A clear link between obesity and tooth loss has been confirmed in the largest study of its kind of over 200,000 adults which examined BMI, tooth retention, tooth location and age. The major new analysis of health insurance claims and health check-up data found that the higher the BMI, the greater the risk of tooth loss, especially in the over-40s.
The research group of Doctors Hiroshi Maegawa and Katsutaro Morino of Shiga University of Medical Science, Japan, collaborated with international oral healthcare company, Sunstar to analyze the relationship between BMI (Body Mass Index, calculated from body weight and height) and the numbers of teeth in each age group, and compared the positions of tooth loss between obese (BMI ≥25) and non-obese subjects using the large database of health insurance claims and health check-ups.
A higher BMI was associated with fewer residual teeth in the over-40s. Obese people lost more teeth, especially molars (i.e posterior teeth), compared to non-obese people. Smoking habits, in addition to obesity, increased the risk of tooth loss in positions different from those likely to be affected by obesity.
Obesity was also identified as a risk factor for tooth loss independent of sex, age, smoking, and diabetes. Although obesity had been known to be related to tooth loss, this data analysis enabled it to be assessed by the level of the BMI and residual teeth.
Just published by medical journal PLOS ONE (https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0274465),
results of the cross-sectional study suggest that weight loss and smoking cessation also become more essential to prevent tooth loss in people with obesity – in addition to early prevention of periodontal disease and dental caries, which directly cause tooth loss. To prevent periodontal diseases and caries from a young age, appropriate oral care should also be provided especially for back teeth, which are at a higher risk of loss.
Background and purpose of the research
Oral health is demonstrated to be associated with general health in various ways. Previous research by Shiga University of Medical Science in collaboration with Sunstar revealed that poor glycemic control decreases the number of teeth in people in their 30s and older. (Diabetology International, 2021 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8733090/).
Obesity is known as an important risk factor for various diseases including diabetes, hypertension, dyslipidemia, cardiovascular diseases, kidney diseases and cancer. According to the latest data from the World Health Organisation (WHO), 39% of adults aged 18 years and over were BMI ≥25 in 2016, and 13% were BMI ≥30. According to the 2019 National Health and Nutrition Survey in Japan, 33.0% of men and 22.3% of women were estimated to be obese with BMI ≥25. Although average BMI is much lower than Western countries, obesity has become a growing health problem in Japan.
Recent studies have demonstrated that obesity increased the risk of the onset and progression of periodontal diseases and that obese people are at higher risk of caries. Several studies have also already demonstrated that obesity is associated with the risk of tooth loss, but no large-scale study had previously been conducted to examine the impact of obesity on residual teeth by age and tooth position. The impact of obesity on tooth loss was also analyzed in view of other major risk factors, such as the indices of smoking and diabetes.
Research detail
The database of health insurance claims and health check-ups included a total of 706,150 subjects. A total of 233,517 adults were included in the study aged 20-74. This included 1) those who underwent a dental check-up in 2015, 2) those whose numbers and positions of teeth could be confirmed, and 3) those who had BMI and HbA1c levels from health check-ups and responses to questionnaires about smoking habits.
According to the classification of the degree of obesity by the Japan Society for the Study of Obesity, subjects were classified into four groups by BMI [underweight: <18.5, normal weight: 18.5-24.9, obesity (1 degree): 25.0-29.9, obesity (2-4 degrees); ≥30.0] to compare the numbers of teeth in 10-year age groups. The percentages of those having each tooth was divided into two groups by the presence or absence of obesity (defined as BMI ≥25) and into four groups by the presence or absence of smoking, in addition to obesity, were calculated. Logistic regression analysis was conducted using BMI, sex, age, smoking status, and diabetes (HbA1c ≥6.5%) as explanatory variables to calculate the odds ratio for having <24 teeth.
Key Research results
- Numbers of teeth by BMI in each age group
Linear trends were noted in each age group over the 40s, i.e., a higher BMI is associated with fewer residual teeth (Figure 1). Obese people under 50 when teeth loss begins are more likely to lose teeth.
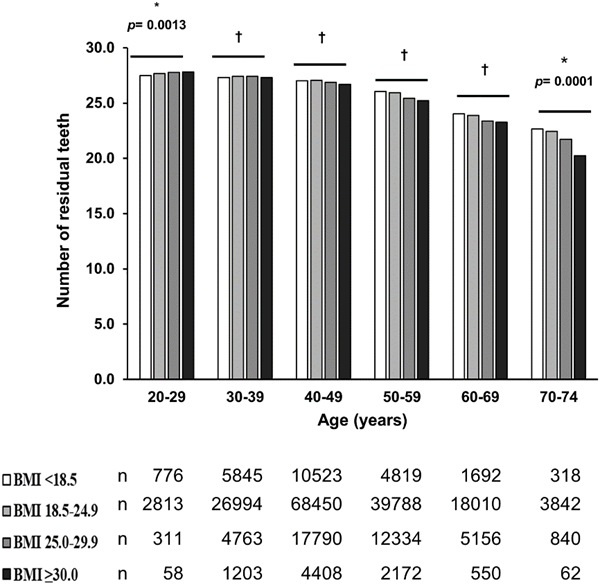
Fig 1. Numbers of teeth by BMI in each age group
- Percentages of people with teeth by presence or absence of obesity and tooth position
Obese people (BMI ≥25; bottom) lost teeth at more tooth positions and had significantly fewer molars (posterior teeth) and maxillary central incisors at any age from 30s to 60s, than non-obese people (BMI <25; top). Most of the maxillary teeth showed a significant difference between obese and non-obese subjects from their 40s. The most significant decrease due to obesity was observed in the mandibular molars (Figure 2).
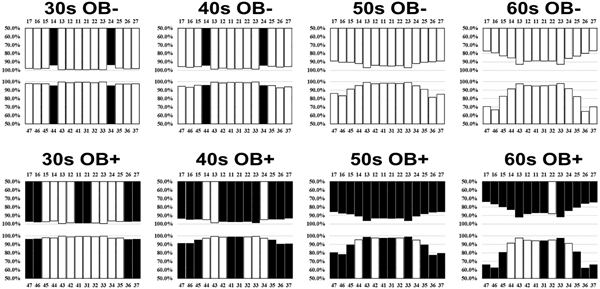
Fig 2. Comparison of the percentages of non-obese and obese people with residual teeth by age
The percentages of having residual teeth are shown for obese and non-obese people. A shorter bar indicates a lower percentage of having residual teeth and a higher likelihood of tooth loss. Positions with significantly lower likelihoods of having residual teeth (p <0.05) are shown in black.
Smoking, in addition to obesity, increased the positions of significant tooth loss, demonstrating tooth loss in different positions from those due to obesity alone.
- Risk factors for having fewer than 24 teeth
To examine whether obesity is an independent risk factor for having <24 teeth, logistic regression analysis was conducted with four models adjusted for other risk factors.
Model 1; BMI ≥25.0
Model 2; Model 1 + Sex and Age
Model 3; Model 2 + Smoking habit
Model 4; Model 3 + HbA1c ≥6.5
As a result, the odds ratios for BMI ≥25.0 were 1.47 (95%CI: 1.43-1.52), 1.39 (95%CI: 1.35-1.44), 1.39 (95%CI: 1.34-1.44), and 1.35 (95%CI: 1.30-1.40), respectively, demonstrating that obesity is an explanatory factor for residual teeth (<24 teeth) independent of other risk factors, such as smoking and diabetes.
CONCLUSION
Preventing tooth loss, chewing food well, and having good dietary habits help maintain the quality of life (QOL) and promote general health. The research based on real-world big data demonstrates that obesity, a risk factor for various diseases, accelerates tooth loss at a relatively young age. People with obesity should be encouraged to prevent tooth loss and maintain good health by visiting the dentist early to treat periodontal disease and caries and by caring for their molars with a proper oral hygiene routine.
Title: Real-world evidence of the impact of obesity on residual teeth in the Japanese population: A cross-sectional study. Authors: Mayu Hayashi, Katsutaro Morino, Kayo Harada, Itsuko Miyazawa, Miki Ishikawa, Takako Yasuda, Yoshie Iwakuma, Kazushi Yamamoto, Motonobu Matsumoto, Hiroshi Maegawa, Atsushi Ishikado.











