Temporomandibular disorders (TMDs) include a number of clinical problems that involve the masticatory musculature, the temporomandibular joint, and associated structures.1 They are considered to be a subclassification of musculoskeletal disorders. Detailed history taking and standardized examination techniques are crucial in forming a proper differential diagnosis. The patient may present with jaw ache, earache, toothache, facial pain, and/or headache; however, the chief complaint may be as benign as a general facial tightness or fatigue. Treatment planning is dependent on various factors such as the chief complaint, health history, presenting symptoms, examination, and diagnosis. In the past, TMD cases have sometimes been regarded as problematic to diagnose and difficult to treat; however, with continuing research in orofacial pain and pain management, clinicians are able to use specific diagnostic methods and standardized classification systems to offer patients treatment modalities with higher success rates. In part 1 of this 2-part series on TMD, emphasis will be placed on the history, epidemiology and classification of TMD, structure and function of the temporomandibular joint (TMJ), and patient evaluation techniques.
HISTORY AND EVOLUTION OF THE MANAGEMENT OF TMD (TABLE 1)
| Table 1: History of the clinical management of temporomandibular disorders | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
As a result of Costen’s work, awareness of the TMJ and its relationship to facial pain increased greatly among practitioners.2 He noted that a number of his patients with pain in the TMJ region seemed to experience a reduction of symptoms following therapeutic alteration in their occlusion. These findings were significant on 2 fronts. Firstly, Costen’s writings introduced hypotheses that occlusion and TMD may be linked. Secondly, he emphasized the practitioner’s role in providing treatments aimed at affecting the TMJ region. Thus, in the first half of the century, generally accepted concepts of patient management focused on occlusal adjustment as the major treatment modality for TMD.3-7
| Table 2. Possible etiological factors in the development of temporomandibular disorders. |
| •Stress •External trauma •Bruxism •Systemic polyjoint arthritis •Hypermobility disorder •Neoplasia •Developmental/growth abnormality •Dental morphologic abnormality •Daytime habitual behavior •Infection •Idiopathic |
The concept of internal derangement of the TMJ was introduced by Ireland15 in 1953 but was not widely accepted until the 1970s, following imaging techniques such as arthrography. Also in the late 1970s and 1980s, surgical intervention with disk repositioning started gaining popularity. Subsequently, TMJ disk removal procedures were recomended, with some surgeons choosing to maintain the joint complex without a disk while others opted for prosthetic TMJ disk implant placement. Unfortunately, use of certain prosthetic implants such as Vitek proplast/teflon resulted in severe complications such as giant cell foreign body reactions. In some implant cases, this led to extremely painful joint conditions with limited range of motion (ROM). Less-invasive surgical techniques such as arthrocentesis and arthroscopy proved to be highly effective for chronic TMJ conditions (eg, unresolving joint pain and closed lock).16-18
 |
 |
|
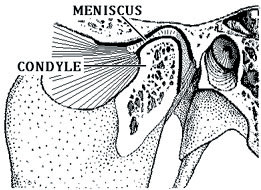
Figure 1. Structure of the temporomandibular joint. |
Figure 2. Palpating the temporalis muscle.
|
 |
 |
|
Figure 3. Palpating the superficial and deep masseter muscles.
|
Figure 4. Bilateral palpation of the TMJs.
|
 |
 |
|
Figure 5. Evaluating mandibular range of motion using a millimeter ruler.
|
Figure 6. A crude measure of reasonably normal interincisal distance is approximately the width of 3 of the patient’s fingers.
|
STRUCTURE AND FUNCTION (FIGURE 1)
TMJ has been a source of interest since the fifteenth century, when this anatomical structure was studied by Leonardo da Vinci. Other notable contributors include Vesalius in the sixteenth century, Meyers in the nineteenth century, and Sicher19 and Rees20 in the early twentieth century. The TMJ has been described as a ginglymoarthrodial synovial compound paired joint. A compound joint consists of 3 bones; however, in the case of the TMJ, the functional disk operates as the third nonossified bone and therefore fulfills the criteria. As a synovial joint, it is governed by the same basic orthopedic principles that apply to other human synovial joints, ranging from pathologic disorders to treatment protocols. The TMJ, however, has many unique features that distinguish it from other synovial joints. These include (1) rigid end point of closure; (2) one side cannot function without movement of the opposite joint; (3) both joints act as one functional unit; (4) any movement or functional alteration in one joint will affect the other joint; and (5) no hyaline cartilage is present.
NATURAL HISTORY AND EPIDEMIOLOGY
In a study on symptoms associated with TMD, Rasmussen21 found that most patients with a clicking TMJ usually did not evolve into an open or closed locking state. According to his findings, acute TMD symptoms lasted a mean of 5 years, and although joint noises generally did not disappear, most painful and disabling symptoms subsided in time. Similar results were shown by Könönen and colleagues, who followed 128 Finnish adults over 9 years.22 They found that the incidence of clicking in these patients increased with age. However, none of the patients developed locking. These studies demonstrate the importance of reversible and noninvasive treatments for the acute TMD patient. In an epidemiological study by Solberg,23 76% of subjects aged 18 to 25 had one or more signs associated with TMD and 26% had at least one symptom associated with TMD. Of this group, only 10% had symptoms that were considered by the subjects to be severe enough to seek treatment.
CLASSIFICATION (TABLES 3 AND 4)
| Table 3. Classification of temporomandibular disorders. |
|
1. Articular 2. Muscular |
Internal Derangement (ID)
Internal derangement of the TMJ is characterized by an anatomical disturbance in the relationship of the components of the disk-condyle complex. This term encompasses a number of clinical entities, including the following:
| Table 4. Inflammatory joint disorders Osteoarthrosis |
|
Osteoarthritis |
Inflammatory Joint Disorders
Arthralgia: This describes a joint that displays increased tenderness on palpation. Osseous changes are usually not noted on radiographic examination. Various terms have been used to specifically characterize this condition depending upon the location of the pain (eg, capsulitis, retrodiscitis, and synovitis).
Muscular Disorders
Myalgia/Myofascial Pain (MFP): This is a dull, aching pain varying in intensity. The primary difference between MFP and myalgia is that MFP produces pain referred to other satellite muscle trigger points upon palpation, whereas myalgia results in pain that is localized to the muscle that is being palpated. MFP tends to be seen in more chronic muscle pain conditions compared to the usually acute presentation of myalgia. Palpation of the trigger points should duplicate the patient’s pain complaint, thus confirming the diagnosis. In addition, blocking the source of the pain (ie, masseter muscle) utilizing a vapo-coolant spray or local anesthetic injection can also provide a definitive diagnosis.
PATIENT EVALUATION
TM disorder assessment should include a general examination of the head and neck, a detailed examination of the masticatory muscles, an evaluation of the temporomandibular joints, an evaluation of mandibular range of motion, and a detailed intraoral examination.24
Evaluation of the Muscles of Mastication
The muscles of mastication are palpated bilaterally for firmness and tenderness utilizing approximately 2 to 3 pounds of pressure. A pain pressure algometer may be used to reproduce reliable palpation pressure25 or the amount of pressure needed to cause blanching of the fingernail. Upon muscle palpation, the patient is asked to report the severity of the tenderness, pain referral to multiple sites or single-site pain localization, and replication of the chief complaint. The primary muscles to be palpated include the temporalis (Figure 2), the superficial and deep masseter (Figure 3), the medial and lateral pterygoid, the suprahyoid, and the upper cervical muscles. Note that palpation of the lateral pterygoid from an intraoral perspective is difficult.26 It may be pertinent to ask patients about their use of analgesic prior to palpation in order to account for reduced symptoms upon examination.
Evaluation of the TMJ
The TMJs are palpated bilaterally for tenderness or swelling with slightly less pressure than used for muscle palpation, especially in the presence of an existing capsulitis (Figure 4). The clinician should palpate the preauricular region as well as the anterior walls of the external auditory canal. Lateral palpation may be utilized to assess joint pain in the lateral capsule, whereas the intrameatal approach via the external auditory canal is better for locating pain emanating from retrodiscal tissues.1
Evaluation of Mandibular Range of Motion (ROM)
Initially, patients’ opening and closing patterns are closely observed to note any mandibular deviations. Evaluation of mandibular ROM consists of measuring with a millimeter ruler the (1) comfort opening, (2) active opening, (3) passive opening, (4) protrusion, and (5) left and right lateral excursions while noting the severity and location of pain with jaw movement (Figure 5). This can be particularly helpful in differentiating between joint and muscle pain. Comfort opening is determined by (1) the patient opening as wide as possible without any pain, (2) active opening with the patient opening as wide as possible with pain, and (3) passive opening with the clinician gently stretching the patient presumably past active opening while noting a soft or hard end feel. A reasonably normal interincisal distance is approximately 40 mm or the width of 3 of the patient’s fingers as a crude measure (Figure 6). Usually, with proper questioning, the patient will reliably reveal any recent limitations in ROM. The occurrence of TMJ clicking, crepitus, or jaw opening interferences with or without pain should also be noted at the initial examination. These baseline findings will aid in establishing the differential diagnosis and treatment options as well as providing a comparison for future change in TMD symptoms.
Evaluation of the Cervical Spine
Often, patients who present with TMD may have a coexisting pain complaint in the neck, shoulder, or upper back region. Poor posture may lead to a forward head position, rounded shoulders, and/or added tension in the head, neck, or back. Thus, an evaluation of the cervical spine may aid in assessing the patient’s head ROM in flexion, extension, and rotation. In addition, if range of motion is limited, it is pertinent to note any areas of pain that the patient experiences while performing various head and neck movements. This may help in localizing additional trigger areas that may have been missed on the palpatory exam.
SUMMARY
The study of temporomandibular disorders has undergone many changes throughout its history. Focus on the structure and function of the TMJ continues to improve our understanding of these complex disorders. A more standardized classification system allows practitioners and researchers to discuss findings in a common language. With improved patient evaluation techniques, the clinician can establish a proper working differential diagnosis and begin focusing attention on treatment planning.
References
- Okeson JP. Orofacial Pain: Guidelines for Assessment, Diagnosis, and Management. Chicago, Ill: Quintessence Publishing; 1996.
- Costen JB. A syndrome of ear and sinus symptoms dependent upon disturbed function of the temporomandibular joint. Ann Otol Rhinol Laryngol. 1934;43:1-15.
- McCollum BB. Factors that make the mouth and teeth a vital organ (articulation orthodontia). J Am Dent Assoc. 1927;14:1261-1271.
- Stallard H. Functions of the occlusal surfaces of the teeth. J Am Dent Assoc. 1930;13:401.
- Stuart CE, Golden IB. The History of Gnathology. Ventura, Calif: CE Stuart Gnathological Instruments; 1981.
- Shore N. Temporomandibular Joint Dysfunction and Occlusal Equilibration. Philadelphia, Pa: JB Lippincott; 1976.
- Ramfjord SP. Dysfunctional temporomandibular joint and muscle pain. J Prosthet Dent. 1961;11:353-374.
- Travell J, Rinzler SH. The myofascial genesis of pain. Postgrad Med. 1952;11:425-434.
- Schwartz LL. A temporomandibular joint pain dysfunction syndrome. J Chronic Dis. 1956;3:284-293.
- Laskin DM. Etiology of the pain-dysfunction syndrome. J Am Dent Assoc. 1969;79:147-153.
- Wilkes CH. Arthrography of the temporomandibular joint in patients with the TMJ pain-dysfunction syndrome. Minn Med. 1978;61:645-652.
- Farrar WB. Diagnosis and treatment of anterior dislocation of the articular disk. N Y J Dent. 1971;41:348-351.
- Farrar WB, McCarty WL. A Clinical Outline of Temporomandibular Joint Diagnosis and Treatment. Montgomery, Ala: Normandie Study Group Publications; 1982.
- Rugh JD, Solberg WK. Psychological implications in temporomandibular pain and dysfunction. Oral Sci Rev. 1976;7:3-30.
- Ireland VE. The problem of the clicking jaw. J Prosthet Dent. 1953;3:200-212.
- Ohnishi M. Clinical application of arthroscopy in the temporomandibular joint diseases. Bull Tokyo Med Dent Univ. 1980;27:141-150.
- Sanders B. Arthroscopic surgery of the temporomandibular joint: treatment of internal derangement with persistent closed lock. Oral Surg Oral Med Oral Pathol. 1986;62:361-372.
- Nitzan DW, Dolwick MF, Martinez GA. Temporomandibular joint arthrocentesis: a simplified treatment for severe, limited mouth opening. J Oral Maxillofac Surg. 1991;49:1163-1167.
- Sicher H. Temporomandibular articulation in mandibular overclosure. J Am Dent Assoc. 1948;36:131-139.
- Rees LA. The structure and function of the temporomandibular joint. Br Dent J. 1954;96:125-133.
- Rasmussen OC. Description of population and progress of symptoms in a longitudinal study of temporomandibular arthropathy. Scand J Dent Res. 1981;89:196-203.
- Kononen M, Waltimo A, Nystrom M. Does clicking in adolescence lead to painful temporomandibular joint locking? Lancet. 1996;347:1080-1081.
- Solberg WK, Woo MW, Houston JB. Prevalence of mandibular dysfunction in young adults. J Am Dent Assoc. 1979;98:25-34.
- Clark GT, Seligman DA, Solberg WK, et al. Guidelines for the examination and diagnosis of temporomandibular disorders. J Craniomandib Disord. 1989;3:7-14.
- Ohrbach R, Gale EN. Pressure pain thresholds, clinical assessment, and differential diagnosis: reliability and validity in patients with myogenic pain. Pain. 1989;39:157-169.
- Johnstone DR, Templeton M. The feasibility of palpating the lateral pterygoid muscle. J Prosthet Dent. 1980;44:318-323.
Dr. Uyanik completed his DDS degree at SUNY Buffalo School of Dental Medicine and then went on to a 2-year post-
doctoral residency program in orofacial pain at UCLA. Upon completion of his post-doctoral training, he obtained board certification from the American Board of Orofacial Pain and is currently a member of the house staff at St. Barnabas Hospital working with residents in the diagnosis and treatment of orofacial pain disorders. He was recently appointed as clinical assistant professor at Columbia School of Dental and Oral Surgery in the Division of Oral and Maxillofacial Surgery as well as director of the Center for Oral, Facial and Head Pain. Dr. Uyanik is currently investigating the effects of low-level diode laser therapy on TMJ arthralgia and myofascial pain syndrome.
Dr. Murphy currently works in private practice in Cork, Ireland. He is a part-time lecturer in the Anatomy Department and Dental School in University College Cork and the Eastman Dental Institute in London, England. He graduated from the UCLA orofacial pain residency programin 2001 and also completed a master of science in oral biology. He is a diplomate of the American Board of Orofacial Pain. His private practice is exclusive to orofacial pain and temporomandibular disorders.









