When a bone breaks, the immune system immediately gets to work, removing pieces of bone and killing germs. The body then forms a soft, protective callus to bridge the fracture while blood vessels grow into the area to assist with healing. Age, diabetes, and radiation treatment all impair that process, however, prompting Michigan Medicine and Kansas University to develop a device that accelerates bone healing.
“We are developing ways to allow bones to heal when they otherwise wouldn’t by looking at introducing blood vessels,” said University of Michigan surgery researcher and lead author Alexis Donneys, MD.
The approach delivers a combination of stimulants, hyaluronic acid and deferoxamine, into a fracture to grow bone. Small animal testing showed that the therapy dramatically accelerates bone healing after injury. If proven effective in human beings, the method could change outcomes for millions of adults who suffer broken bones that don’t heal, the researchers said.
Mark Cohen, MD, a University of Michigan surgery and pharmacy professor, had been working with Laird Forrest, PhD, a pharmacy professor at Kansas University, on an implantable hyaluronic acid drug delivery system to help cancer drugs reach their target. Colleagues at the University of Michigan then saw an opportunity to combine the technology with their insight in bone healing.
“This modified method for administering hyaluronic acid and deferoxamine with an implantable device eliminates the need for repeat injections,” said Donneys. “This is beneficial for patients since it eliminates pain and discomfort, potential for infection, and the time associated with multiple injections.”
Known as Ferroximend, the device delivers the stimulants gradually to the fracture site during the critical period of angiogenesis, which is when blood vessels develop. The device earned the University of Michigan Department of Surgery’s 2018 Michigan Surgical Innovation prize. Also, research suggests a role for deferoxamine in bone repair by inducing bone vessel growth, but its current use is in treating iron overload.
“The data thus far demonstrates that the HA-DFO hyaluronic acid and deferoxamine combination improves upon the use of either compound used singly at the fracture site,” said Donneys.
For children and adults, a broken bone means weeks or months of recovery. But for the elderly and for those who have experienced radiation treatment for cancer, recovery is more difficult.
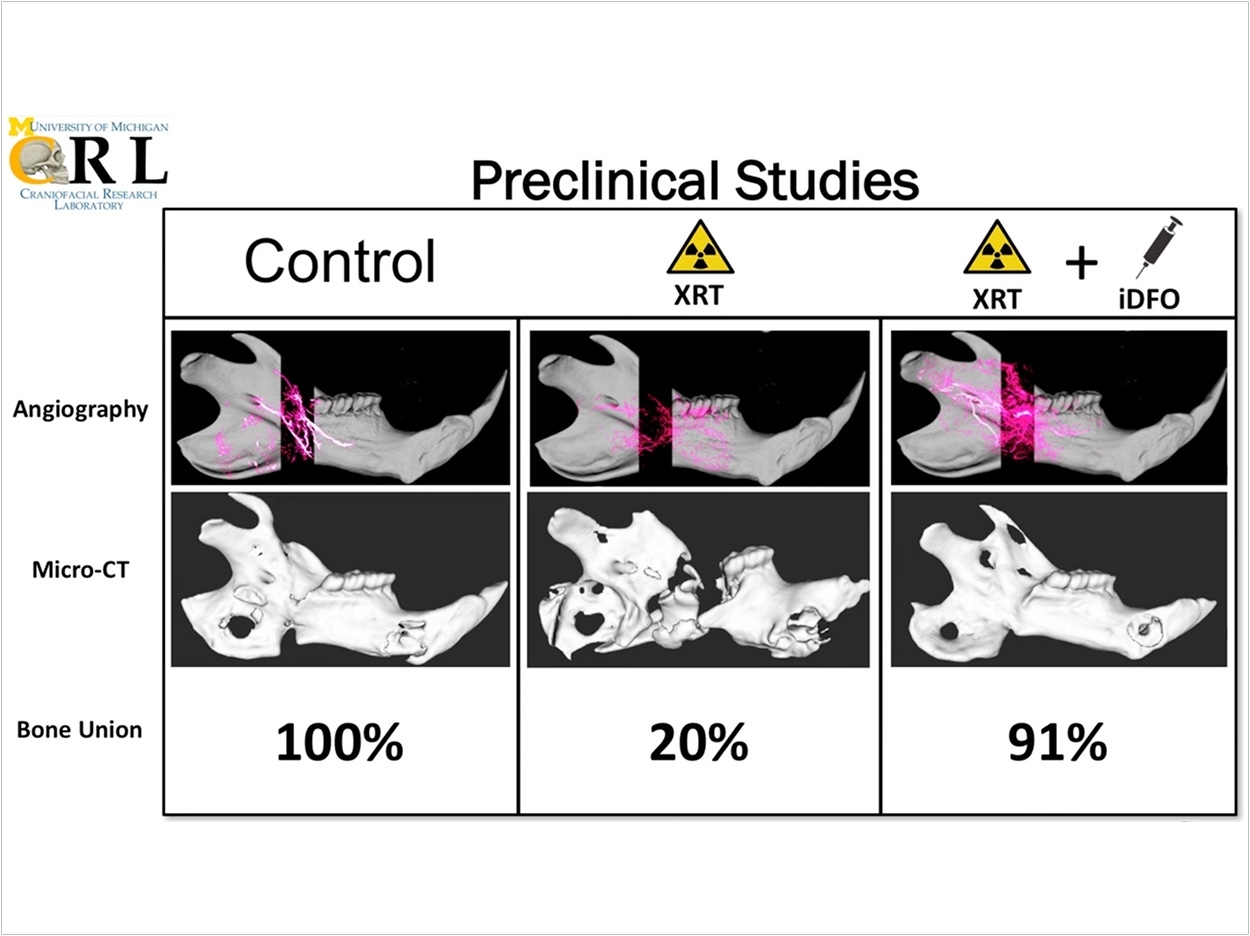
For example, late film critic Roger Ebert lost the lower part of his jaw due to complications from thyroid and salivary gland cancer treatment. Such large, complex bone wounds often require grafts and multiple surgeries, but just 20% of radiated bone fractures heal, according to the researchers. They also are difficult for doctors and patients to content with.
“We want to do a lot better for patients to help avoid debilitating and disfiguring complications and to improve their quality of life in a way we haven’t seen yet,” said Donneys.
For the study, the researchers applied the hyaluronic acid and deferoxamine delivery method to bone fractures in animals that had undergone radiation, which is one of the most challenging healing processes. Animals with bone fractures treated with hyaluronic acid and deferoxamine had a 91% bone union rate, which was three times higher than untreated animals, the researchers said.
“If you can grow bone in nuclear winter, you can grow bone anywhere,” said Steven R. Buchman, MD, craniofacial plastic surgeon at Michigan Medicine and study coauthor.
As the University of Michigan surgeons looked for bright ideas for commercialization, the experimental device had the most promise for improving patient care. Next, the surgery team will use funding, guidance, and feedback from its Innovation Prize to focus on preclinical studies and regulatory strategies. One day, the researchers hope to see Ferroximend used in operating rooms.
“While most of us were surgically and scientifically skilled, it really felt like we were back in the classroom learning something completely new,” said Donneys of the University of Michigan’s Surgical Innovation Development Accelerator Course and prize competition. “The difference was, this time, the lessons we learned could make a bid difference in improving surgical practice and patients’ lives on a larger scale.”
The study, “Implantable Hyaluronic Acid-Deferoxamine Conjugate Prevents Nonunions Through Stimulation of Neovascularization,” was published by Regenerative Medicine.
Related Articles
Hydrogel Shows Promise in Treating Bone Defects
Biomaterial Fuels Bone Healing With Less Rejection
Scaffold Technology Improves Craniofacial Bone Regeneration












