INTRODUCTION
Dental professionals must recognize that more than 90% of systemic conditions appear in the mouth—autoimmune conditions such as Sjögren’s syndrome, lupus, sarcoidosis, diabetes, HIV, and hematological issues. Crohn’s disease can present in the mouth before gastrointestinal symptoms, as can numerous other conditions. I have had the opportunity to diagnose many of these disorders over the years and work with many of my patients’ other healthcare providers to improve patient outcomes.
The clinical presentation of a patient with Sjögren’s syndrome, an autoimmune condition, is the hallmark symptom of dry eyes and mouth. Whether the patient has had a definitive diagnosis or not, the eyes often feel gritty, burned, and itchy. The mouth can feel as though it is full of cotton, making it difficult to swallow or speak. In Sjögren’s patients, the moisture-secreting glands of the mouth and eyes tend to be affected first, resulting in a decrease in saliva and tears. Furthermore, as dental professionals, we may be the first to make that connection.
Sjögren’s syndrome is an immune system disorder often accompanied by other immune system disorders, such as lupus and rheumatoid arthritis. The patient highlighted in this article denied having other conditions. This syndrome typically occurs in females over 40 years of age. Other findings associated with this disorder include:
- Dry skin or rashes
- Persistent cough
- Prolonged fatigue
- Joint pain, swelling, and stiffness
- Swollen salivary glands, especially around the jaw and ears
CASE REPORT
Our case study is of a 44-year-old black female who is a pediatrician, wife, and mother of 2. The patient presented with a chief dental complaint of dry mouth and generalized sensitive teeth. Upon review of the patient’s health history, she noted a positive history of Sjögren’s syndrome and gallbladder removal in 2018. Sjögren’s syndrome was diagnosed 10 years prior with no other significant findings.
Clinical Presentation
The patient seemed to squint her eyes often. This observation was seen at the first appointment and every visit afterward. She was experiencing the common symptom of dry eyes, causing discomfort and difficulty with her vision.
My clinical examination was conducted through the lens of my practice model, prioritizing health, function, and aesthetics.
Health
The health examination found the following:
- Extensive decay involving multiple surfaces of the entire dentition
- Moderate periodontal disease with generalized inflammation and pocketing
- Radiographic bone loss
- Dry mouth
- Dry eyes
- Gingival recession
Function
The examination found the following functional issues:
- Lack of canine guidance with tooth No. 11
- Malocclusion that resulted in bruxism, numerous abfraction lesions, pitting, and fractures of teeth
- An anterior open bite
Aesthetics
The patient’s smile was determined as:
- Aesthetically pleasing with slight evidence of asymmetry (Figure 1a)

Figure 1a

Figure 1b.

Figure 1c

Figure 1d—Figure 1. (a) Original beautiful smile with asymmetry. (b) Patient demonstrates anterior open bite in CO; crowding in the mandibular anterior region; severe gingival inflammation, especially in the mandibular arch; and gingival recession. (c) Image showing root decay in the lower right premolar and gingival inflammation. (d) Image demonstrates bimaxillary protrusion, root decay, and gingival inflammation.
Clinical Approach
Health: My approach to restoring health is by addressing oral disease and systemic involvement.
The primary focus includes periodontal therapy (salivary testing, SC/RP, laser therapy, StellaLife Oral Rinse (StellaLife), and oral/gut probiotics (ProBiora). After the treatment, 6-week and 3-month followups are required. Then regular, 3-month hygiene appointments are needed. This patient must be diligent about her oral health practices, as well as using products to stimulate salivary production.
Carious elimination: Caries were removed with a ceramic bur (CeraBur K1SM [Komet]). The steps to eliminate dental decay were as follows: LimeLite pulp material (Pulpdent) was placed. The teeth were etched, desensitized, and bonded, and ACTIVA BioACTIVE (Pulpdent) was placed as the core buildup material.
Functional Approach
This step occurred before all others.
- Before any restorative work, models were taken. The upper arch’s horizontal relationship was determined using a SAM 3 Articulator kit (Great Lakes Dental Technologies) with face-bow. The patient was deprogrammed with a leaf gauge for 15 to 20 minutes, and centric bite records were taken.
- A minimal slide from CR to CO was identified. The discrepancy was eliminated on the cast and teeth.
- Select teeth are sometimes equilibrated to create a more balanced occlusal scheme. The preliminary work of deprogramming; taking a centric bite; mounting; and adjusting the cast and teeth, if needed, is critical to understanding if the muscles, joints, and teeth are functioning in harmony prior to fabricating temporaries and finalizing restorative work.
Treatment of Aesthetics: Maintain Beautiful Aesthetics
There was no cosmetic wax-up done for this case. The patient desired no change of aesthetics. However, in hindsight, I would reconsider this decision due to the complexity discovered when making the chairside temporaries for this case.
Restorative Approach to Care
The case was completed in phases due to the extent of treatment needed and the decision to spread the financial commitment over 12 to 14 months. The total investment was approximately $50,000.
First Appointment
Complete charting was completed, digital /intraoral images were taken, an FMX series was taken, and periodontal charting was completed. The length of the first appointment was approximately 1.5 hours.
Digital imaging showed:
- Anterior openbite, CO (Figure 1b)
- Bimaxillary protrusion (Figure 1c)
- Crowding in the mandibular anterior region (Figure 1b)
- Severe gingival inflammation, especially in the mandibular arch (Figures 1b to 1d)
- Gingival recession (Figure 1b)
- Root decay (Figures 1b and 1d)
Intraoral images: When taking intraoral imaging, 3 surfaces of each tooth were captured: the buccal, occlusal/incisal, and lingual surfaces (Figures 2 and 3). The following issues were then seen:
- Abfraction with decay (Figures 2a and 2b)
- Abfraction lesions (Figures 2c and 2d)
- Occlusal pitting (Figure 3a)
- Occlusal wear (Figures 3b and 3c)
- Decay (Figures 3b and 3d)

Figure 2a
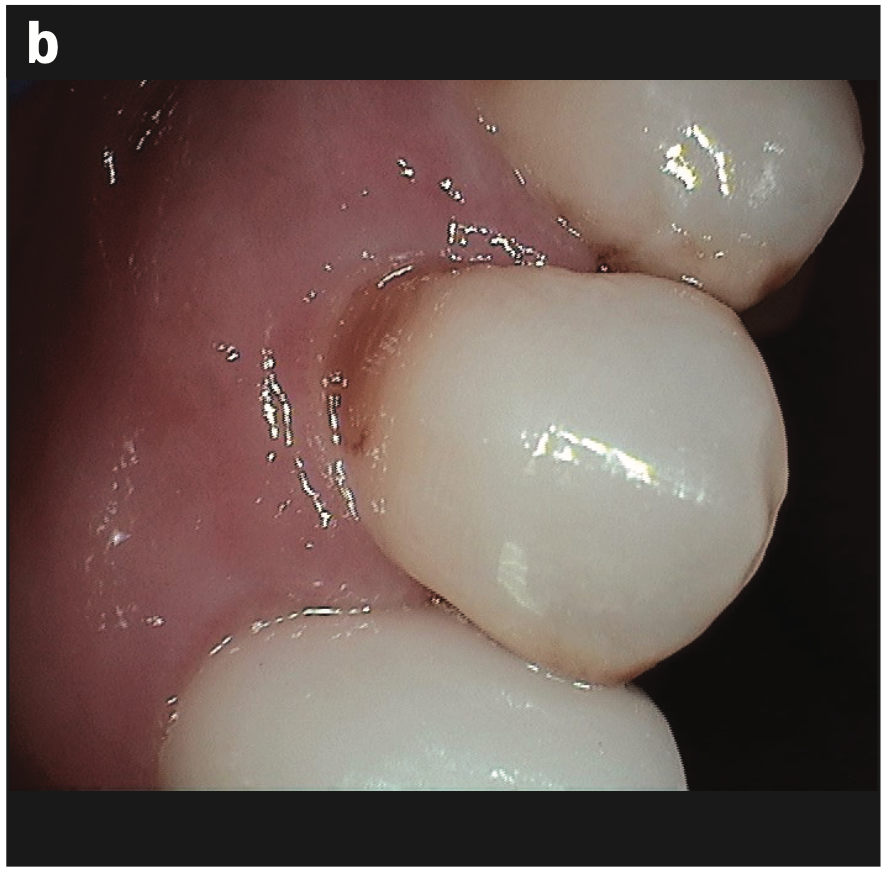
Figure 2b

Figure 2c

Figure 2d—Figure 2. (a and b) Abfraction with decay. (c and d) Abfraction lesions.

Figure 3a

Figure 3b

Figure 3c

Figure 3d—Figure 3. Occlusal (a) pitting, (b) wear, (c) fracture, and (d) decay.
These images are a small sample of the damage caused by the malalignment and rampant decay.
Documentation: These comprehensive cases must be documented thoroughly. Documentation is needed for several reasons. The reasons are as follows:
- As evidence of how the patient presented
- Used for patient education
- Needed for liability reasons
- Required for insurance submission
- Used to show before and after images
First Phase of Treatment
Imaging: The maxillary and mandibular anterior regions were addressed first to establish proper anterior and canine guidance. No cosmetic or functional wax-up was done for this case. Therefore, chairside temporization with the correction of any discrepancies was required at the preparation appointment for Nos. 6 to 11 and Nos. 21 to 28 (Figures 4a to 4c) and the smile shot (Figure 4d).

Figure 4a

Figure 4b

Figure 4c

Figure 4d—Figure 4. (a) Restored teeth Nos. 6 to 11 and Nos. 21 to 28. (b) Right lateral view of restored teeth. (c) Left lateral view of restored teeth. (d) Smile view of phase 1 treatment.
First Step of Treatment
Carious Elimination/Crown Preparation: The armamentarium for crown buildups is as follows.
- Use of ceramic burs (CeraBur K1SM)
- Use of LimeLight cavity liner, which stimulates secondary dentin formation, provides benefits of calcium hydroxide, and sets extremely hard
- Use of a desensitizer (Hurri Seal [Beutlich Pharmaceuticals]) and bond (Scotchbond Universal Adhesive [3M])
- Use of ACTIVA BioACTIVE; this material is wear- and fracture-resistant, seals against microleakage, releases fluoride, and is easy to prepare
- Conservative, ideal crown preparations
- Chairside temporaries were fabricated using Luxatemp (DMG America); we needed to maintain beautiful aesthetics with the chairside temporaries while creating an ideal alignment and function
Second Phase
This phase saw the completion of crown buildups and crown preparations and temporization for mandibular posterior teeth (Nos. 18 to 20 and 29 to 31).
Third/Final Phase and Completion of the Case
Crown buildup and crown preparations were done (Nos. 2 to 5 and 12 to 15).
Final Results
- Canine guidance was restored (Figures 5a and 5b)
- The aesthetics were maintained (Figure 5c)
- The maxillary and mandibular occlusal views show the arch harmony (Figures 5d and 5e).

Figure 5a

Figure 5b

Figure 5c

Figure 5d

Figure 5e—Figure 5. (a) Canine guidance restored. (b) Lateral view. (c) Aesthetics maintained. (d) Occlusal view of the maxillary arch. (e) Occlusal view of the mandibular arch.
CONCLUSION
There is no definitive answer to why autoimmune conditions develop, but there is evidence of their deleterious effects in the oral cavity. Dentists often treat patients who have conditions such as Sjögren’s syndrome, a condition that disturbs the oral microbiome and contributes to oral issues, such as decay and periodontal disease. So often, these patients suffer from constant discomfort and oral problems with no hope for resolution.
The decision to treat this patient comprehensively with the consideration of health, function, and aesthetics was based on numerous factors. The patient was receiving limited care over the years that required numerous fillings that only addressed 1 or 2 surfaces of decay, leaving the other areas untreated. The patient was living with constant sensitivity, with only limited options being offered. The decision to do complete dentistry corrected rampant decay, periodontal disease, and malalignment while maintaining her beautiful aesthetics.
Throughout the treatment, the patient was required to use saliva replacement and fluoride trays. These cases require a strong partnership between the dental professionals and the patient in order for them to be successful. For the patient, it requires a commitment to good oral hygiene, 3-month recall visits, use of products, and maintaining visits with other physicians to ensure long-term success.
As dentists, we must see ourselves as physicians of the oral cavity who must research these conditions, present options for care, and deliver high-quality dentistry. My patient and her husband were ecstatic with the process and the final results. The couple’s excitement throughout and following treatment has led to numerous referrals of patients to my practice who seek complete care. My practice model of health, function, and aesthetics and my philosophy of building relationships and trust has been paramount in supporting patients through their journeys of seeing dentistry as a branch of medicine.F
ABOUT THE AUTHOR
Dr. Glasper received her DDS degree from Howard University in Washington, D.C., and completed her postgraduate residency program at the University of Medicine and Dentistry in New Jersey. Dr. Glasper’s postgraduate work has included training with some of today’s most renowned restorative and cosmetic dentists. Dr. Glasper teaches dental continuing education courses for dentists and their teams across the country, sharing her passion, knowledge, and skills in the area of comprehensive dentistry. She leads the “Teach Me Dental” movement, which is redefining how the public understands and treats their dental health. In 1999, she opened her practice at Revive Dental Cosmetic & Restorative Dentistry to serve patients in Marriottsville, Md and Ellicott City, Md, Dr. Glasper is a member of the ADA, AACD, and the Maryland State Dental Association. She can be reached at drglasper@gmail.com.
Disclosure: Dr. Glasper reports no disclosures.











