INTRODUCTION
Osteomyelitis (OM) is an inflammatory condition of bone that involves the medullary cavity and the adjacent cortex. It occurs more frequently in mandible than in the maxilla and is often associated with suppuration and pain.1 The osseous spaces are usually filled with exudates that can lead to pus formation. Chronic osteomyelitis can be the result of a non-treated acute mild inflammation or emerge without a precursor. When osteomyelitis occurs in the mandible, it is usually more diffused and widespread.1-6 Clinical examination alone is often enough to diagnose chronic mandibular osteomyelitis due to the progression of this disease and suppuration.1,2 In cases of chronic osteomyelitis, a radiolucent circumscribed image can be seen encapsulating central radiopaque sequestra, as well as radiopacities of the surrounding bone due to a local osteogenic reaction.7 Patients who present active chronic osteomyelitis usually require long-term use of antibiotic therapy and surgical intervention.7 Treatment requires both antibiotic therapy and surgical debridement, meaning the necrotic bone must be completely removed until the underlying bone starts bleeding.7 Although most cases of OM of the jaws result from dental origins, other sources of infection are possible.2 Although primary OM following extraction of periodontally involved teeth is rare, it is, however, of concern to both the patient and dentist. The following case report describes the presentation of OM and how it was managed.
|
CASE REPORT
A 62-year-old woman referred to our clinic for treatment of chronic infection and pain following extraction of the left mandibular second molar under local anesthesia by her general dentist. She was in good general health and did not have a history of drug use. Her pre-extraction radiographic examination confirmed the presence of a deep distal periodontal pocket (Figure 1). She then developed pain, chronic infection, and discharge following the extraction (Figure 2). She returned to her general dentist who prescribed amoxicillin 500 mg every 8 hours for 10 days. After multiple visits to her dentist, and no abatement of her symptoms after 5 months, she was referred to our clinic.
Intraoral clinical examination revealed that the socket of the left mandibular second molar tooth had chronic infection and a malodorous discharge. A sample of this fluid was collected for culture and antibiotic sensitivity. Culture was positive for non-A non-D streptococci sensitive to cephalexin. Radiographic examination confirmed the presence of a sequestrum in the socket (Figure 3).
Considering the clinical and radiographic presentation, a diagnosis of chronic osteomyelitis was made and the patient was scheduled for surgery. After general anesthesia, preparation, draping and packing the oropharynx; a flap was reflected and the sequestrum was removed with a curette. The socket was cleaned and irrigated. Nonvital necrotic bone was shaved using a round bur until vital bone was apparent (confirmed clinically by bone bleeders). The lesion was sent to the pathology laboratory and their report confirmed the diagnosis of chronic osteomyelitis. The patient was given cephalexin and metronidazole 500 mg every 6 hours for 2 weeks. A radiograph was that taken 3 months postoperatively showed bony consolidation of the socket (Figure 4). The patient has been symptom-free since the completion of the surgical treatment and antibiotic regimen.
DISCUSSION
Osteomyelitis may result from the direct extension of pulpal or periodontal infection without the formation of a granuloma or from acute exacerbation of a periapical lesion. It may also occur following penetrating trauma or various surgical procedures. Extension of the infection into adjacent soft tissue and fascial spaces is common, and often the presenting clinical symptoms are swelling, pain and suppuration. Sequelae to transcortical extension of the inflammatory process can include cortical destruction, fistulization and periosteal reaction. These changes can be evaluated by imaging techniques.5
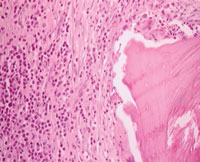
Histopathology.The bone pathology presents various forms, depending on the virulence of the infecting microorganism, the host capacity of effective immune response and the kind of reaction of the periosteal and osseous tissues. Chronic osteomyelitis histopathology depicts irregular fragments of devitalized bone surrounded by dense fibrous tissue heavily infiltrated by plasma cells, lymphocytes, and only a few granulocytes (Figure 5).
Imaging.Appropriate evaluation of radiographic types of osteomyelitis is necessary for treatment planning. Kazunori Yoshiura6 classified mandibular osteomyelitis into four basic patterns, as lytic, sclerotic, mixed and sequestrum patterns. Our case presented with the latter pattern. In some cases computerized tomography or scintography may be necessary.1
Presentation.Patients can have swelling of the face, tenderness and pain (localized), draining sinus tracts, suppuration, tooth loss, possible necrotic bone fragment formation, and a low-grade fever. New bone and oral mucosa will occasionally regenerate beneath the sequestra, probably because of activation of periosteal osteoblasts. According to Reinert,6 clinical examination alone can be enough to diagnose mandibular chronic osteomyelitis, particularly at the onset of the disease. The radiographic characteristics of the osteomyelitis presented were a radiolucent area circumscribing a central bone sequestrum and radiopacity in the surrounding bone. Due to the characteristics of the pathology and the clinical history, there was no need for other exams.
Predisposing factors. Viral fevers (eg, measles), malaria, anemia, malnutrition, and use of tobacco are found to contribute to the development of osteomyelitis.
Management.Treatment goals include reversal of any predisposing conditions, long-term antibiotic therapy. Antibiotic therapy alone is not enough for the treatment of osteomyelitis, since the devitalized osseous tissue in combination with the capsule of the surrounding fibrous connective tissue protects the microorganisms from the drug action. Corticotomy can be used as treatment, and if not effective, bone resection can be done as a more radical alternative. However, aggressive treatment may cause loss of function, exposure of the inferior alveolar nerve and problems regarding the reconstruction.7 High doses of antibiotics should accompany any aggressive surgical treatment. Some authors feel that penicillin G is the medication of choice, followed by clindamycin.7 Since most of the osteomyelitis infections are polymicrobial oral flora (primarily facultative streptococci, Bacteroides spp, Peptostreptococcus, and Peptococcus), antibiotic treatment includes penicillin, metronidazole, and clindamycin. Operative interventions such as sequestrectomy, decortication, removal of nonviable bone (ie, mandibulectomy or maxillectomy), and dental extractions, are also needed. A wide incision to remove all the diseased tissue, as well as primary closure of the surgical wound is performed to ensure a successful operation.7
SUMMARY
This article describes the presentation of OM, and presented a case report that outlined patient treatment and outcome.
REFERENCES
-
- Taori KB, Solanke R, Mahajan SM, Rangankar V, Saini T. CT evaluation of mandibular osteomyelitis. Indian J Radiol Imaging. 2005;15:447-451
- Eyrich G, Baltensperger M, Bruder E, Graetz K. Primary chronic osteomyelitis in childhood and adolescence. A retrospective analysis of 11 cases and review of the literature. J Oral Maxillofac Surg. 2003;61:561-573.
- Schultz C, Holterhus P, Seidel A, Jonas S, Barthel M, Kruse K.Chronic recurrent multifocal osteomyelitis in children. Pediatr Infect Dis J. 1999;18:1008-1013.
- Job-Deslandre C, Krebs S, Kahan A. Chronic recurrent multifocal osteomyelitis: Five-years outcomes in 14 patients cases. J Bone Spin. 2001;64:245-251.
- Lavis JF, Gigon S, Gueit I, Michot C, Tardif A, Mallet E. Chronic recurrent multifocal osteomyelitis of the mandible. A case report. Arch Pediatr. 2002;9;1252-1255.
- Reinert S, Widlitzek H, Venderink DJ. The value of magnetic resonance imaging in the diagnosis of mandibular osteomyelitis. Br J Oral Maxillofac Surg. 1999;37:459-463.
- Pozza DH, Neto NR, Sobrinho JB, Santos JN, Weber JB, de Oliveira MG. Combined treatment by antibiotic therapy and surgery of chronic mandibular osteomyelitis: a case report. R Ci méd boil. 2006:5;75-79.
BIOS
Dr. Motamedi is a professor, OMS clinic and Trauma Research Center, Baghyatoolah Medical Sciences University (BMSU), Tehran, Iran. He can be reached atmotamedical@lycos.com.
Dr. Shams, DMD is an assistant professor, OMS clinic, Baqiyatallah Medical Sciences University, Tehran, Iran.
Dr. Azizi is an assistant professor, pathology department, Baqiyatallah Medical Center, BMSU, Tehran, Iran.
Dr. Ardakani is at the Hospital Dentistry, Dental Clinic, Baqiyatallah Medical Center, BMSU, Tehran, Iran.