known as toxic reaction) occurs when the blood (serum) level of LA in either the central nervous system (CNS) or myocardium is elevated to a point where the drug produces potentially life-threatening events. The overdose reaction persists until the blood level of the drug in these “target” organs falls below the toxic level. Table 4 lists ways in which overly high blood levels can be produced.
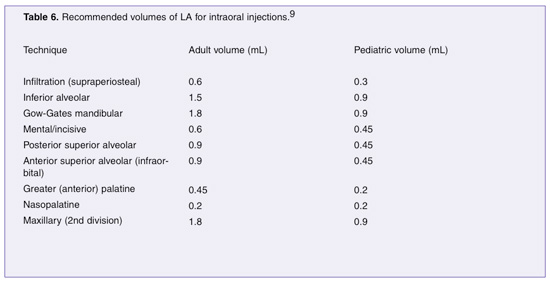
(1) Treatment plan. In interviews with trained pediatric dentists, I have found that when presented with the patient described above (young, light-weight, well-behaved), the pediatric dentist will not treat all 4 quadrants at one visit using LA. Limiting treatment to 1 or 2 quadrants per visit represents a more rational approach to this patient’s needs, and increased safety.
(2) Choice of LA. In most instances where serious LA overdose has occurred in children, the LA administered has been a “plain” drug, either mepivacaine HCl 3% or prilocaine HCl 4%. Both of these are excellent LAs when used properly. The rationale behind the clinician’s selection of a short-acting drug for children includes: (a) most pediatric appointments are of short duration, and (b) plain LAs have a shorter duration of posttreatment soft tissue anesthesia, minimizing the likelihood of inadvertent soft tissue injury as the child bites or chews his/her numb lip or tongue.
(3) Volume of LA administered. Pain control for the entire primary dentition can be achieved with approximately 2 cartridges of LA. In the child patient, there is never a compelling reason to administer a full 1.8 mL cartridge of LA for any 1 injection. Yet, when children receive LA administered by nonpediatric dentists, full cartridges tend to be routinely administered. In many of the instances where death resulted, a total of 5, 6, or 7 cartridges were administered.8
(4) LA administered to all 4 quadrants at one time. The administration, over 1 or 2 minutes, of 4 or more cartridges of a LA without a vasopressor to all 4 quadrants makes little therapeutic sense, while increasing the likelihood of an overdose. Administration of LA to one quadrant, treating that area, then anesthetizing the next quadrant, and so on, makes considerably more sense both from a therapeutic and safety perspective. For equal amounts of LA, administration over a longer timeframe (1 to 2 hours) will result in a lower blood level of the LA as compared to the entire dose being administered at one time.
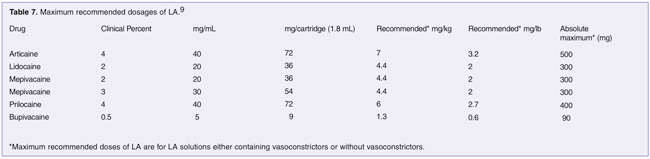
(5) Exceeding the maximum dosage based on patient’s body weight. An important factor, especially when managing younger, lighter-weight patients, is maximum dosage. Determine the weight of the patient (in pounds [lb] or kilograms [kg]) prior to the start of treatment. It is preferable to weigh the child on a scale, as parents frequently can offer only a rough estimate of the child’s weight.
CONCLUSION
LAs are the foundation of pain control in dentistry and are used to reversibly block peripheral nerve conduction. It must always be remembered that all drugs have the potential to do harm. All dentists and hygienists permitted to administer LAs must be aware of these potential problems and be prepared to manage them expeditiously and effectively.
References
- Malamed SF. What’s new in local anaesthesia: dentistry’s first line in pain control. Independent Dentistry. 2001;4:43-46.
- Haas D, Lennon D. Local anesthetic use by dentists in Ontario. J Can Dent Assoc. 1995;61:297-304.
- Jastak JT, Yagiela JA, Donaldson D. Local Anesthesia of the Oral Cavity. Philadelphia, Pa: Saunders; 1995.
- Haas DA. An update on local anesthetics in dentistry. J Can Dent Assoc. 2002;68:546-551.
- Malamed SF, Gagnon S, Leblanc D. Articaine hydrochloride: a study of the safety of a new amide local anesthetic. J Am Dent Assoc. 2001;132:177-185.
- Shojaei AR, Haas DA. Local anesthetic cartridges and latex allergy: a literature review. J Can Dent Assoc. 2002;68:622-626.
- Malamed SF. Morbidity, mortality and local anaesthesia. Primary Dental Care. 1999;6:11-15.
- Finder RL, Moore PA. Adverse drug reactions to local anesthesia. Dent Clin North Am. 2002;46:747-757.
- Malamed SF. Handbook of Local Anesthesia. 4th ed. St Louis, Mo: C.V. Mosby Inc; 1997:191, 218, 265.
- Malamed SF. Report of a case. Unpublished data. 2002.
- Malamed SF. Handbook of Medical Emergencies in the Dental Office. 5th ed. St. Louis, Mo: C.V. Mosby Inc; 2000:51-52.
Dr. Malamed is a professor of anesthesia and medicine at the School of Dentistry at the University of Southern California.












