
I have been an advocate of dental lasers for a long time. I saw the potential for the technology but was frustrated because I could never fully realize the impact clinically. I’ve found that dentists tend to shy away from dental lasers for hard-tissue procedures in general because of experiences that were less predictable than expected with erbium lasers. I also used an erbium laser, but needed much more anesthesia-free predictability from the device and found hemostasis often difficult to achieve.
Last year, I decided to invest in Solea, a 9.3-μm carbon-dioxide (CO2) dental laser from Convergent Dental. This technology has made vast improvements over previous generations of erbium lasers because of the unique waveform. I have expanded the scope of procedures that I can perform while achieving predictable anesthesia-free results and delivering a better clinical experience overall for my patients. Here are three specific cases that demonstrate the benefits of utilizing a 9.3-μm CO2 dental laser for hard-tissue procedures.
Multiple Interproximal Carious Lesions
Recently, I met with a patient who presented with multiple interproximal carious lesions. The deepest was on tooth No. 3 MO (Figure 1). I was able to perform the entire procedure solely with my dental laser, with no injection or high-speed/low-speed handpiece. No anesthetic was used, and the entire procedure only took around 35 minutes.
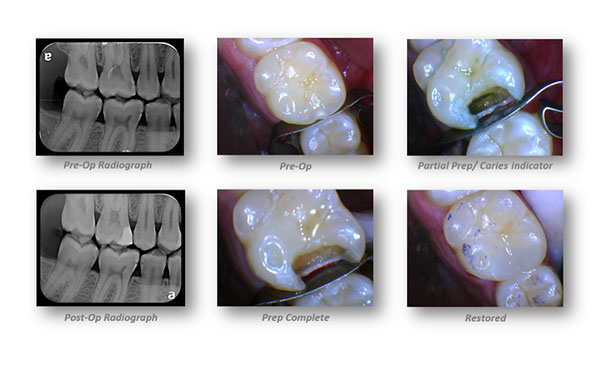 |
| 1. In this laser-only Deep Class II restoration, there was deep decay in No. 3 MO. The procedure involved a pre-op look at the tooth, followed by partial prep with a caries indicator, and a post-op radiograph of the restored tooth, along with laser-only preparation and restoration. |
This procedure was advantageous with the use of a dental laser versus traditional tools for a number of reasons. A significant amount of time was saved because there was no injection and no time spent waiting for anesthetic to set in. Because local was not needed, the occlusion was accurately checked and the patient did not need to come back for an adjustment. In addition, eliminating the noise, rattling, and vibration associated with the drill enhanced the patient’s experience. The procedure was a success from every perspective.
Crown Lengthening
A patient with a history of endodontic treatment presented with an ML fracture of tooth No. 30 to the level of the alveolus (Figure 2). The objective was to expose enough tooth structure to get a perfectly fitting crown and establish biologic width. I minimally flapped the tissue to be able to visualize and reshape the bone for proper osseous architecture. Next, I ablated the osseous tissue for bulk removal. I then finished the procedure with a piezoscaler to remove any bony spicules that were still attached.
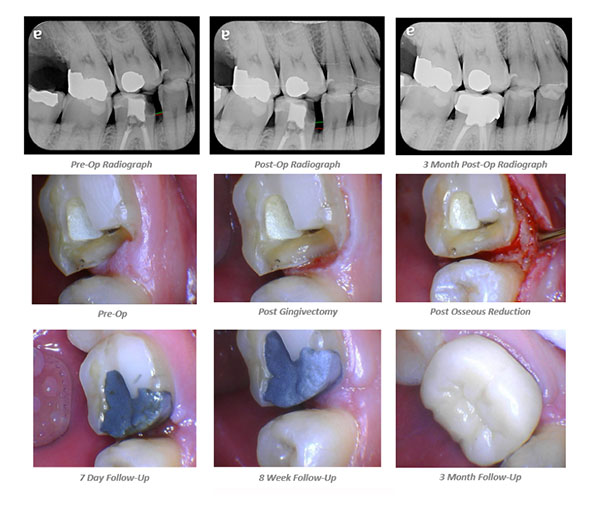 |
| 2. The pre-op radiograph of No. 30 in this crown lengthening procedure showed inadequate tooth structure coronal to alveolar bone. The post-op radiograph shows adequate coronal tooth structure after osseous reduction. The 3-month radiograph reveals the final crown insert. |
Previously, I would have had to refer this procedure out to a periodontist. Thanks to my laser, I was able to perform it within my practice, which the patient was very happy to hear.
Fractured Amalgam and Recurrent Decay
An exam revealed a fractured amalgam and recurrent decay on a patient’s No. 15 MOL (Figure 3). I began the procedure by using my laser to outline the amalgam until dentin was reached. The precision of the spot size also made it possible to create a trough adjacent to the amalgam without hitting the amalgam itself. I then removed the amalgam with a high-speed handpiece, as I was able to use the bur without anesthetic because of the analgesic effect achieved by starting with my dental laser. This simplified the entire procedure and delivered an excellent result.
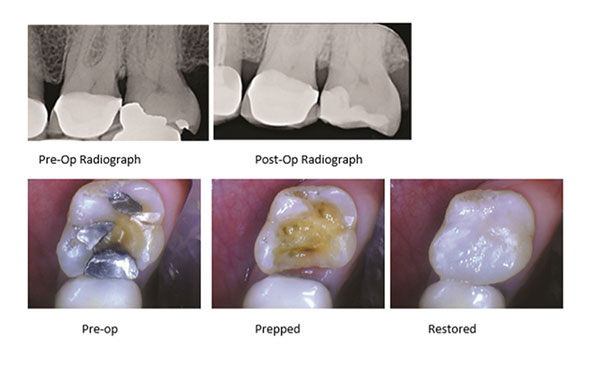 |
| 3. The third patient presented with fractured amalgam and recurrent decay in No. 15 that was treated with moderately deep restoration with the laser and composite. |
I never would have been able to perform this procedure without any anesthetic prior to using a 9.3-μm CO2 dental laser. With the Solea, however, my patient left the chair reporting no discomfort during or after the procedure and was thrilled to not feel numb.
Conclusion
These are only three examples of patients who left my chair smiling a little wider because their dental experiences were pain-free with my use of the Solea. My practice’s improved clinical outcomes, efficiency gains, and patient experiences have allowed me to practice in ways that I only could have dreamed of a few years ago.
 Dr. Joshua Weintraub graduated in 1992 from Clark University in Worcester, Mass, with a major in biology and continued his education at the University of Maryland Dental School, graduating in 1996. He started his dental career in the U.S. Navy Dental Corps as a lieutenant in Okinawa, Japan, followed by the Navy Yard in Washington, DC. He entered private practice in 1999 and has been utilizing dental lasers since 2008, including erbium and Nd YAG lasers. He currently uses a 9.3-μm CO2 Solea dental laser by Convergent Dental within his practice. Dr. Weintraub also has lectured internationally, including recently in Germany and Toronto.
Dr. Joshua Weintraub graduated in 1992 from Clark University in Worcester, Mass, with a major in biology and continued his education at the University of Maryland Dental School, graduating in 1996. He started his dental career in the U.S. Navy Dental Corps as a lieutenant in Okinawa, Japan, followed by the Navy Yard in Washington, DC. He entered private practice in 1999 and has been utilizing dental lasers since 2008, including erbium and Nd YAG lasers. He currently uses a 9.3-μm CO2 Solea dental laser by Convergent Dental within his practice. Dr. Weintraub also has lectured internationally, including recently in Germany and Toronto.
Related Articles
It’s Not Just Patients Who Hate the Needle











