INTRODUCTION
An amalgam tattoo oral mucosal lesion is a relatively common finding. The diagnosis is often relatively simple. However, the differential diagnosis is extensive, and failure to elucidate the correct diagnosis can be a serious issue. The differential diagnosis of macular pigmented oral mucosal lesions includes the following: amalgam tattoos, hemangioma, oral melanotic macules, melanocytic nevi, melanoacanthoma, smokers’ melanosis, racial/physiologic pigmentations, post-inflammatory pigmentations, medication-induced pigmentations, varices, heavy metal deposits, systemic disease/condition-related pigmentations (Peutz-Jeghers syndrome [PJS], Addison’s disease), and malignant melanoma.1-9
Tavares et al9 reported a study of 34,127 archived histopathologic specimens. They noted that 458 were pigmented lesions, of which 230 were melanocytic. Approximately 60% were macular. Regarding the 458 pigmented lesions, amalgam tattoos were noted as the diagnosis of 46.3% of the specimens, melanotic macules represented 22.9%, and nevi represented 20.5%. Other diagnoses included racial pigmentation, exogenous pigmentation, and melanoma. Hassona et al5 reported a study of 386 patients with oral pigmentations. They noted that racial pigmentation represented 39.9% of the cases, smokers’ melanosis represented 32.9%, amalgam tattoos represented 18.9%, melanotic macules represented 5.7%, post-inflammatory pigmentation represented 1.6%, medication-related or systemic disease-related pigmentations represented 0.52%, heavy metal deposits represented 0.26%, and oral nevi represented 0.26%. Kauzman et al2 listed other differential diagnoses, including Addison’s disease, Kaposi’s sarcoma, hemangioma, varices, PJS, LHS, thrombi, hematoma, blue nevi, and melanoacanthoma.
The diagnosis of an amalgam tattoo is based upon several factors, which include a history of prior dental restorative and surgical therapies, the length of time the lesion has been present, the clinical appearance of the lesion, the determinative differential diagnosis of other oral pigmented lesions, and radiographic and histopathologic findings.1-5
We present a case of an oral mucosal amalgam tattoo and also review the differential diagnoses of other oral mucosal macular pigmented lesions.
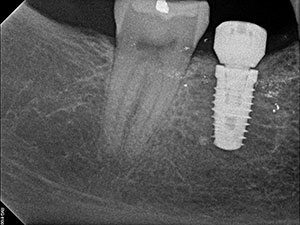
 |
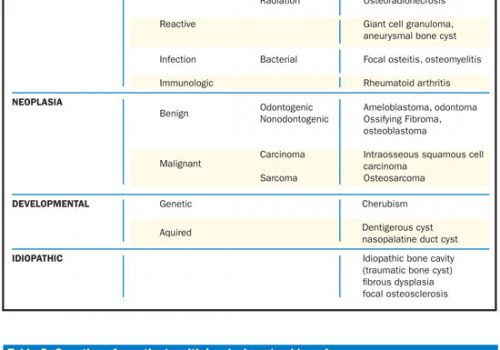
| Figure 1. Appearance of the darkened gingiva inferior to the implant replacing the right mandibular first molar. |
 |
 |
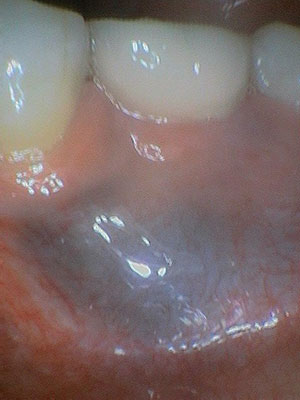
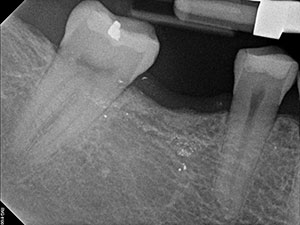
| Figure 2. Periapical radiograph taken prior to placing the implant. | Figure 3. Periapical radiograph taken after placement of the implant. |
 |
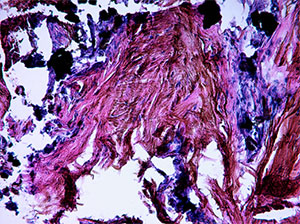 |
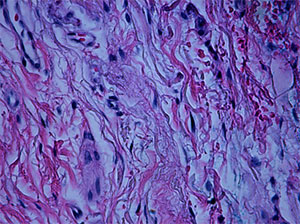
| Figure 4. Histopathology of a biopsy specimen at 100x. | Figure 5. Histopathology of the biopsy specimen at 200x. |
AMALGAM TATTOO CASE REPORT
A 47-year-old female patient presented to her periodontist for a periodontal evaluation in late January 2019 with the following chief complaint: “I bit down on an olive pit and felt some discomfort for about a day, and when I looked in my mouth, I noted a bruise.” The blackish gingival lesion buccal to the right mandibular first molar that was approximately 2 cm in diameter palpated as normal gingival tissue and appeared to be consistent with the appearance of an amalgam tattoo (Figure 1). However, the lesion was not present prior to implant surgery 3 years ago or at the postoperative appointments. The patient reported that the lesion was asymptomatic.
The working diagnosis was of an amalgam tattoo, and the initial differential diagnosis was that of an amalgam tattoo, a melanotic macule, hemangioma, and malignant melanoma. The patient’s radiographs from 5 years ago and 3 years ago, after the implant was placed, demonstrated opacities consistent with amalgam restoration fragments (Figures 2 and 3). Numerous opacities at the edentulous site of the right mandibular first molar were consistent with foreign dental material, the most common being amalgam. The occlusal surfaces of both the right mandibular second bicuspid and second molar had a flattened appearance. Also, the mesial lamina dura of the right mandibular second molar appeared to be thickened. The clinical appearance at the time was not consistent with amalgam tattoos.
The patient was seen toward the end of February 2019 for followup, and the lesion was perceived to be slightly larger and darker. A periodontal probe was utilized to apply pressure to the lesion, and the lesion failed to blanch. Therefore, the diagnosis of hemangioma was ruled out. A scalpel biopsy procedure was performed with one cartridge of 2% lidocaine with 1:100,000 epinephrine. The specimen was sent out for a histopathologic evaluation. The histopathology evaluation (Figures 4 and 5) reported a diagnosis of an amalgam tattoo. The connective tissue was noted for containing the incorporation of both faint (100x) amalgam particles and more prominent (200x) amalgam particles within collagen fibrils. The patient was informed of the benign diagnosis and educated regarding the condition.
DIFFERENTIAL DIAGNOSES OF ORAL MUCOSAL MACULAR PIGMENTATION MELANOACANTHOMA
Melanoacanthoma is an uncommon, benign, hyper-pigmented lesion. The clinical presentation is well-circumscribed, typically macular, dark-brown-to-black lesions. It preferentially occurs in young African American females and is relatively uncommon in white subjects. There is an association with continuing trauma. Approximately 20% of patients with melanoacanthoma present with multiple lesions. The histopathologic appearance is noted for the proliferation of dendritic melanocytes scattered through an acanthotic and hyperkeratotic epithelium. A biopsy is necessary for a definitive diagnosis.2,10
Melanotic Macule
A melanotic macule is a benign macular oral pigmented lesion and a relatively commonly occurring oral lesion. The condition is due to increased melanin production, and melanotic macule lesions can occur singly or in multiples, although most often singly. This lesion typically presents as a solitary macular with a well-defined, smooth border and homogeneously pigmented lesions and varying in size from 1 to 2 cm (although they can be smaller than 1 cm) and varying in color from tan to dark brown. The condition is more common in females than males, and the age range is from 1 to 98 years old. The lesions of such systemic conditions as PJS are multiple melanotic macules. The most common oral locations are the gingiva, palate, lower lip, and buccal mucosa. The histopathologic appearance demonstrates increased melanin pigmentation within the melanocytes and keratinocytes within the basal layer of the stratified squamous epithelium and sometimes within the upper portion of the lamina propria. A biopsy should be considered to rule out a diagnosis of melanoma, especially with regard to palatal lesions.2,8,11
 |
 |
| Figure 6. Multiple melanocytic macules of the lip in a Peutz-Jeghers syndrome (PJS) patient. | Figure 7. Multiple melanocytic macules of the buccal mucosa in a PJS patient. |
 |
 |
| Figure 8. Hemangioma of the buccal mucosa. | Figure 9. Blanching of the hemangioma due to pressure with a periodontal probe. |
Pigmented Oral Nevi
Oral pigmented nevi are rare macular benign lesions. Melanocytic nevi are a variable group of benign melanocytic neoplasms. They are characteristically brown or blue. Pigmented nevi are separated into several histologic categories: junctional, intradermal/intramucosal, and compound nevi. Congenital nevi present at birth, and banal nevi, also known as acquired melanocytic nevi, present in childhood and may continue to enlarge in adults over time. The most common lesion site is the hard palate, and these lesions are typically round to ovoid and sometimes macular. As the palate is known as a site of oral malignant melanoma lesions, it is necessary to biopsy pigmented lesions of the hard palate. The most common site for the intramucosal nevus is the buccal mucosa. Histologically, nevi are formed by an accumulation of nevus cells in the basal epithelium, lamina propria, or both. The transformation of oral pigmented nevi to melanoma is questionable.1-3,12,13
Post-Inflammatory Pigmentation
Chronic oral inflammatory mucosal disorders such as oral lichen planus can cause mucosal pigmentation. The condition is associated with darker complexions. The condition may present with multiple brown-to-black pigmented lesions of oral mucosal areas. The histopathologic picture notes increased melanin production by melanocytes and melanin-incorporated macrophages in the superficial lamina propria.2,3,14
Systemic Disease/Condition and Physiologic-Related Oral Mucosal Hyperpigmentation
The main characteristic of this group of conditions is bilateralism.
Physiologic (Racial) Oral Mucosal Pigmentation
Physiological pigmentation is associated with dark-skinned populations. The most common oral mucosal location is the attached gingiva. The condition is usually bilateral, with irregular, poorly defined borders.15
Smokers’ Melanosis
The condition of smoker’s melanosis presents as a black-brown oral mucosal pigmentation of the labial gingiva that is found in heavy smokers. The condition is more common in women compared to men.15
Medication-Induced Mucocutaneous Pigmentation
Drug-induced mucocutaneous pigmentation is associated with the long-term utilization of a number of systemic medications, including tetracyclines, antimalarials, antifungals, anti-mycobacterial drugs, anti-retroviral drugs, chemotherapeutics, psychotropic drugs, and oral contraceptives.15
Peutz-Jeghers Syndrome
PJS is an autosomal dominant genetic condition. The oral findings are pigmented macules (melanotic macules) of the lips and buccal mucosa. Melanotic macules also occur on the skin. These findings are significant as PJS is associated with benign hamartomas (polyps) of the intestines. These polyps increase the PJS patient’s risk for gastrointestinal (GI) cancers as demonstrated in a 50-year-old female with PJS (Figures 6 and 7).2,15,16 The patient presented at a university dental clinic in 1992, and she reported having a diagnosis of PJS, which her physicians previously established. When a dental patient presents with multiple melanotic macules of the lips and/or buccal mucosa, it is important for dentists to pursue the possibility of a PJS diagnosis in order to alert the patient of the risk of GI cancer.2,15,16
Laugier-Hunziker Syndrome
In Laugier-Hunziker Syndrome (LHS), mucocutaneous pigmentary melanotic macules occur on the labial, oral, and acral areas. Longitudinal melanonychia occurs in half of the patients diagnosed. Dermoscopic findings include regular reticular, linear, curvilinear arc streaks or parallel ridge patterns in mucocutaneous pigmentary lesions occurring most commonly on the lower lip, tongue, gingiva, or palatal mucosa, and they are brown, blue-black, or black in color. The average age of reported cases is 47.4 years old, and women are affected more than men. The occurrence of these lesions on the gingiva are similar to amalgam tattoos. LHS has a similar oral presentation to PJS but is a benign condition. Therefore, it is important to distinguish LHS from PJS. Besides oral lesions, cutaneous and/or genital melanosis may be present.2,5,15
Addison’s Disease
Addison’s disease is an autoimmune endocrine condition characterized by adrenocortical insufficiency. Hyperpigmentation may present on the skin, lips, oral cavity, conjunctiva, and/or genitalia. The treatment includes corticosteroid systemic drug therapy. If untreated, this condition is fatal.15
Heavy Metal Oral Discoloration
Increased levels of heavy metals such as lead, bismuth, mercury, silver, arsenic, and gold in the blood represent a known cause of oral mucosal discoloration. In adults, the most common cause for these increased levels is occupational exposure to heavy metal vapors. It is important to assess changes in the color of the oral mucosa and as a marker of disease with a thorough evaluation.3,9 Infrared spectroscopy can be used to evaluate the metallic deposits from melanocytic lesions. Intraoral biopsies and subsequent histopathologic examinations still represent the diagnostic gold standard. FTIR spectroscopy is another very useful diagnostic tool to differentiate amalgam tattoos from melanocytic lesions.4,15
OTHER PIGMENTED ORAL CONDITIONS
Varices
Varices (also known as varicosities) are distended veins. Oral varices may be observed in some patients at the ventral base of the tongue, and they appear dark blue. The cause of the distention is believed to be related to smoking, age, and hypertension.2,17,18
Hemangioma
Hemangioma, a relatively common benign proliferation of endothelial cells that line vascular channels, is another lesion to consider differentially. The lesion is flat or slightly raised, varying in color from red to bluish-purple, depending on the vessels involved.2 It can occur anywhere on the body and commonly appears on the face and lips. Two primary forms of hemangioma are infantile and congenital. Congenital hemangiomas appear at birth, and the infantile ones appear 1 or 2 months after birth and grow in size for a short time. They may either remain stable in appearance or regress. The treatment of macular hemangiomas is usually unnecessary, unless the lesion presents a cosmetic complaint. Sclerotherapy with ethanolamine oleate was utilized in years past. Presently, however, the laser is the surgical instrument of choice. Diagnosis can usually be accomplished by demonstrating the vascularity of the lesion through utilizing pressure to show blanching of the lesion when the pressure is applied. Diascopy, or placing a glass pathology slide over the lesion and applying pressure, has been the accepted standard.19,20
To illustrate the diagnosis of an oral mucosal hemangioma, a case is presented here. In early October 2020, a 70-year-old male patient, referred by his dentist, presented with a chief complaint of a sub-dermal lump in his left inner cheek (Figure 8). The lump was asymptomatic. Approximately 5 weeks prior, the patient discovered the lump as he could feel it with his tongue. The condition was described as a 1.5-cm, bluish-colored, round, slightly papular lesion of the left buccal mucosa. The lesion blanched when compressed by a periodontal probe, which determined a diagnosis of hemangioma (Figure 9).
Melanoma
Oral cancer only accounts for approximately 3.5% of cancers. Oral melanoma, or malignant melanoma of the oral cavity, is a very rare lesion, occurring in less than 1% of all oral malignancies. Malignant melanoma of the oral mucosa may be considered one of the most lethal of all human neoplasms. The most common oral location is the hard palate. This site represents approximately 40% of oral melanoma lesions. The main secondary site is the gingiva. Oral melanomas present as asymptomatic, slow-growing, brown-to-black lesions with irregular borders or as fast-growing lesions that may be associated with pain, ulceration, tooth mobility, bone destruction, and bleeding. The histopathologic picture is noted for the proliferation of malignant melanocytes adjacent to the basement membrane and within the lamina propria. Early diagnosis is essential with respect to treatment outcomes. The treatment is aggressive surgery with wide, clear margins. Nevertheless, oral melanoma has a poor prognosis.2,3,9,13,21
DISCUSSION
The amalgam tattoo oral mucosal lesion is a benign, asymptomatic condition. This condition can be safely diagnosed with dental radiographs to confirm the presence of radiopaque amalgam particles within the area of pigmentation. The pigmentation is typically blue to gray to black. The size is typically between 0.1 cm and 2 cm, and the lesions are not well-circumscribed.7,22
However, in some cases in which the patient or the clinician believes that the size of the lesion is increasing, it may be necessary to biopsy the lesion in order to provide a definitive diagnosis. The amalgam tattoo case presented was somewhat confusing. The patient or dentist did not notice the discoloration until years after the mandibular first molar had been removed and replaced with an implant. There was a perception by the dentist and the patient that the pigmented lesion had continued to enlarge.
The history and the radiographic appearance were consistent to determine a diagnosis of an amalgam tattoo. As the dental radiographs revealed radiopaque fragments within the area of the discoloration, an amalgam tattoo was the logical diagnosis. However, the possibility that the pigmented lesion was slow-growing necessitated a biopsy procedure to definitively determine the diagnosis and specifically to rule out oral malignant melanoma. Amalgam tattoos do not tend to grow in size.3,4,7,22
Another rationale for considering a biopsy procedure is the number of differential diagnoses related to oral mucosal pigmented lesions. In 2004, Buchner et al12 reported on an evaluation of 773 solitary pigmented melanocytic lesion cases from cases submitted from the files of the oral and maxillofacial pathology laboratory of the University of the Pacific School of Dentistry from 1984 through 2002. They reported the frequency of the various diagnoses of these lesions. They came to the following conclusions:
• Solitary pigmented melanocytic lesions are uncommon in the oral cavity and accounted for only 0.9% of the total biopsies accessed, while amalgam tattoos comprised 1.8%.
• Oral and labial melanotic macules were the most common solitary pigmented melanocytic lesions (86.1%), followed by oral melanocytic nevi (11.8%), oral melanoacanthoma (0.9%), and oral melanoma and atypical melanocytic proliferations (0.6% each).
Amalgam has been recognized as the primary posterior tooth restorative material for a great many years. Although there has been a decrease in the utilization of amalgam in the recent past, amalgam is still recognized as having advantages over other dental restorative materials. It is less sensitive to moisture during placement, it is very durable, it requires less expertise to place, and it is less expensive compared to other restorative dental materials. The use of amalgam has been attacked by the misconception that it is more toxic when compared to other dental materials. The issue of the amalgam tattoo is a relatively minor concern but a concern, nevertheless. Upon removing teeth with amalgam restorations, amalgam fragments may be incorporated within the stroma and may cause stable discoloration in the gingiva and other adjacent oral mucosal tissues. There are a large number of oral mucosal differential diagnoses, and the vast majority of them are benign lesions. The amalgam tattoo is localized, and there is no associated malignant transformation. The amalgam tattoo lesion is a relatively common condition, and the diagnosis is usually relatively straightforward. However, the diagnostic procedure of biopsy comes into play when the presentation or history is atypical. Fortunately, with respect to the case presented, the biopsy confirmed a diagnosis of an amalgam tattoo.3-5,22
CONCLUSION
In summary, amalgam tattoo lesions are relatively common benign oral lesions. With respect to the diagnostic process, there are a number of oral lesions with a similar appearance. It is important to define the diagnosis due to the seriousness of oral malignant melanoma, which may present similarly to many of these oral macular pigmented lesions.
References
- Natarajan E. Black and brown oro-facial mucocutaneous neoplasms. Head Neck Pathol. 2019;13:56-70.
- Kauzman A, Pavone M, Blanas N, et al. Pigmented lesions of the oral cavity: review, differential diagnosis, and case presentations. J Can Dent Assoc. 2004;70:682-683.
- Eisen D. Disorders of pigmentation in the oral cavity. Clin Dermatol. 2000;18:579-587.
- Laimer J, Henn R, Helten T, et al. Amalgam tattoo versus melanocytic neoplasm—differential diagnosis of dark pigmented oral mucosa lesions using infrared spectroscopy. PloS One. 2018;13:e0207026.
- Hassona Y, Sawair F, Al-Karadsheh O, et al. Prevalence and clinical features of pigmented lesions. Int J Dermatol. 2016;55:1005-1013.
- Lambertini M, Patrizi A, Fanti PA, et al. Oral melanoma and other pigmentations: when to biopsy? J Eur Acad Dermatol Venereol. 2018;32:209-214.
- Lundin K, Schmidt G, Bonde C. Amalgam tattoo mimicking mucosal melanoma: a diagnostic dilemma revisited. Case Rep Dent. 2013;2013:787294.
- Gondak RO, da Silva-Jorge R, Jorge J, et al. Oral pigmented lesions: clinicopathologic features and review of the literature. Med Oral Patol Oral Cir Bucal. 2012;17:e919-e924.
- Tavares TS, Meirelles DP, de Aguiar MCF, et al. Pigmented lesions of the oral mucosa: a cross-sectional study of 458 histopathological specimens. Oral Dis. 2018;24:1484-1491.
- Gonçalves IMF, Gomes DQC, Pereira JV, et al. Clinical and histopathological study of oral multifocal melanoacanthoma: a case report. J Clin Exp Dent. 2019;11:e391-e394.
- Rosebush MS, Briody AN, Cordell KG. Black and brown: non-neoplastic pigmentation of the oral mucosa. Head Neck Pathol. 2019;13:47-55.
- Buchner A, Merrell PW, Carpenter WM. Relative frequency of solitary melanocytic lesions of the oral mucosa. J Oral Pathol Med. 2004;33:550-557.
- Hicks MJ, Flaitz CM. Oral mucosal melanoma: epidemiology and pathobiology. Oral Oncol. 2000;36:152-169.
- Mergoni G, Ergun S, Vescovi P, et al. Oral postinflammatory pigmentation: an analysis of 7 cases. Med Oral Patol Oral Cir Bucal. 2011;16:e11-e14.
- Duan N, Zhang YH, Wang WM, et al. Mystery behind labial and oral melanotic macules: clinical, dermoscopic and pathological aspects of Laugier-Hunziker syndrome. World J Clin Cases. 2018;6:322-334.
- Mărginean CO, Meliţ LE, Patraulea F, et al. Early onset Peutz-Jeghers syndrome, the importance of appropriate diagnosis and follow-up: a case report. Medicine (Baltimore). 2019;98:e16381.
- Jassar P, Jaramillo M, Nunez D. Base of tongue varices associated with portal hypertension. Postgrad Med J. 2000;76:576-577.
- Hedström L, Albrektsson M, Bergh H. Is there a connection between sublingual varices and hypertension? BMC Oral Health. 2015;15:78.
- da Silva WB, Ribeiro ALR, de Menezes SAF, et al. Oral capillary hemangioma: a clinical protocol of diagnosis and treatment in adults. Oral Maxillofac Surg. 2014;18:431-437.
- Pal M, Saokar A, Gopalkrishna P, et al. Diode laser-assisted management of intraoral soft tissue overgrowth: a case series. Gen Dent. 2020;68:28-31.
- Gorsky M, Epstein JB. Melanoma arising from the mucosal surfaces of the head and neck. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:715-719.
- Galletta VC, Artico G, Dal Vechio AMC, et al. Extensive amalgam tattoo on the alveolar-gingival mucosa. An Bras Dermatol. 2011;86:1019-1021.
Dr. Cherry-Peppers is an associate professor at the Howard University College of Dentistry. She can be reached via email at gail.cherrypeppers@howard.edu.
Dr. Karapetian is in private practice in Vienna, Va.
Dr. Kumar is an assistant professor at the New York University School of Dentistry.
Dr. Morton is an associate professor at the Howard University College of Dentistry.
Dr. Edwards is a clinicial instructor at the Howard University College of Dentistry.
Dr. Brown is professor emeritus, Howard University College of Dentistry, and a clinical associate professor at Georgetown University Medical Center.
Disclosure: The authors report no disclosures.
Related Articles
Management of Oral Viral Lesions With a Diode Laser
Recognize the Patient and Lesion Risk Factors for Oral Cancer