The differential diagnoses for an asymptomatic cyst-like radiolucent lesion of the anterior mandible include radicular cyst, focal periapical cemental dysplasia type I (cementoma), residual cyst, odontogenic keratocyst, central giant cell granuloma, lateral periodontal cyst, amelo-blastoma, primordial cyst, odontogenic myxoma, hemangioma, clear cell odontogenic carcinoma, anterior lingual mandibular salivary gland defect, and labial and/or lingual bone concavity/depression.1-7 The lesions that are listed as part of the differential diagnosis all can have a unilocular radiolucent radiographic appearance with an asymptomatic clinical history.
Giunta1 recently reported 4 cases of labial bone concavities. Bone concavities can be mistaken radiographically for pathology, and as such clinicians should include them within the differential diagnosis. In the area of the apparent radiographic lesion, the bone is thinned and appears more radiolucent than the adjacent bone. Concavities are noted primarily in the anterior mandible but also in the anterior maxilla. Radiographically, bone concavities may appear as defined radiolucencies, similar to a cyst, or with a ground-glass pattern, similar to a fibro-osseous disease. Their presence may be due to a congenitally missing tooth, a prominent canine fossa (due to anatomy or to a missing tooth), a malposed tooth, an anatomical variation, or a surgical defect. Once the diagnosis is made, no further treatment is recommended.1,3-6
Giunta1 describes labial bone concavities of either the mandible or maxilla as an indentation or depression of the labial bone that may produce radiolucencies that can be mistaken for disease. He further elaborates that because this condition is relatively common (although incidence or prevalence data do not exist at the present time), dentists should include this condition within the differential diagnosis of radiologic radiolucent entities. This condition is similar to the more noted Stafne’s bone defect, but that particular lesion is usually located in the lingual posterior inferior mandible, and salivary gland tissue fills the area of the depression. Furthermore, Stafne8 in his original article alluded to anatomical thinning of the anterior labial mandible below the incisor teeth, which may appear as a radiolucent lesion.
Philipsen, et al4 described a number of variations of bony jaw depressions. He and his colleagues advocated the term of either lingual or buccal mandibular bone depressions. They also noted that these “lesions” may be located in the area of the posterior lingual mandibular ramus (as described by Stafne), anterior lingual mandible, and rarely on the buccal aspect of the ascending mandibular ramus. Philipsen, et al4 concluded that all of these variants have a common origin, which is described as hyperplastic/hypertrophic lobes of either the sublingual, submandibular, or parotid salivary glands. Therefore, the difference between Giunta’s1 labial bone concavities and Philipsen, et al4 and Stafne’s8 bone defects is the absence or presence of salivary gland tissue.
In this report, a case is presented in which the radiolucency was detected after orthodontic repositioning to enhance implant placement. With the increased popularity of implant therapy, inevit-ably there will be more clinical situations where it will be important for the clinician to include bone concavity within the differential diagnosis.
CASE REPORT
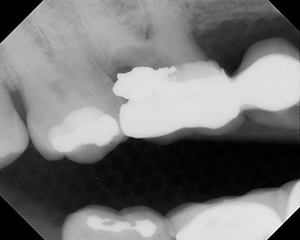
| Figures 1a and 1b. Periapical radiographs demonstrate a spherical radiolucent lesion, which appears to be associated with the apical area of the tooth root. |
| Figure 2a. Periapical radiograph demonstrates that the radiolucent lesion is superior to the root apex. Figure 2b. Periapical radiograph demonstrates the radiographic appearance at the initiation of therapy. |
A 34-year-old African American female was referred to an oral medicine private practice for consultation regarding a radiographic lesion. The medical history was not contributory to the chief complaint, and the patient was in apparent good health. The chief complaint was “suspicious area on lower tooth.” There were no symptoms. The patient was undergoing orthodontic therapy to reposition her teeth to enhance implant placement for a missing mandibular left lateral incisor. The radiographic lesion was found on a routine dental radiographic series in March of 2002. Clinically, there was no lymphadenopathy nor other clinical signs or symptoms. The radiographs (Figures 1a and 1b) revealed a well-defined/demarcated but not well-corticated radiolucent cyst-like apical lesion of the mandibular left central incisor. The inferior aspect of the lesion was at the level of the root apex. The right mandibular cuspid tested vital, as did the left mandi-bular central incisor (the tooth in question). All other hard and soft oral tissues ap-peared to be within normal limits.
Due to the patient’s history, clinical evaluation, and ethnicity, the working diagnosis was focal periapical cemental dysplasia stage I (cementoma). The differential diagnosis included radicular cyst, residual cyst, primordial cyst, odontogenic keratocyst, central giant cell granuloma, odontogenic myxoma, lateral periodontal cyst, ameloblastoma, gingival cyst, clear cell odontogenic carcinoma, anterior lingual mandibular salivary gland defect, and labial and/or lingual bone concavity/depression. The patient was referred back to her dentists with instructions to keep the lesion under observation.
Shortly afterward, the patient’s periodontist called and suggested that the working diagnosis of focal periapical cemental dysplasia type I was probably incorrect because the lesion was coronal to the apical area of the tooth (Figure 2a). Radiographs taken one year ago did not demonstrate a lesion (Figure 2b). Therefore, it was suggested that a biopsy of the lesion was needed to ascertain a diagnosis. The area was surgically explored, and a specimen was submitted. The microscopic evaluation reported normal periosteum and connective tissue. The surgical report noted no obvious pathologic findings. However, the periosteum of the labial bone demonstrated only an extremely thin amount of tissue over the tooth root. Therefore, the diagnosis was changed to labial bone concavity. As the area of thinned bone was now in the area of the tooth, the implant site appeared to have sufficient space. However, it was recommended that diagnostic radiography be utilized for preoperative measurements to en-sure that adequate space was available for implant placement.
DISCUSSION
The patient in the present case was being treated for a missing mandibular left lateral incisor tooth, which resulted in spaces between the mandibular central incisors and between the mandibular left central incisor and the mandibular left canine. The treatment plan was to orthodontically reposition the mandibular left central incisor medially adjacent to the mandibular right central incisor, which would re-establish the space of the missing mandi-bular left lateral incisor. Once the space was created, the plan called for placement of an implant. However, the radiographic appearance of an apparent lesion necessitated further inquiry. It appeared that the movement of a tooth into an area of thinned bone produced a radiographic appearance consistent with a cystic lesion.
The presence of a mandibular labial bone concavity complicates the implant procedure, as greater imaging and possible bone grafting must be considered. How-ever, with knowledge of this condition, imaging through tomographs or computed axial tomography (CT) can allow a measurement of available space and a determination of the need for an augmentation. The resultant measurements will determine what size implant is suitable for the available space.
Labial bone concavity, lingual/buccal mandibular bone depressions, anterior lingual mandibular salivary gland defect, and Stafne’s bone concavity in the anterior man-dible appear to be similar in that these conditions tend to be asymptomatic and are discovered only upon radiographic examination.1-7 Katz, et al6 reported a well-delineated radiolucent finding inferior to a mandibular second premolar and named the entity Stafne’s bone cavity in the anterior mandible. However, a biopsy procedure was not performed, and the area was evaluated through panoramic and CT radiography. No salivary gland tissue was observed. However, de Courten, et al5 had a similar finding and performed a biopsy that demonstrated the presence of salivary gland tissue between the area of the mandibular premolar and first molar. Therefore, they demonstrated that the concavity was due to the presence of salivary gland tissue.
In a much larger review, Philipsen, et al4 reported on 583 cases of asymptomatic mandibular radiolucent depressions. Of these, the vast majority (497/583) were in the lingual posterior region and were consistent with the entity first reported by Stafne.8 They reported that lingual anterior lesions represented 72 of 583 cases, lesions of the lingual ramus represented 13 of 583, and lesions of the buccal ramus represented only 1 of 583 cases. These lesions were noted for the presence of salivary gland tissue and appeared to be developmental in that the lesions rarely occurred in children and never before the age of 10. These lesions tended to occur much more often in men as compared to women, with an approximate 6-to-1 ratio.
Furthermore, Philipsen, et al4 reviewed previous re-ports related to buccal anterior mandibular depressions. Although this entity was first reported in 1858,4 the first detailed reports appeared in 1984 and 1989 by Cataldo and Giunta3 and Arensburg, et al.9 Giunta1 reported 3 males and 6 females with a labial bone concavity. Of these cases, 6 were in the mandible and 3 were in the maxilla. Arensburg, et al9 utilized a composite cadaver collection of 970 assorted dried mandibles of children and adults of various ethnic origins, geographic regions, and time periods, and described a buccal anterior mandibular depres-sion. In their sample, they noted an incidence of 13.5% buccal anterior bone depressions that were definitively present and 23.5% reported as vestigial.
Utilizing the same cadaver mandibles, Kaffe, et al10 reported an incidence of 19.8% for mandibular buccal anterior depressions with no gender differences. Furthermore, they described an incidence of mandibular buccal anterior bone depressions that was higher in children compared to adults. They reported that these buccal (or labial) anterior depressions tended to decrease with age, while lingual bone concavities tended to increase with age, and that buccal (or labial) anterior depressions appeared to be distinctly different from lingual anterior bone depressions. (It was previously noted that lingual mandibular depressions are caused by infiltrating salivary gland tissue, while anterior mandibular depressions are not caused by salivary gland tissue.) Littner, et al11 noted that mandibular anterior bone depressions are significant when evaluating edentulous patients for implant placement. When evaluating mandibular anterior depressions, CT scans are superior to conventional dental radiology such as panoramic or periapical radiographs.
CONCLUSION
This case illustrated a labial bone concavity in the anterior mandible. There was a large list of lesions that comprised the differential diagnosis. Exploratory surgery to biopsy the apparent lesion indicated a diagnosis of man-dibular labial bone concavity. This condition is an anatomical variation and may have significant implications for implant dentistry.
References
- Giunta JL. Labial bone concavity. J Mass Dent Soc. 2002;51:24-26.
- Kanas RJ, DeBoom GW, Jensen JL. Inverted heart-shaped, interradicular radiolucent area of the anterior maxilla. J Am Dent Assoc. 1987;115:887-889.
- Cataldo E, Giunta JL. A clinico-pathologic presentation. Labial bone concavity. J Mass Dent Soc. 1984;33:56.
- Philipsen HP, Takata T, Reichart PA, et al. Lingual and buccal mandibular bone depressions: a review based on 583 cases from a world-wide literature survey, including 69 new cases from Japan. Dentomaxillofac Radiol. 2002;31:281-290.
- de Courten A, Kuffer R, Samson J, et al. Anterior lingual mandibular salivary gland defect (Stafne defect) presenting as a residual cyst. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:460-464.
- Katz J, Chaushu G, Rotstein I. Stafne’s bone cavity in the anterior mandible: a possible diagnostic challenge. J Endod. 2001;27:304-307.
- Giunta JL. Gingival cysts in the adult. J Periodontol. 2002;73:827-831.
- Stafne EC. Bone cavities situated near the angle of the mandible. J Am Dent Assoc. 1942;29:1969-1972.
- Arensburg B, Kaffe I, Littner MM. The anterior buccal mandibular depressions: ontogeny and phylogeny. Am J Phys Anthropol. 1989;78:431-437.
- Kaffe I, Littner MM, Arensburg B. The anterior buccal mandibular depression: physical and radiologic features. Oral Surg Oral Med Oral Pathol. 1990;69:647-654.
- Littner MM, Kaffe I, Arensburg B, et al. Radiographic features of anterior buccal mandibular depressions in modern human cadavers. Dentomaxillofac Radiol. 1995;24:46-49.
Acknowledgement
The authors wish to thank Dr. Neil Sushner for referral of the patient for the initial work-up.
Dr. Farquharson is an assistant professor in the department of oral diagnostic services at Howard University College of Dentistry, Washington, DC. He can be reached at afarquharson@howard.edu.
Dr. Brown is a professor in the department of oral diagnostic services, Howard University College of Dentistry, and a clinical associate professor in the department of otolaryngology, Georgetown University Medical Center, Washington, DC. He can be reached at rbrown@howard.edu.
Dr. Haynes is an assistant professor in the department of orthodontics, Howard University College of Dentistry, Washington, DC. She can be reached at (202) 806-0365 or ejhaynes@howard.edu.
Dr. Kaufman maintains a private practice in periodontics in Washington, DC. He can be reached at (202) 223-2211 or dcperio@aol.com.