
A dental impression is a negative imprint of the teeth and adjacent structures, as well as the first step in fabricating dental prostheses such as removable dentures and fixed restorations in addition to dental appliances such as mouth guards, whitening trays, retainers, and invisible aligners.
Traditionally, to take an impression, patients must visit dentists in their office. However, faster and more efficient treatments involving automated voice messages, texting, and online submissions with less human interaction seem to be favored by younger generations.
This leads to a question. Could patients safely and accurately take their own impressions in their home without the supervision of a dentist? There would be some benefits for the patient, who would save the time and cost associated with a dental visit, while dentists could re-center their attention and precious chair time on more demanding procedures.
But it also raises some concerns, mainly the safety of the patient who might choke or aspirate some foreign material. A secondary concern is related to the accuracy of an impression taken by a layperson.
Objectives
The objective of this study is to determine if a layperson can safely take adequate dental impressions of the maxilla and mandible using only the instructions from an Impression-Taking Guide(ITG) and an impression kit including trays, impression material, and gloves (Figure 1). These impressions were compared to those taken by a dentist to assess clinical acceptability.
Methods and Materials
A total of 55 patients were screened, and 53 patients met the inclusion criteria and were included. To be included, patients had to be at least 18 years of age. They also needed to be willing to provide voluntarily written informed consent. They had to be in good medical and dental health and able to tolerate the dental procedure. And, they had to have at least 24 teeth present.
 |
 |
| Figure 1. A typical impression kit includes trays, impression material, and gloves. | Figure 2. The most common reason for an unacceptable impression among the participants was the absence of gingival outline |
 |
 |
| Figure 3. Inadequate mixture of material was one reason for unacceptable impressions. | Figure 4. Some patients confused the upper and lower tray, leading to unacceptable impressions. |
 |
| Figure 5. Some patients applied inadequate pressure while seating the tray. |
Participants could not be dental professionals, nor could they or anyone in their immediate family be employed by the study’s sponsor. The exclusion criteria also included:
- Any known disease that interferes with taking dental impressions
- Ongoing orthodontic treatment
- Intraoral piercings that cannot be removed during an impression
- Ongoing cancer treatment
- Loose or mobile teeth
- A complete and/or partial denture
- Having less than 24 permanent teeth present
- Teeth with a history of self-reported preoperative pulpal problems
- Known difficulties breathing during a dental procedure
- Limited mental capacity and inability to give informed consent
- Condition affecting salivary flow, such as salivary gland disorder or Sjögren’s Syndrome
- Rampant caries
- Teeth requiring extraction for deep subgingival caries, fractures, or other conditions
- Evidence of acute periodontal infection such as an abscess, suppuration, severe swelling, or spontaneous bleeding
- Clinical signs and symptoms of periapical pathology
- Any other condition that, in the point of view of the investigator, may affect the ability of a subject to complete the study
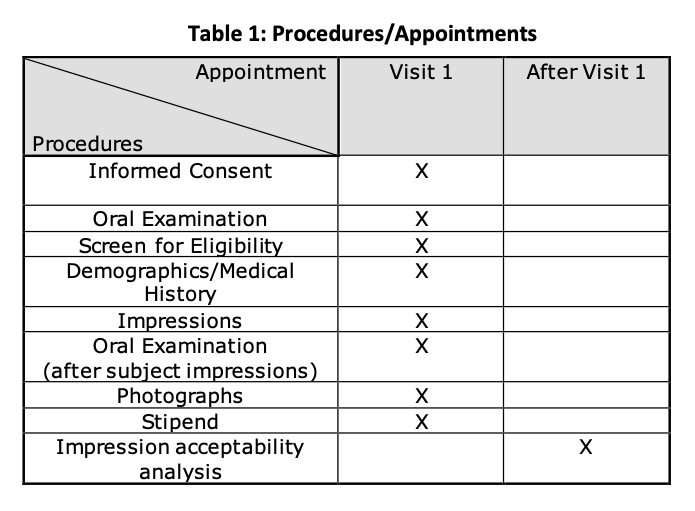
All participants signed informed consent forms, provided demographic information, and filled out a medical history questionnaire (Table 1). The study was approved by the Institution Review Board (IRB) at Tufts University School of Dental Medicine in Boston, Massachusetts. It also got an approval for the Informed Consent Form that was used to obtain consent from study participants.
 |
Subjects received a limited oral exam to participate in the study. They also were instructed to brush their teeth before taking photographs of a frontal view, maxillary occlusal view, and mandibular occlusal view.
Subjects started by taking two sets of impressions (two maxillary and two mandibular impressions), using putty impression material. They then followed the criteria outlined in the ITG, and the sequence of taking an upper or lower impression was randomized.
| Table 2 click here |
| Table 3 click here |
The working time for each impression was 120 seconds and the setting time was 150 seconds, which was observed by research personnel who did not provide instructions, answer questions, or intervene (except for safety reasons) with the subject while taking two sets of impressions.
At the end of the visit, all subjects’ questions were answered, and a limited oral examination was performed to determine if any residual impression material was left after the impression tray removal. Subjects were asked to rinse their mouths thoroughly using water to ensure there was no residual material left in their oral cavities.
Using the same criteria outlined in the ITG, the co-investigator took a set of maxillary and mandibular impressions that he considered to be clinically acceptable while under the supervision of the primary investigator. In cases where the impressions were not deemed acceptable, a second impression was obtained. Only the acceptable impressions were utilized in the analysis portion of the study. For routine disinfection, impressions were immersed for 10 to 15 minutes in disinfectant, or for an hour in case of increased risk of infection, followed by rinsing under running water for 15 seconds.
 |
Each subject had a total of six impressions, or in some instances eight impressions, taken. A sum of 324 impressions was taken: 162 upper impressions (108 by the subjects, 54 by the clinician) and 162 lower impressions (108 by the subjects, 54 by the clinician). Each impression was photographed and labelled with a master key known by the principal investigator only.
The photographs of the subjects’ dentition were organized and labelled with the same master key used to label the impressions. Subjects’ observations were recorded on the investigator observation form.
Results
Fifty-three patients with a median age of 28.44 (IQR = 7.44) had complete data for analysis. Thirty-three participants (62%) were female.
None of the participants experienced choking or allergic reactions from any of the impressions. Within the limitation of this study, it seems that there are no risk or safety-related issues associated with patients taking their own impressions (Table 2).
 |
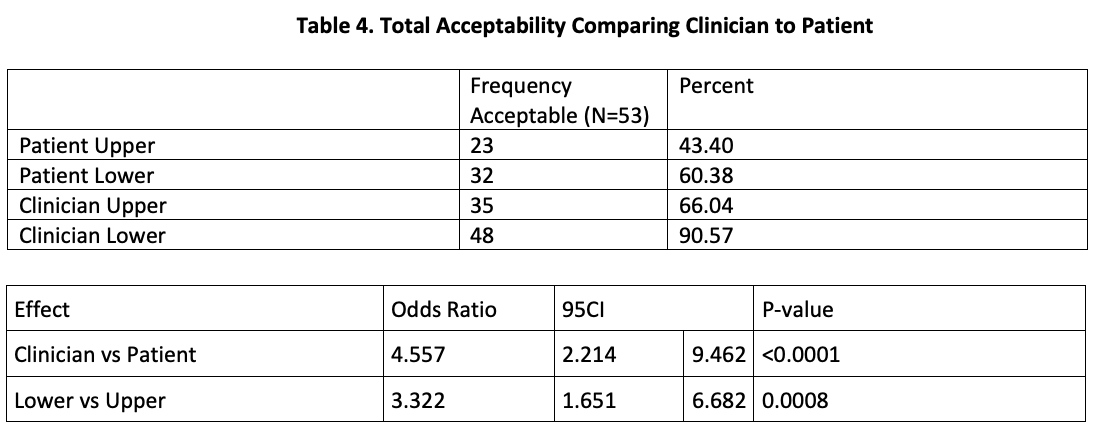
The accuracy and acceptability of impressions taken by the subjects were compared to those taken by the dental professional. Acceptable impressions needed to capture the gingival outline and posterior teeth without a double imprint or bubbles. Overall, the laypeople were able to produce acceptable maxillary and mandibular impressions approximately 50% of the time.
The most common reason for an unacceptable impression among the participants was the absence of gingival outline (Figure 2), which might be due to inadequate pressure applied on the tray, or due to the use of a smaller tray size compared to the arch size, avoiding complete seating of the tray.
Other reasons for an unacceptable impression among participants included inadequate material mix (Figure 3), participants confusing the upper and lower tray (Figure 4), and inadequate pressure applied during seating of the tray (Figure 5).
Twenty-three participants (43.40%) were able to make at least one completely acceptable maxillary impression, and 32 participants (60.38%) were able to make at least one completely acceptable mandibular impression. Thirty-five of the clinician-made maxillary impressions (66.04%) were completely acceptable. Forty-eight of the clinician-made mandibular impressions (90.57%) were completely acceptable (Tables 3, 4, and 5).
After controlling for impressions made for the same patient using a conditional logistic regression model, the odds of a clinician-made impression being acceptable were 4.6 times the odds for participant-made impression (95 CI = 2.214 – 9.462, p<0.0001). (P-value cannot be calculated when there are no discordant impressions, such as no change between first and second.)
Mandibular impressions were more likely to be acceptable. The odds of a mandibular impression being acceptable were 3.322 times the odds of a maxillary impression being acceptable (95 CI = 1.651 – 6.682, P = 0.0008).
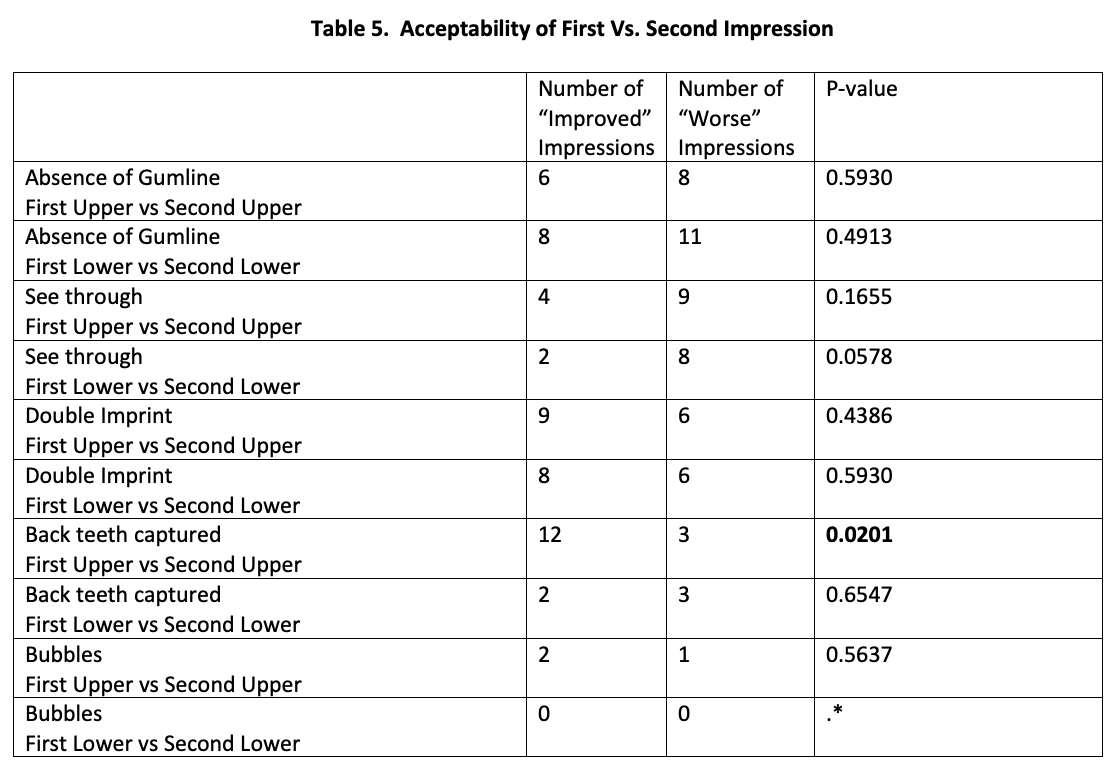
For each acceptability parameter, the first impression was compared to the second impression using McNemar’s test. There were no statistically significant differences except for capturing the back teeth for the maxillary impression. Participants were likely to improve capturing the posterior teeth of the maxillary impression in the second trial (P = 0.02).
Discussion
Onelimitation of the study was that patients were not seen by a periodontist, so there was no periodontal evaluation. Also, the study was limited to individuals with an average of 28 years, mostly females, which might necessitate the involvement of older ages in the upcoming studies for evaluation purposes (Table 6).
 |
The subjects said that the instructions were clear and easily understood. However, some difficulties were reported. For example, there were issues with the size of the gloves and trays. Hence, patients recommended including different sized gloves and trays in the kit.
Also, there were issues for patients in easily identifying the maxillary and mandibular trays. To avoid patients’ confusion between the maxillary and mandibular trays, color coding of the trays and adding the color key to the ITG was suggested.
There were issues in capturing the palate and oral vestibules due to insufficient pressure applied when seating the tray intraorally, overmixing the impression material, undermixed impression material, and uneven impression material mixture.
To avoid an inadequate impression mix, it was recommended that instead of directing the patient to mix the impression for a specific amount of time, the patient was better advised by the ITG to mix the impression until the mix becomes homogenous with no color streaks to ensure proper mixing.
Additionally, the amount of pressure that should be applied during impression taking should be more clarified in the ITG, and it should be clarified that the trays need to be fully seated to capture the required oral tissues. Once again, it was recommended that extra tray sizes should be provided to help in avoiding incomplete seating of the trays—in case of small trays/larger arches—and to match all arches shapes and sizes.
Adding a link to a video demonstrating the procedure to the ITG will help patients better understand what oral structures are required to be captured by the impression and guide them through the procedure step by step.
Finally, after implementing these recommendations, adding a quality check in the dental labs before pouring casts will ensure that the impressions taken by the patients meet the minimal acceptable quality requirements.
Future studies are necessary to assess if the impressions taken by the patient could possibly be used to fabricate other dental appliances by a dental laboratory, eliminating the need for a patient to go directly to a dental office.
Conclusion
A layperson can take impressions to fabricate mouthguards, bleaching trays, invisible aligners, and other appliances that do not necessitate the capture of palate or oral vestibules, as these structures were the hardest to capture by the patients.
The inconsistency of patient-made impressions capturing the palate or oral vestibules means that fabricating orthodontic appliances using a layperson’s impression is still questionable. Nevertheless, not capturing the palate will eliminate the risk of having a gag reflex.
Future research is necessary to pour up the impressions and evaluate lab-processed appliances such as mouthguards and bleaching trays in the patient for fit, accuracy, comfort, and functionality.
In an era when everyone owns a smartphone, a smartphone application where the patient could create an account, take intraoral pictures, and send them over to the lab so it could get a better picture of the current oral health status, such as recession and gingival inflammation, would be of great benefit. However, pocket depth and mobility would not be evaluated.
Dr. Perry is the principal investigator. He is a professor of comprehensive care and director of the Dental International Students program at Tufts University School of Dental Medicine. He can be reached at ronald.perry@tufts.edu.
Mr. Fisselier is the co-investigator and a prosthodontics student at Tufts University School of Dental Medicine. He can be reached at francois.fisselier@tufts.edu.
Dr. Avrampou is the co-investigator and an assistant professor of prosthodontics at Tufts University School of Dental Medicine. She can be reached at maria.avrampou@tufts.edu.
Ms. Bedair is a student at Tufts University School of Dental Medicine. She can be reached at nadine.bedair@tufts.edu.
Related Articles
Move Fast and Break Teeth: Digital Medicine’s Lessons for Innovation
California Law Requires X-Ray Reviews Before Orthodontic Treatment
What You Should Tell Your Patients About Mail-Order Orthodontics











