INTRODUCTION
The need for endodontic care during the COVID-19 pandemic has remained as important as ever. But as we face unprecedented clinical challenges due to this ongoing pandemic, we must adjust our practices by adopting certain protocols. This article will discuss how to adapt to COVID-related considerations that center around efficient and effective endodontic treatment and the reduction of viral transmission risks in the dental office.
COVID-related patient management and facility considerations should be followed as per your regulatory body’s guidelines. This should include consideration of the Centers for Disease Control and Prevention (CDC) and ADA guidances.1,2
Mitigating transmission risks obviously includes the use of barriers such as personal protective equipment (PPE), as per current guidelines.1,2 But it may also include enhanced patient screening, triage, and diagnosis; reducing the number of visits required to perform endodontic treatment; reducing patient time in the office by means of improved efficiency; and reduced production of contaminated aerosols and air droplets.
 |
PRETREATMENT (COVID-RELATED SCREENINGS AND DIAGNOSES)
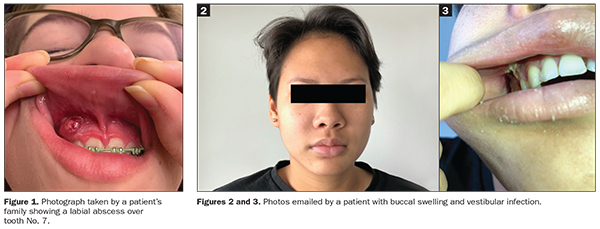
Added patient visits may increase the risk of transmission of the coronavirus and also use up precious, costly, and possibly limited PPE resources. In turn, you should attempt to remotely and virtually “tele-screen” and triage patients when they contact your office with a toothache. For instance, try to rule out non-endo-related symptoms, such as dentin hypersensitivity (ie, momentary sharp pain to sweets or brushing) or parafunction (ie, non-localized pressure tenderness waking patients up at night or present upon waking up in the mornings). Encourage patients to send you intraoral and extraoral photos taken on their smartphones1,2 (Figures 1 to 3).
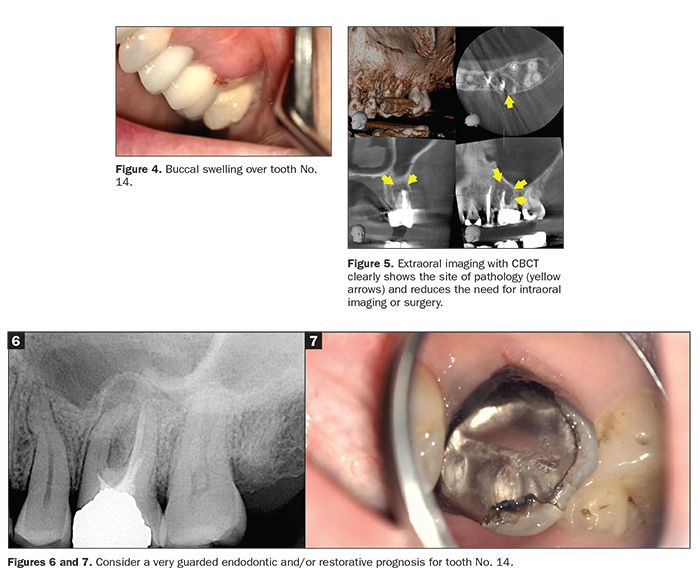
Whenever possible, incorporate more extraoral imaging, such as CBCT scans or panorex x-rays, for diagnosis. This helps reduce the need for intraoral radiographs, which entail an increased risk of patients coughing or gagging, which may produce contaminated droplets.3 A CBCT scan can often replace the need for an invasive exploratory endodontic access and/or a surgery that would inherently involve contact with contaminated saliva and/or blood (Figures 4 and 5).
 |
TREATMENT PLANNING
In order to reduce the number of patient visits, be prepared to treat a patient who may have presented for a consultation only. This preparation should start prior to the appointment. Administrative staff should educate patients as to why limiting excursions out of their “safe” homes and accepting same-day treatment, if determined to be necessary, benefits their safety during a pandemic. Hence, if it’s determined that a patient requires emergency or non-emergency treatment, your staff and you should be prepared to provide immediate treatment. This includes front desk staff rearranging the schedule to accommodate the unscheduled treatment and even calling and moving the following scheduled patients a “few minutes” later, as you might be running late with the unscheduled emergency. It also includes having logistical clinical systems in place that enable immediate treatment. Such a reduction of patient visits would benefit the patients’ and staff’s safety and the practice’s efficiency and production—a win-win during a pandemic.
When treatment planning, keep in mind the importance of definitive treatments. When presenting patients with treatment options, explain that during a pandemic, it might not be the time for heroic endodontics. Treatments with a lower prognosis are more likely to require follow-up visits due to postoperative complications or failures. For instance, the retreatment of a complex molar case that has guarded restorability may have a poor prognosis vs that of an extraction and implant replacement (Figures 6 and 7).
 |
TREATMENT CONSIDERATIONS
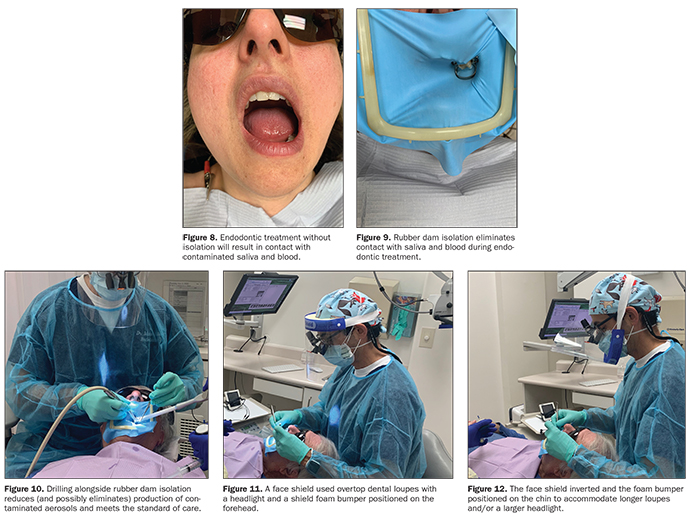
Once it is determined that endodontic treatment is necessary, you should keep the following in mind: Reduce the airborne spread of the virus by decreasing, and possibly eliminating, the production of contaminated aerosols and droplets by using rubber dam isolation.3,4
It should be noted that rubber dam isolation is an unequivocal standard of care in North America and must be incorporated during all non-surgical root canal treatments. A COVID-related benefit of its use is the elimination of contact with contaminated saliva during drilling and file handling and the prevention of air droplets, should patients cough during the procedure (Figures 8 to 10). So, not only do we have to use rubber dam isolation, but it could be argued that it may make non-surgical endodontic treatment one of the least likely procedures to produce contaminated aerosols and air droplets. Prior to endodontic access preparation, oral rinse with an antiviral solution is encouraged, along with bathing the isolated tooth’s crown with an antiviral solution.3
Reduce the patient’s time in the chair by performing the procedure as efficiently as possible with the following protocols and armamentaria.
Use enhanced magnification and illumination to more efficiently locate canals, including calcified and MB2 canals. This is accomplished by using high-power loupes with an overhead light and/or a dental microscope. Depending on the guidelines in your jurisdiction, face shields may be necessary. Note that the use of a face shield with a microscope could be a minor challenge, so the practitioner will have to get creative. You also might need some ingenuity to incorporate shields into your practice: for example, having the shield come up from the chin instead of down from the forehead (Figures 11 and 12).
 |
Using a quality electronic apex locator to determine working lengths will reduce the need for numerous intraoral radiographs, which expose your assistant and you to contaminated saliva and the risk of the patient coughing while taking the radiographs, and make the procedure more efficient overall.
Endodontic NiTi filing systems that require fewer files and fewer steps than traditional NiTi filing systems will help make the procedure more efficient and enable you to possibly accommodate endodontic emergencies and same-day treatments.
Traditionally, multi-visit root canal treatments have been common for teeth with necrotic pulps. Yet, as previously mentioned and whenever possible, performing root canal treatments in a single visit is encouraged. This is possible by performing root canals more efficiently and by incorporating certain protocols. Studies show no difference in outcomes between single- and multi-visit root canal treatments when certain protocols are incorporated. In part, they include enhanced intra-canal medication and activation. It has also been shown that there may be no increased risk of post-op pain with single-visit root canal treatments vs multi-visit treatments. The same was the case for the risk of post-op flare-ups following single-visit root canal treatments, hopefully meaning no increased need for post-op visits.5,6
If the opportunity is there, one might also attempt to permanently restore the endodontically treated tooth in the same visit, especially while rubber dam isolation is still present and immediately after root canal treatment. Doing so helps improve the outcome by reducing coronal bacterial microleakage and should help reduce the risk of tooth and/or temporary restoration fractures, especially if a follow-up visit is not imminent.7
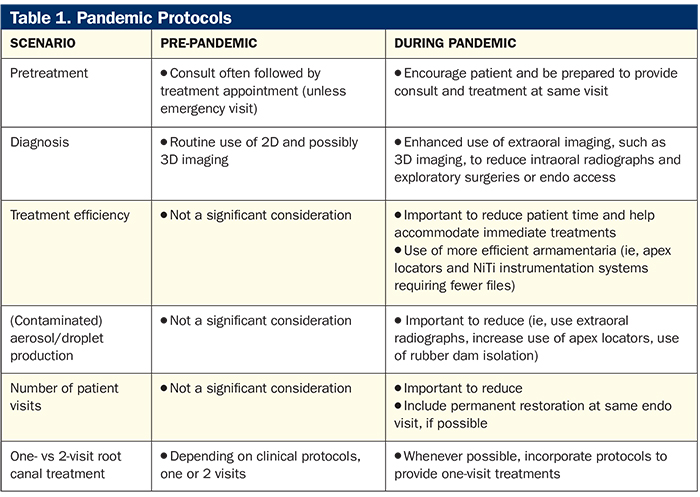
This is all very important to keep in mind while providing treatment during a pandemic as patients need to reduce their excursions outside their homes. Table 1 sums up the considerations and protocols that help us adapt to practicing endodontics during the COVID-19 pandemic.
IN SUMMARY
Providing endodontic care during a pandemic should entail protocols that reduce the risk of viral transmission amongst patients, staff, and doctors. This means reducing unnecessary patient visits by means of teledentistry, being prepared to provide same-day treatment, reducing treatment times, and reducing the production of contaminated aerosols and air droplets. Doing so benefits and safeguards patients, dental staff, and the viability of your dental practice.
References
- Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19). Guidance for dental settings. Updated August 28, 2020. Accessed November 12, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html.
- American Dental Association. ADA coronavirus (COVID-19) center for dentists. Updated November 6, 2020. Accessed November 12, 2020. https://success.ada.org/en/practice-management/patients/infectious-diseases-2019-novel-coronavirus.
- Harrel SK, Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. J Am Dent Assoc. 2004;135:429-437.
- Baumann K, Boyce M, Catapano-Martinez D. Transmission precautions for dental aerosols. Decisions in Dentistry. December 12, 2018. Accessed November 12, 2020. https://decisionsindentistry.com/article/transmission-precautions-for-dental-aerosols/.
- Schwendicke F, Göstemeyer G. Single-visit or multiple-visit root canal treatment: systematic review, meta-analysis and trial sequential analysis. BMJ Open. 2017;7:e013115.
- Kalhoro FA, Mirza AJ. A study of flare-ups following single-visit root canal treatment in endodontic patients. J Coll Physicians Surg Pak. 2009;19:410-412.
- Goldfein J, Speirs C, Finkelman M, et al. Rubber dam use during post placement influences the success of root canal-treated teeth. J Endod. 2013;39:1481-1484.
Dr. Haas is a certified specialist in endodontics and lectures internationally. He is a Fellow of the Royal College of Dentists of Canada and is on staff at the University of Toronto Faculty of Dentistry and the Hospital for Sick Children. He maintains a full-time private practice limited to endodontics and microsurgery in Toronto. He can be reached at haasendoeducation.com.
Disclosure: Dr. Haas reports no disclosures.
Related Articles
Better and Faster Root Canal Treatments: A Synopsis of the Latest High-Tech Protocols
Root Canals Aren’t What They Used to Be
Questions to Ask Prior to Root Canal Treatment











