|
INTRODUCTION
As preventive health care providers, what is our intention for prevention beyond the scope of providing hygiene therapy and giving oral hygiene instructions?
This article is not about the science of saving enamel or the dynamics of the dental caries process. It is intended to assist the everyday working hygienist in understanding the practical and predictable options for prevention. The intention is to help you become more knowledge about innovative and effective preventive products and the benefits that they provide.
THE MYSTERY IS IN THE HISTORY
Dental caries is an infectious disease. Streptococcus mutans and Lactobacillus produce organic acids when consuming carbohydrates, causing the pH to drop below 5.5. The acid dissolves the carbonated hydroxypatite, the main component of enamel, and demineralization begins. Thirty minutes later, the sugar is gone, and the mineral loss can be recovered (remineralization begins) from ions dissolved in the saliva. Dental caries result when the rate of demineralization exceeds the rate of remineralization and the latticework is destroyed.
Prevention of dental caries, especially in early childhood, is important with respect to its future progression, to improve the quality of life, and to reduce the costs of restorative treatments throughout a patient’s lifetime. Efficacious, safe, feasible, and cost-effective caries prevention methods for children are essential.
 |
 |
| Figure 2. Clinical flouride application (Profluorid L [VOCO America]) placement. | Figure 3. Application of fluoride using a tray for delivery. |
 |
 |
| Figure 4. Clinical application of a fluoride varnish (Flor-Opal Varnish [Ultradent Products]). | Figure 5. Zoom 2 Day White and Nite White with ACP (Discus Dental). |
MOVING BEYOND GOOD INTENTIONS
Everyday experience tells us that good intentions are often simply not enough. The use of traditional prophy pastes and fluoride foams and gels is no longer the only option we have.
Today our intention is to discuss different methods and products of prevention, such as fluoride varnish; amorphous calcium phosphate (ACP), a special milk-derived phosphopeptide that binds calcium and phosphate to tooth surfaces, plaque, and the surrounding soft tissues (Recaldent MI Paste [GC America]) (Figure 1); calcium sodium phosphosilicate (NovaMin [Sultan Healthcare]); and use of xylitol products into your practice.
TIMING MATTERS
The key to an effective preventive program is the appropriate mix at the appropriate time. In order to prevent primary caries, early intervention is important. To achieve lifelong caries prevention, fluorides, and other products must be made available during all stages of enamel development in both pre-eruption and posteruption. When ingested systemically through infant fluoride drops, fluoridated vitamins, and fluoridation, fluoride strengthens developing enamel. When applied topically via topical fluoride treatments, prescription fluorides, and toothpastes, fluoride not only strengthens posterupted enamel but also reverses incipient lesions and helps arrest the decay process.
 |
| Figure 6. Xylishield Comprehensive Dental Care System (Ultradent Products). |
CONCENTRATION MATTERS: PROFESSIONALLY APPLIED FLUORIDE COMPOUNDS
No longer does anyone question the efficacy of fluoride. In the United States, dental clinicians have been applying highly concentrated fluoride compounds directly to patients’ teeth for more than 50 years. Application procedures were developed based on the research that the fluoride would be incorporated into the crystalline structure of the enamel and would help develop a well-crystallized and more acid-resistant apatite in the enamel surface when the pH in the mouth drops (Figure 2).
Studies report that fluoride uptake by enamel increased in an acidic surrounding. Fluoride gel is often formulated to be highly acidic, consisting of a pH of 3.5 which can result in a bitter taste. The 3 professional strength fluoride products approved by the US Food and Drug Administration and ADA contain higher levels of concentration in both strength and acidity. Sodium fluoride (NaF) and stannous fluoride concentration both range between 9,000 ppm and 19,000 ppm, 9 mg and 19 mg of fluoride per mL. where as acidulated phosphate fluoride contains 12,300 ppm or 1.23 mg of fluoride per mL of product with a phosphoric acid pH of approximately 3.5. The at home self-applied NaF gels contain 5,000 ppm and stannous fluoride contains 1,000 ppm of fluoride per mL of product.
QUANTITY MATTERS: HOW MUCH IS TOO MUCH
The toxic nature of fluoride makes it necessary to establish prudent monitoring for professional strength fluoride treatments delivered within the dental office. Naturally, an area of concern includes professional strength topical fluoride treatments on children less than age 6 years, since this age group has the greatest incidence of inadvertently swallowing fluoride because of their immature swallowing reflex. The variables that directly affect fluoride ingestion by patients in the dental office include applying fluoride to the teeth with a cotton swab, dispensing the inappropriate quantity of fluoride, selecting the inaccurate size and shaped tray, or clinicians altering the fluoride tray (Figure 3) being used, thus making fluoride varnishes the fluoride of choice.
 |
EASE OF USE MATTERS
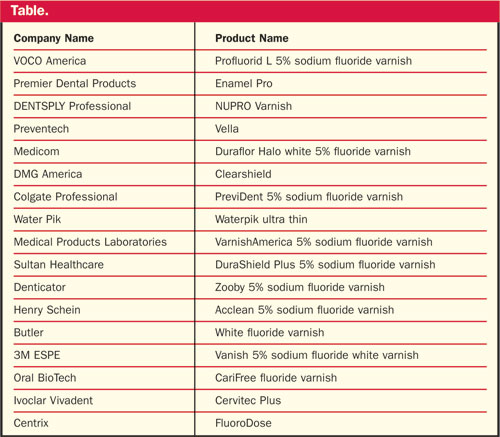
Fluoride varnish (Figure 4) has been used in the United States for caries (as “off-labeled”) since 1991 (Table). The primary reason for its wide acceptance is the easy, safe, convenient, and well-accepted application procedure, especially for young children. With fluoride varnishes, the amount of fluoride exposure to patients can be better controlled and less chair time is required. It covers the teeth with an adherent film for a prolonged period of time, thereby enhancing the uptake of fluoride ions into the tooth structure. Even though fluoride varnishes contain higher concentration levels of fluoride, 22,600 ppm of NaF, studies have shown lower levels of fluoride in blood plasma. Because the amount of fluoride ingestion is minimal, due to its adhesive nature, fluoride varnish can be applied to very young children.
The ADA Council on Scientific Affairs recently suggested the use of fluoride varnish as often as 4 times per year, for children and adults identified as high-risk.
KNOWLEDGE OF OTHER PRODUCTS AND BENEFITS MATTER
ACP—is inorganic amorphous calcium phosphate, made by combining soluble salts of calcium and phosphorous, and it consists of the same minerals contained in hydroxyapatite crystals. ACP speeds up remineralization by rapidly delivering calcium and phosphate ions to the tooth. ACP technology is found in Arm & Hammer Enamel Care with Liquid Calcium as well as their Age Defying Toothpaste, and Mentadent Replenishing White Toothpaste, Discus Dental’s Zoom 2 DayWhite and NiteWhite with ACP (Figure 5), Discus Dental’s Relief ACP sensitivity relief product, and Premier Dental Products’ Enamel Pro from and 5% NaF varnish.
Casein Phosphopeptide (CCP)-ACP—a 7.4-pH, milk-derived protein that releases bio-available calcium and phosphate ions when a patient’s saliva becomes acid challenged. When using CPP-ACP in the mouth, it binds to biofilm, plaque, bacteria, hydroxyapatite, and soft tissues. Elevating the level of fluoride further enhance its effects since fluoride requires a good source of calcium and phosphate for remineralization of enamel with the more acid-resistant fluorapatite. Recaldent CPP-ACP can be delivered to the teeth by Trident XtraCare gum with Recaldent, and MI Paste and MI Paste Plus manufactured by GC America.
Calcium Sodium Phosphosilicate compound (NovaMin)—is a tradename for bioactive glass. It is made from elements which are naturally found in the body. NovaMin particle delivers an ionic form of calcium, sodium, phosphorus, and silica, which bind to the tooth surface. When exposed to saliva or water, it instantly reacts, releasing sodium, calcium, and phosphate ions, which then interact and result in the formation of a crystalline hydroxycarbonate apatite layer that is chemically and structurally similar to enamel and bone. Products Containing NovaMin include: NUPRO Sensodyne Prophylaxis Paste, Sensodyne NUPRO Professional Toothpaste with NovaMin, Sensodyne Repair & Protect, NuCare Prophylaxis Paste with NovaMin and NuCare Root Conditioner with NovaMin, SootheRx, Dr. Collins Restore Toothpaste, and Burt’s Bees Natural Toothpaste.
Xylitol—is a naturally occurring sugar (alcohol) sweetener that is used as a sugar substitute. There is a considerable amount of evidence that the use of gum or candy with xylitol prevents dental caries in the permanent teeth when used several times daily. (The effectiveness varied between 30% and 60% when compared to controls without the gum use.) According to the NIH Consensus Statement on the Diagnosis and Management of Dental Caries, the evidence for xylitol is strong as the primary prevention of dental caries. The preventive effect of xylitol seems to derive from the remineralization of decalcified surfaces of teeth, replacement of fermentable dietary sugars and reduction of the amount of dental plaque or the amount of S mutans in plaque and saliva.
The most significant effect demonstrated so far in caries reduction is its ability to reduce the growth and acid production of S mutans, the primary bacteria responsible for caries. Growth retardation of S mutans is thought to result from an energy-spending “futile xylitol cycle” and impaired glucose uptake and metabolism
With regard to plaque, several studies have shown xylitol to reduce the amount, adhesiveness, and acidogenic potential of the bacterial colonies. Xylitol has the ability to reduce the number of S mutans in plaque and to loosen the plaque and bacteria binding to the tooth surface.
Caries prevention seeks to prevent the onset of carious lesions, arrest progression, and even to repair them. Prevention can be successfully carried out both by eliminating contributory factors of caries and by improving the resistance of teeth to caries attacks.
Dental products containing xylitol include Xylishield Comprehensive Dental Care System (Ultradent Products) (Figure 6), TheraGum and TheraMints (Godwin and Miller), BreathRx (Discus Dental), Spry (Xlear), Biotene, Dentiva (Nuvora), Natural Dentist (Caldwell Consumer Health), Supersmile Professional Whitening Gum, Trident Gum, and Spiffies.
THE POWER OF INTENTION
Studies have shown the beneficial effect of fluoride varnish in preventing progression of dental caries and the effect of using xylitol in reducing salivary S mutans levels. They have shown how the use of ACP, CCP-ACP, and NovaMin all help in the remineralization process These products may offer an efficacious and cost-effective caries prevention strategy, which may greatly improve the quality of oral health.
IN CLOSING: INTERVENTION FOR PREVENTION
By carefully evaluating techniques and using the appropriate materials, one can consistently obtain a predictable, practical, preventive program that works.
Ms. Hartley extensive professional experience spans 3 decades as a full-time practicing hygienist, patient care coordinator, business office administrator, and dental assistant. She is founder of a professional speaking and practice management consultant firm called The Business of Dental Hygiene that is dedicated to helping others develop productive hygiene departments where quality patient care and profitability are congruent, operating with systems and protocols that would not allow one to compromise the other. Ms. Hartley is the hygiene editor-in-chief for CPS Magazine. The CPS Evaluation Team members, combine product review for the whole team and consist of dentists, assistants, hygienists, front desk associates, and the dental laboratory. She can be reached via e-mail at hartleyrdh@aol.com or at the Web site deborahhartley.com.
Disclosure: Ms. Hartley reports no disclosures.











