INTRODUCTION
Over the past 30 years, the approach to replacing a missing tooth or a couple of missing teeth has changed dramatically. Implant dentistry has almost become the standard of care for single- or multiple-tooth replacement due to the assumption that it is a less invasive and more durable approach than a fixed prosthesis. Traditional crown-supported fixed prostheses require aggressive tooth removal because they need taper and parallelism between both abutments. For many tooth-conserving clinicians and patients, the idea of cutting adjacent teeth for a fixed bridge is unimaginable considering the collateral damage and possible side effects. Most patients deem a fixed implant to be more desirable than a removable partial denture.
After 30 years of dental implants, astute dental professionals have learned that, in many cases, dental implants are neither more minimally invasive nor problem-free. In a large study of the Swedish population, it was found that at 9 years, 45% of all patients presented with peri-implantitis, bleeding on probing/suppuration, and bone loss greater than 0.5 mm, as well as a 7.6% implant loss during the same period.1,2
In some cases, the patient has to undergo invasive bone augmentation graft surgeries to place a dental implant. The procedure is far from minimally invasive or problem-free, especially when considering that 11.3% of implants placed on grafted sites fail during the first 5 years of function.3 Also worthy of note is that placing dental implants in young patients may result in long-term “aesthetic failure,” meaning successful integration but unaesthetic positioning due to the development of the alveolar process. When considering the many possible complications of implant tooth replacement and the advances in adhesion and dental materials, it may be time for astute professionals to consider minimally invasive bonded bridges as a first-choice option in certain clinical circumstances.
THE EVOLUTION OF MINIMALLY INVASIVE ANTERIOR BONDED BRIDGES
When thinking about bonded bridges, many clinicians think of the Maryland bridge,4 which is broadly viewed as unsuccessful. A common and very problematic complication with the metal 2-retainer design is the debonding of one retainer, often resulting in secondary caries. This complication can be caused by the lack of sufficient adhesion to the metal pad and the flexibility of thin metal abutment wings, which causes a peeling effect. Also, occlusal forces have consequences on anterior teeth, creating an uneven tooth deflection. All of the above problems combined lead to increased failure rates. Subsequently, Yamashita and Yamami5 introduced a new design in Japan, adding mechanical retentive features to the “adhesion bridge” and utilizing a metal adhesive. Figures 1 to 4 show a bonded bridge treated by Dr. Bertolotti, successfully using this concept on a cantilever bridge made more than 30 years ago and still in service.

Figure 1. Preoperative view of a very young patient with a congenitally missing lateral.

Figure 2. Occlusal view of the retainer wind design, showing the channel preparation on the mesial of the canine.
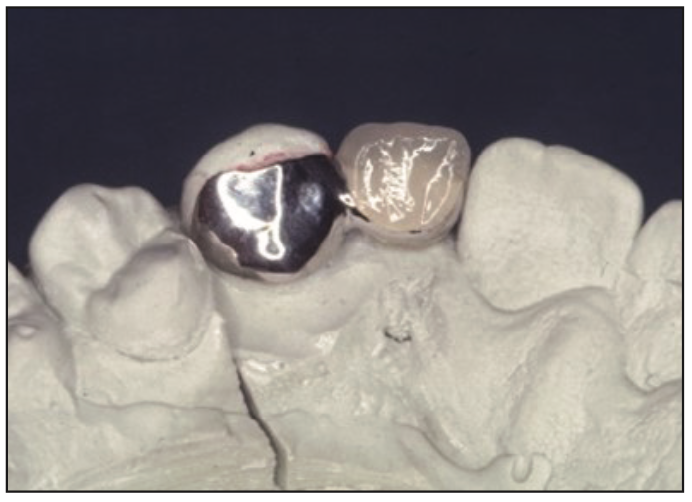
Figure 3. The cast with the nickel-chromium-based alloy, Rexillium III, for rigidity and a PFM pontic.
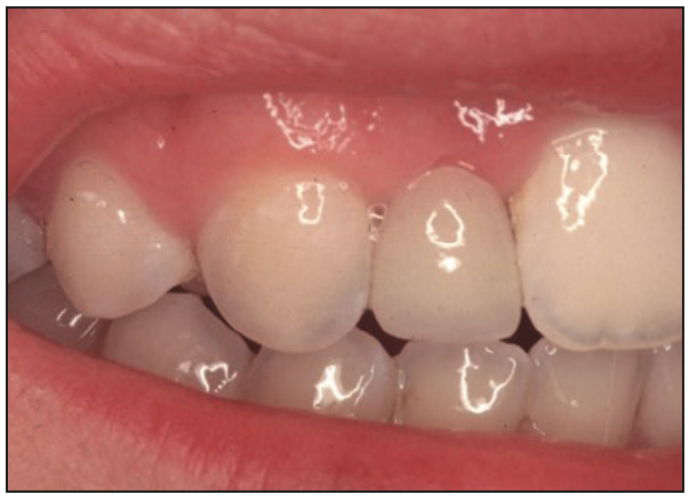
Figure 4. The bridge was bonded with Opaque shade PANAVIA 21 (Kuraray Noritake Dental).
THE CANTILEVER BONDED ZIRCONIA BRIDGE
In 1990, all-ceramic adhesion bridges began to be used. Realizing the disadvantages of the 2-retainer design for anterior teeth, Kern6 introduced the single-retainer (cantilever) design using all-ceramic materials with excellent success. Alumina bridges had high adhesive success but with higher fracture rates than desirable. Kern subsequently began using zirconia to replace the alumina and established successful methods for bonding to zirconia, a non-etchable ceramic. The survival rates reported were remarkably high: 99.2% at 10 years. Fracture of the zirconia was rare, but “debonds” did occur. Generally, the debonded bridges were successfully rebonded. The rare, fractured zirconia bridges were traced to poor design in the stressed connector areas, and subsequently, minimum design requirements were established for clinical success: a minimum connector height of 3 mm and connector thicknesses of 2 mm, minimum lingual pad thicknesses of 0.7 mm, and a minimum bonding area of 30 mm2 on the retainer. Figure 5 depicts an ideal preparation following the above guidelines.6 Using the single-retainer zirconia concept, a patient with a missing left lateral incisor received a zirconia bonded bridge with a single canine retainer (Figures 6 to 8).
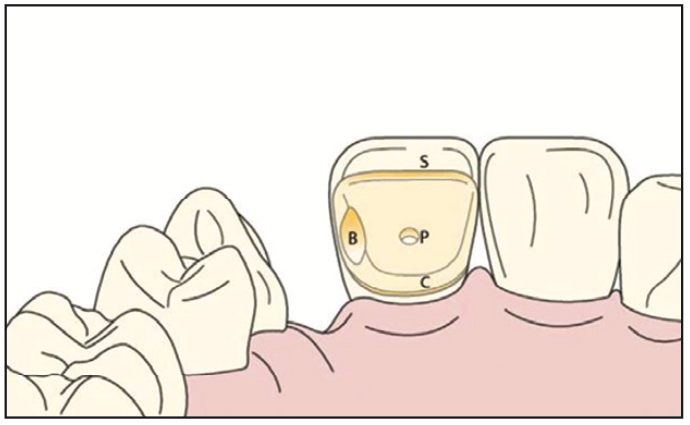
Figure 5. Kern-style lingual retained wing preparation. (Image courtesy of Dr. Mathias Kern and Quintessence Publishing.)

Figure 6. Patient with missing lateral. (Image courtesy of Dr. Charles Ruefenacht.)

Figure 7. Lingual view of a zirconia cantilever bridge. (Image courtesy of Dr. Ruefenacht.)

Figure 8. Facial view of the previous case. (Image courtesy of Dr. Ruefenacht.)
ALTERNATIVE DESIGNS FOR ANTERIOR BONDED BRIDGES
Understanding principles learned through the evolution of bonded bridges allows us to be more creative with different designs based on the variety of clinical circumstances our patients present. The 6 primary considerations for success are materials selection, sufficient dimension of connectors, sufficient stiffness on the bonded retainer pad, sufficient size of the bondable surface, proper bonding protocol, and proper management of occlusal forces. An example of a variation required by clinical circumstances would be when a patient is treatment-planned for porcelain veneers for aesthetic reasons and there is a missing tooth. An important variation on the retainer design frequently used by Dr. Ruiz is the porcelain veneer-supported bonded bridge with 2 retainer wings. When the bonded bridge is being placed where severe occlusal forces are expected, a 2-retainer option should be considered. Tagami et al7 showed that a 2-retainer option withstands higher debonding forces than a single retainer on posterior bonded zirconia bridges, with narrow- and wide-rest designs showing no statistical difference in retention. Other clinical circumstances possibly requiring 2 retainers could include canine and first premolar replacements, where anterior and posterior teeth are connected, especially on heavy grinders. Figures 9 to 11 depict a case using an anterior veneer to posterior onlay-proximal rest-retainer design.

Figure 9. Canine replacement using an anterior veneer to posterior proximal-facial rest-retainer design.
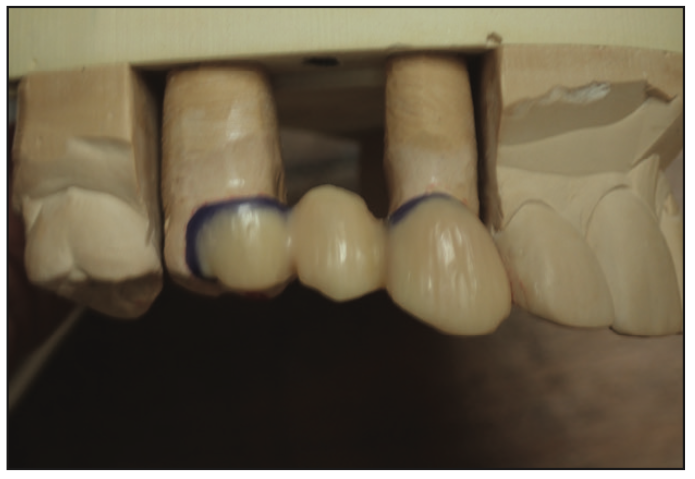
Figure 10. Wax design of a bonded bridge.

Figure 11. Immediately after bonded cementation.
POSTERIOR MINIMALLY INVASIVE BONDED BRIDGES
While the adhesive forces can retain properly designed cantilevered posterior bridges, Passia et al8 have shown short-term clinical durability with cantilever posterior bonded bridges. Long-term experience has shown that posterior teeth with cantilevers often cannot withstand occlusal forces successfully, especially in bruxers; those teeth frequently show signs of occlusal trauma and even fractures (Figures 12 and 13). A posterior 2-retainer design could be considered a safer option because the occlusal forces will be better supported, and with a preparation mostly on enamel, it can still be considered extremely minimally invasive. Design can vary dramatically depending on the condition of existing retainer teeth. One common scenario is the 2-inlay/onlay retainer design, especially when retainer teeth already have existing restorations. Figure 14 shows a molar rest-retainer extending facially for aesthetic purposes. The features in this preparation are sufficient bonding surface to exceed 30 mm2 minimum, a 1-mm proximal-occlusal reduction, and needing to maintain parallelism to the second retainer tooth. This preparation is primarily on enamel and margins and always supragingival. The posterior connector size should be 3 mm in height and 4 to 5 mm in width. Figures 15 and 16 show a posterior 2-retainer bonded bridge using the above design. While the profession has limited experience with minimally invasive posterior bonded bridges, they are a very desirable option because of their minimally invasive nature. The authors’ extensive experience in adhesive dentistry gives them the confidence to know that a properly designed and bonded adhesive bridge retainer will have equal or fewer chances of coming loose than a crown-retained counterpart with traditional crown and bridge cement. Attention to lateral forces and understanding the Three Golden Rules of Occlusion9 will yield more manageable forces to the fixed prosthesis.
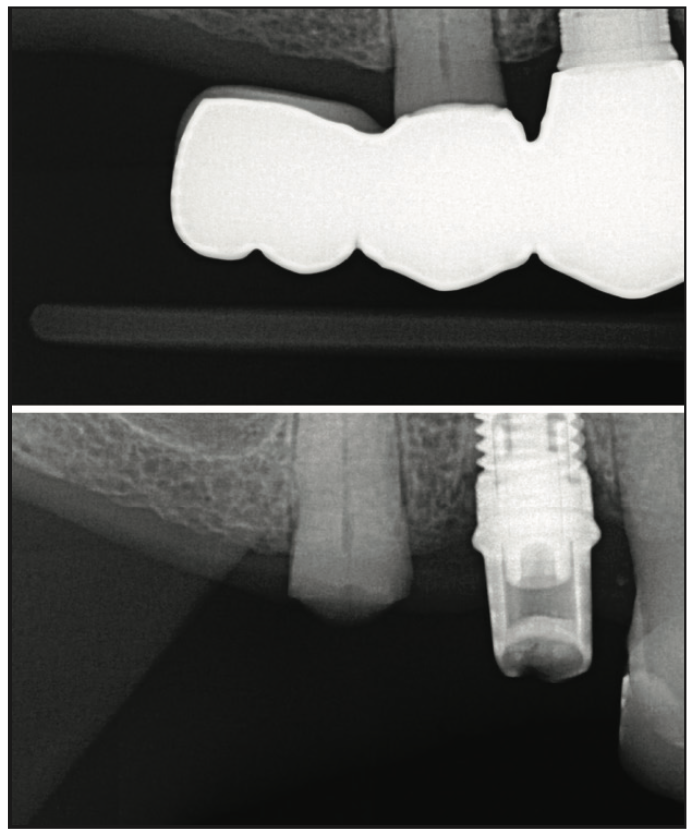
Figure 12. Before and after photos of a posterior cantilever bridge that caused the full fracture of a retainer tooth.
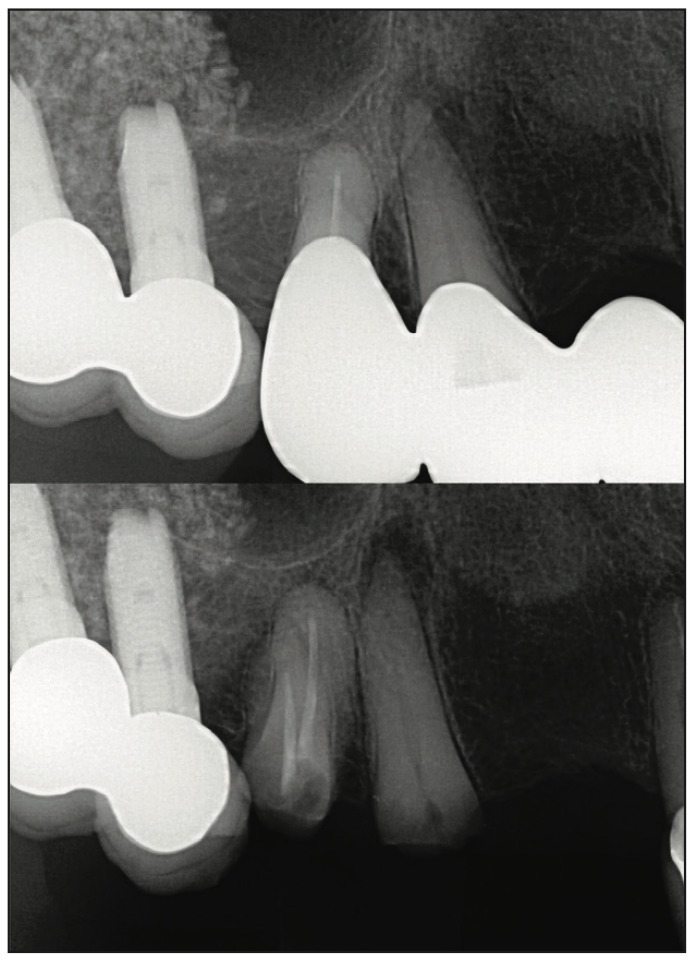
Figure 13. A second case with a similar clinical circumstance as the previous one.

Figure 14. A molar rest-retainer design.

Figure 15. Zirconia restoration in the cast.

Figure 16. Clinical view immediately after cementation.
ZIRCONIA AND BONDING TO ZIRCONIA
The assumption that all zirconia restorative materials are the same will lead to frustration and failure. Attention should be placed on choosing a properly manufactured, high-strength Y3 (3 mol% yttria) zirconia, like KATANA Zirconia LT, HT, or HTML Plus (Kuraray Noritake Dental). More translucent Y4 (4 mol% yttria) or higher zirconia formulations are weaker and are more likely to lead to fractures of the connector. The elastic modulus of zirconia is superior to precious metal, thus making it a better choice for stiff-bonded retainer pads. Kern et al10 have shown that 0.7 mm is the sufficient thickness for anterior retainer pads. Posterior rest/pads should be 1 mm. Bonding to zirconia has been tested by long-term studies, allowing clinicians to understand that zirconia adhesion can be very strong and durable.10 There are multiple ways to successfully bond to zirconia. Blatz et al11 have suggested the APC Concept: A stands for air abrading with aluminum oxide particles; P stands for priming with MDP-based primer (CLEARFIL CERAMIC PRIMER [Kuraray Noritake Dental]); and C stands for cement, using a self-cure or dual-cure resin cement, like Panavia V5. Alternately, Dr. Bertolotti has advocated for more than a decade for a simple and proven method to bond to zirconia: alumina sand blast and air remove the powder, (do not rinse with water, as it slightly decreases adhesion), followed immediately by the application of Panavia F 2.0 or 21 (Kuraray Noritake Dental) (both MDP-containing resin cements do not require primer) and seating on phosphoric-etched enamel.
CONCLUSION
After almost 40 years of experience with osseointegrated implants for tooth replacement, it is evident that they are not trouble-free nor minimally invasive in many cases. After more than 30 years of trial and experience, adhesion bridges have evolved. They are highly successful treatment options for anterior teeth and, in many cases, should be considered a first-choice treatment over more invasive implant procedures. Their use for posterior missing teeth is now being established with some very promising early results. As always, the clinician is responsible for making a proper case selection, discussing the pros and cons of each procedure, and allowing the patient to make an appropriate, informed decision. Most bridges are currently being made of Y3 zirconia and minimally invasive tooth preparations in enamel.
REFERENCES
1. Derks J, Schaller D, Håkansson J, et al. Effectiveness of implant therapy analyzed in a Swedish population: prevalence of peri-implantitis. J Dent Res. 2016;95(1):43–9. doi:10.1177/0022034515608832
2. Derks J, Håkansson J, Wennström JL, et al. Effectiveness of implant therapy analyzed in a Swedish population: early and late implant loss. J Dent Res. 2015;94(3 Suppl):44S-51S. doi:10.1177/0022034514563077
3. Eckert SE, Salinas TJ, Akça K. Chapter 6: Implant fractures: etiology, prevention, and treatment. In: Froum SJ, ed. Dental Implant Complications: Etiology, Prevention, and Treatment. 2nd ed. Wiley-Blackwell; 2015: 132–44.
4. Thompson VP, Del Castillo E, Livaditis GJ. Resin-bonded retainers. Part I: Resin bond to electrolytically etched nonprecious alloys. J Prosthet Dent. 1983;50(6):771–9. doi:10.1016/0022-3913(83)90088-4
5. Yamashita A, Yamami T. Design and clinical procedures of adhesion bridge (adhesion splint). J Jap Pros Soc. 1982; 26:592–8.
6. Kern M. Resin-Bonded Fixed Dental Prostheses: Minimally invasive – esthetic – reliable. 1st ed. Quintessence Publishing; 2018.
7. Tagami A, Chaar MS, Zhang W, et al. Retention durability of one-retainer versus two-retainer posterior RBFDPs after chewing simulation. J Mech Behav Biomed Mater. 2022;133:105353. doi:10.1016/j.jmbbm.2022.105353
8. Passia N, Chaar MS, Kern M. Clinical outcome of posterior cantilever resin-bonded fixed dental prostheses using two different luting agents. J Prosthodont Res. 2022. doi:10.2186/jpr.JPR_D_22_00033
9. Ruiz JL. The three golden rules of occlusion. Dent Today. 2010;29(10):92–3.
10. Kern M, Passia N, Sasse M, et al. Ten-year outcome of zirconia ceramic cantilever resin-bonded fixed dental prostheses and the influence of the reasons for missing incisors. J Dent. 2017;65:51–5. doi:10.1016/j.jdent.2017.07.003
11. Blatz MB, Alvarez M, Sawyer K, et al. How to bond zirconia: The APC concept. Compend Contin Educ Dent. 2016;37(9):611–7.
ABOUT THE AUTHORS
Dr. Ruiz is founder of the Los Angeles Institute of Clinical Dentistry, former course director of the University of Southern California’s Esthetic Dentistry Continuum, associate instructor at Gordon J. Christensen Practical Clinical Courses in Utah, and an independent evaluator for Clinicians Report. He is the author of Supra-Gingival Minimally Invasive Dentistry with Dr. Ray Bertolotti and of many research and clinical articles. He has been named as one of Dentistry Today’s Leaders in CE since 2006. He is also in private practice in the Studio District of Los Angeles. He can be reached at drruiz@drruiz.com.
Disclosure: Dr. Ruiz reports no disclosures.
Dr. Bertolotti received his DDS degree from the University of California, San Francisco, after working as a PhD metallurgical and ceramic engineer at Sandia National Laboratories. He is perhaps best known for introducing “total etch” to North America in 1984. He also introduced Panavia in 1985, tin plating in 1989, self-etching primers in 1992, and HealOzone in 2004. He is the founder of Danville Materials (now part of Zest Dental Solutions) and was director of research at the company. The sectional Contact Matrix System, MicroPrime B, MicroEtcher sandblasting, and intraoral tin plating are also his developments. He is a well-known international lecturer, having presented at invited lectures in more than 30 countries. He can be reached via email at rbertolott@aol.com.
Disclosure: Dr. Bertolotti reports no disclosures.











