Successful outcomes in oral health often depend on how well the rest of the body is doing—and vice versa. So, many dental practices and other healthcare providers are taking an integrated approach to treatment, working with each other to improve the lives of their patients.
It’s a new perspective, though, and many dentists and doctors alike simply aren’t familiar with it. To help, the Virginia Oral Health Coalition (VaOHC) has developed an online toolkit that providers can use to improve their collaboration and address their patients’ needs.
“Were hearing from a lot of providers that they’re really excited about the possibilities of integrating oral health into their practice. Or if they’re a dental provider, integrating a little more primary care,” said Sarah Bedard Holland, executive director of the VaOHC. “But they want some really practical information about how.”
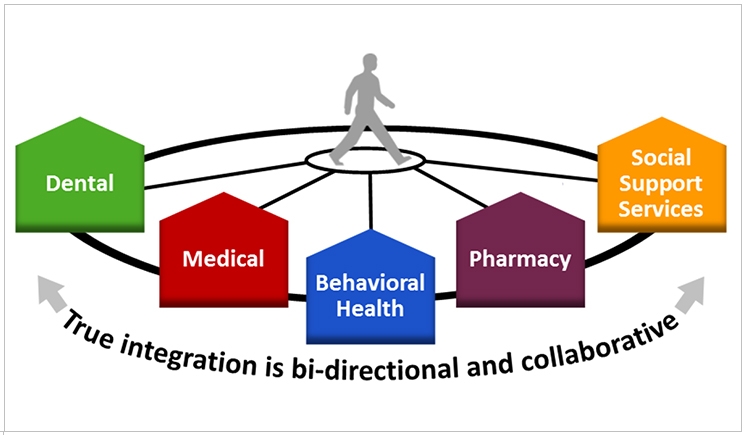
The toolkit spotlights advice for dental, medical, behavioral health, pharmaceutical, and social support professionals, detailing where their interests overlap. For instance, dentists can measure blood pressure during regular checkups, and pharmacists can monitor opioid use.
“We know that children see a pediatrician 8 times in their first year or 2 of life. That’s a fabulous opportunity for the pediatrician to begin applying a varnish to those early-erupting teeth and making sure that the caregivers understand the solid need for that child to see a dentist by the age of one,” said Bedard Holland.
“We also know the opportunity for primary-care providers to talk to adult patients about the relationship between diabetes and periodontal disease, or between oral health and heart disease,” said Bedard Holland. “The relationships and associations are pretty astounding.”
The toolkit is more than a series of questions and procedures for providers to ask and employ. It also outlines opportunities to address community health needs across the medical spectrum, starting with strategies for reducing emergency room usage related to dental issues that could have been addressed more appropriately elsewhere.
“One of the biggest challenges is that adults on Medicaid don’t have access to a comprehensive dental benefit. It’s an emergency extraction benefit that really doesn’t do anything to keep adults out of the emergency department for care,” said Bedard Holland. “It doesn’t provide any preventive services.”
For example, Bedard Holland said, 81% of adults who go to the emergency room for dental treatment get prescribed an opioid. Also, almost 70% of them are prescribed an antibiotic because the ER doesn’t provide access to dental treatment, so providers there can only help with the pain and the infection.
Additionally, better oral care can significantly impact ventilator-associated pneumonia in the intensive care unit as well as maternal and child health and wellness. Oral care concerns in patients with mental illness or chronic illnesses like heart disease are addressed too.
The toolkit takes on these issues at the office level and across the industry. It focuses on leadership, education, patient populations, available services, communication, measures and assessment, financing, infrastructure, and community support as well. All of these factors, the group believes, are necessary to improving access to integrated care.
“The Medicaid kids here in Virginia have access to really fabulous comprehensive dental benefits,” said Bedard Holland. “And while we do have about half of these kids accessing that benefit, which is a good number if you compare it to the national rate, that still means that half of these kids who are enrolled are not taking advantage of it for a variety of reasons.”
After considering the opportunities to address community health needs and answering the toolkit’s prompt queries about the core components of integration, clinical organizations can employ the Integration Model Checklist, which will help them assess where they now stand and identify areas for action.
“Let’s say the dental providers are practicing at a community health center,” said Bedard Holland. “They could look at some of the opportunities to address some of the community health needs that surround them and really think with their partners about some even more elevated ways to integrate.”
Additional practical resources in the toolkit include a series of clinical practice tools, such as a caries risk assessment form, an overview on dry mouth, a guide for integrating electronic medical records, fluoride varnish billing instructions, and other instructional documents. Resources for educating patients also are available.
“And we’re continually updating,” said Bedard Holland. “One of the reasons we wanted to do this online was so we could continually update the information that’s provided there. These kinds of things will be updated as we hear from other people about what information they need from the kit.”
Finally, the VaOHC acknowledges that there will be a curve as dentists and other practitioners begin to learn more about each others’ respective fields—not just in terms of presentation and treatment, but also in practice management. The toolkit links to a host of online continuing education opportunities as well.
“If dentists are interested in facilitating additional opportunities, I would suggest that they reach out to their state dental association and ask for some help,” said Bedard Holland. “There are a lot of groups out there that are really interested in providing additional training.”
Related Articles
Collaborative Dental Practice Targets Systemic Healthcare
Dental Hygienists Support Systemic Health Screenings
University Plans $15.5 Million Research Center for Oral-Systemic Health











