INTRODUCTION
Certain glass polyalkenoate (ionomer) systems have proven to be excellent dentin replacement liners and bases for decades in biomimetic stratification tooth repair.1 The resin-modified glass-ionomer cements, particularly, are well suited to that purpose. Now there is a worthy alternative. Since its introduction in January 2021, TheraBase (BISCO) has been proving itself as an excellent radiopaque, bonded dentin replacement base/liner.2 The company refers to the material as a “dual-cured, calcium- and fluoride-releasing base, self-adhesive base/liner.” TheraBase is packaged in a double-barrel syringe with a self-mixing delivery tip that is used to inject material directly into a cavity preparation. Another method of delivery comes from mixing pad spatulation and using the AccuDose syringe system (CENTRIX). Simulated delivery of the material and photo-polymerization in an extracted molar is shown in Figures 1 to 3.
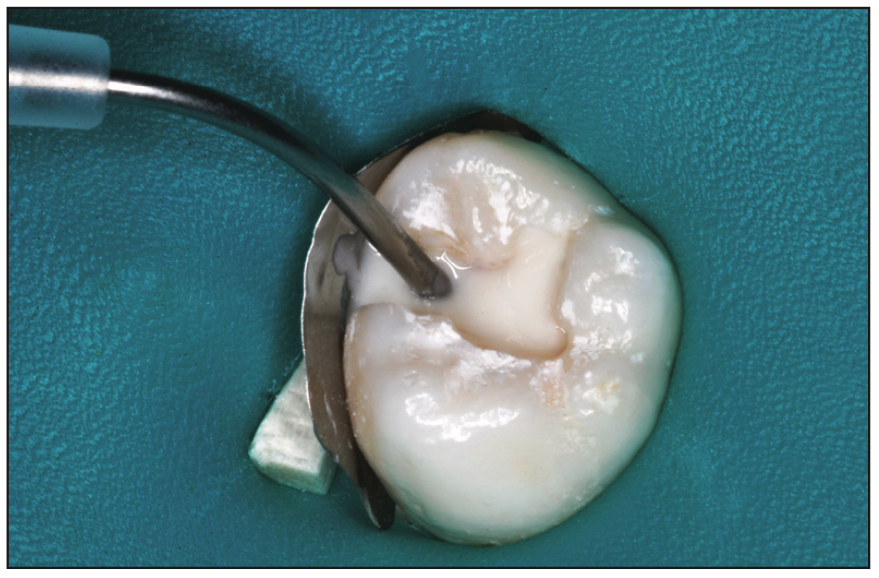
Figure 1. Beginning injection with the double-barreled delivery/mixing system in an extracted tooth simulation.
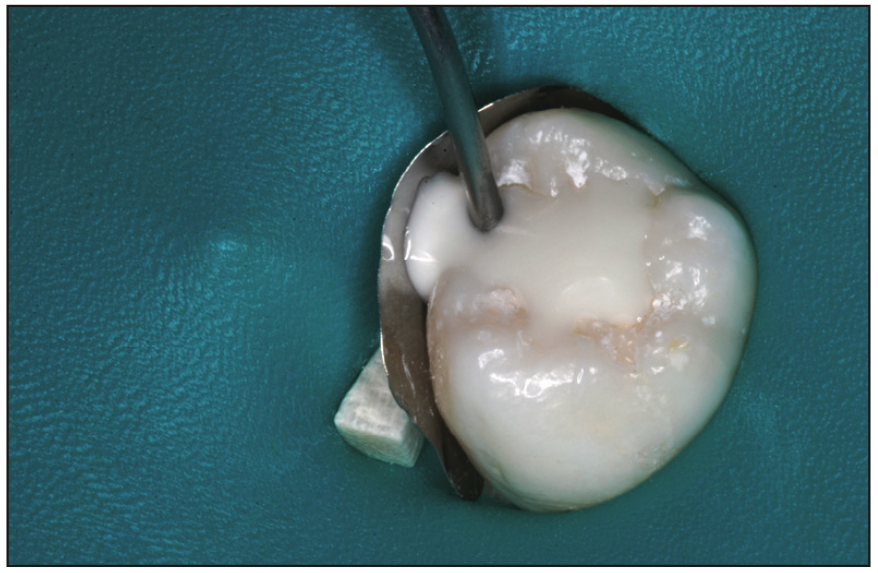
Figure 2. Injection of TheraBase (BISCO) to overfill to serve as a dentin/enamel interim restoration.
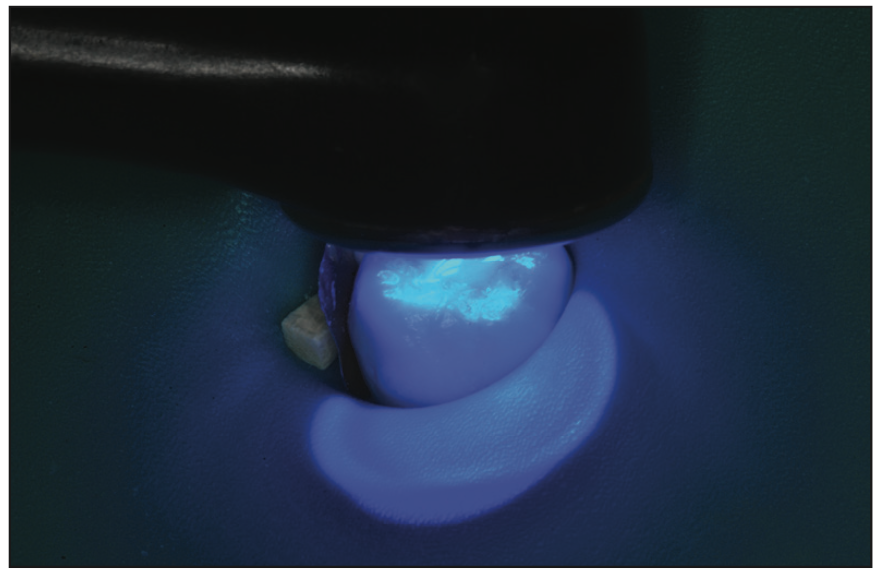
Figure 3. Photo-polymerization followed by chemical curing of the material. Trimming with appropriate burs followed.
The manufacturer’s material safety data sheets fully describe the makeup of TheraBase, which consists of tricalcium silicate (Ca3SiO5), dicalcium silicate (Ca2SiO4), tricalcium aluminate (Ca3Al2O5), and calcium aluminoferrite (Ca4AlnFe2-nO7) and a photopolymerizing resin component.3,4 MDP (10-methacryloyloxydecyl dihydrogen phosphate) is also included as a bonding agent for chemical adhesion to tooth substrates.5,6
Currently, calcium silicate/calcium aluminate cement materials offer an alternative to the glass-ionomer systems for dentin replacement liners/bases.7 BISCO’s “Thera” products are examples of such liner and base materials. In more than 2 years of clinical use in both primary and permanent teeth, we have discovered that, in addition, TheraBase can also be used as an interim restorative material, replacing both dentin and enamel. Traditionally, zinc oxide/eugenol (ZOE), reinforced ZOE, and many of the glass-ionomer cement systems are used in that manner. TheraBase is now proving itself to be a worthy alternative. Following the repair of dozens of primary molars meeting certain criteria, permanent teeth needing “temporization” observations in clinical practice show that the material does not exhibit early wear, fractures, or erosion. This article presents typical examples of such uses of this material.
TECHNIQUE FOR PLACEMENT
- Cut a cavity preparation in the same design for resin-based composite or glass-ionomer cement, including mechanical undercutting.
- Clean the preparation of all debris with water spray.
- Remove excess moisture with air spray, there is no need to completely dry surfaces to the point of desiccation.
- In the mouth, disinfect the cavity preparation with a solution such as Gluma (Kulzer) or MicroPrime (Zest Dental Solutions).8,9
- Mix and inject material to overfill from the bottom up in the preparation and with care to avoid air entrapment.
- Apply the light beam for 20 seconds (no need to inject and cure in segments due to the chemical cure).
- Trim to the desired contour and adjust the bite to ensure against impacting occlusal forces.
DISCUSSION
With 2 years of use of TheraBase as an interim restorative material for replacing dentin and enamel, we cannot predict long-term resistance to fracture, wear, or erosion of the material when used as described here. However, in our early observations, we have seen no such material damage. In vitro laboratory experimentation and in vivo clinical studies would be useful to determine the capabilities of TheraBase interim restorations over time. However, in cases of primary teeth that have limited time before exfoliation (1 to 3 years), TheraBase could be a reliable, durable, and extremely easy-to-use temporization material (Figures 4 to 8). In addition, it features excellent radiopacity (Figure 9). This material also shows promise as a rapid stop-gap solution in permanent teeth requiring a quick and easy repair in office emergency scenarios or in any clinical circumstance when a delay is needed until more long-term treatment can be pursued (Figure 10). Examples are a temporary fill of an endodontic access opening or interim repair of a tooth with a sensitive caries lesion, with or without enamel hypoplasia/hypocalcification. Partially erupting permanent teeth exhibiting caries lesions can also be temporarily treated with TheraBase, such as the molar shown in Figure 11. When TheraBase was placed in that tooth one year prior, one-half of the crown was covered by the soft-tissue operculum, and short of an operulectomy, access was limited. Figures 12 and 13 show 8- and 10-month postoperative images of emergency repairs in patients. Figure 14 is a montage of 6 primary and permanent molars, all of which had been repaired with TheraBase 12 to 24 months post-op.

Figure 4. Four months after mesial-occlusal repair of a second primary molar in an 11-year-old.

Figure 5. Seven-month-old mesial-occlusal-distal TheraBase repair in a 12-year-old.

Figure 6. Eight months after Class II repair of 2 primary molars in an 11-year-old.

Figure 7. Eight-month-old “MOD” interim repair of a primary second molar in a 12-year-old.

Figure 8. Ten months after silver diammine fluoride caries attenuation and TheraBase repair in a 9-year-old.
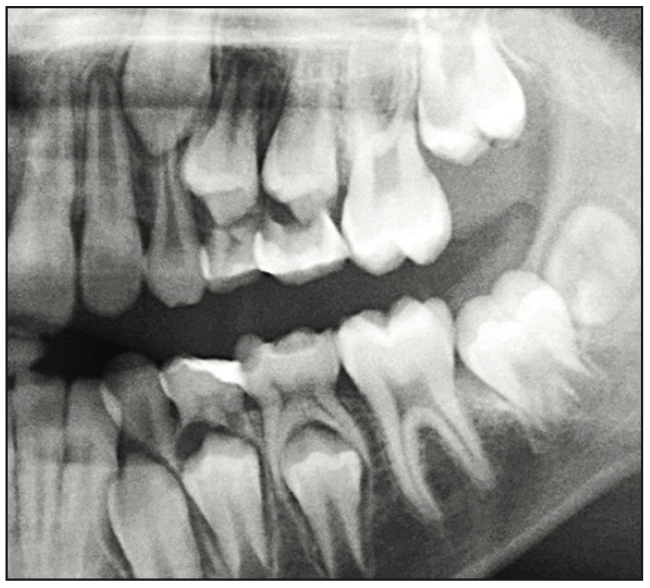
Figure 9. Radiographic view showing material radiopacity of 3 primary molars (2 shown in Figure 6), plus the mandib- ular primary first molar, near exfoliation, 10 months postoperatively.

Figure 10. Six months after an “emergency visit,” TheraBase repair of a sensitive carious tooth was done in a 19-year-old.

Figure 11. A permanent second molar in a 13-year-old was partially erupted when interim repair was needed one year prior.

Figure 12. Interim emergency premolar repair, 8 months post-op, after a 16-year-old patient fractured a disto-occlusal resin-based composite (RBC) restoration.

Figure 13. Emergency TheraBase restoration 10 months post-op after a 19-year-old patient fractured a mesial-occlusal-distal RBC. Residual RBC is seen at the margin.
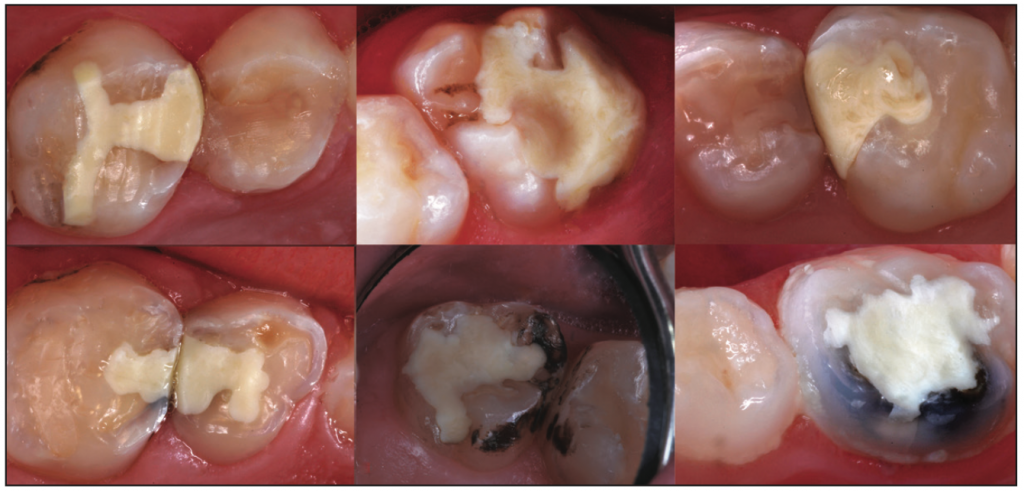
Figure 14. A montage of 6 permanent and primary molars that had been repaired with TheraBase 12 to 24 months post-op.
REFERENCES
1. Croll TP, Cavanaugh RR. Posterior resin-based composite restorations: a second opinion. J Esthet Restor Dent. 2002;14(5):303–12. doi:10.1111/j.1708-8240.2002.tb00526.x
2. Cannon ML. A 21st-century material for all deep restorations. Inside Dentistry. 2022; 18(8):44–5.
3. BISCO. TheraBase Base Safety Data Sheet. https://www.bisco.com/assets/1/22/TheraBase_Base_SDS_US_English.pdf
4. BISCO. TheraBase Catalyst Safety Data Sheet. https://www.bisco.com/assets/1/22/
TheraBase_Catalyst_SDS_US_English.pdf
5. Kuraray Dental. MDP Monomer. May 13, 2018. Accessed January 26, 2022. https://
kuraraydental.com/clearfil/key-technologies/mdp-monomer/
6. Lively T. What is MDP and why is it an MVP for bonding? Dental Products Report. 2021;55(11).
7. Primus C, Gutmann JL, Tay FR, et al. Calcium silicate and calcium aluminate cements for dentistry reviewed. J Am Ceram Soc. 2021;105(3):1841–63. doi:10.1111/jace.18051
8. Christensen R. TRAC Research: Disinfection of tooth preparations—why and how? Clinicians Report. 2009;2(11):1-2.
9. Christensen R. Focus On: Tooth preparation disinfection. Dent Today. 2014;33(3):16.
ABOUT THE AUTHORS
Dr. Croll is the clinic director of Cavity Busters Doylestown in Doylestown, Pa; an adjunct professor of pediatric dentistry at the Dental School at the University of Texas Health Science Center at San Antonio; and a clinical professor of pediatric dentistry at the Case Western Reserve School of Dental Medicine in Cleveland. He can be reached at willipus@comcast.net.
Dr. Gutmann is professor emeritus at the Texas A&M University College of Dentistry in Dallas and a distinguished adjunct professor in the Department of Cariology at Saveetha Dental College and Hospital in Chennai, India. He can be reached at jlg4570@aol.com.
Dr. Lawson is the director of the division of biomaterials and program director of the biomaterials residency program at the University of Alabama at Birmingham School of Dentistry. He can be reached at nlawson@uab.edu.
Disclosure: Dr. Lawson receives research and honoraria from BISCO, Kulzer, and other companies not mentioned in this article. Drs. Croll and Gutmann report no disclosures.











