In this age of anxiety, pain control and sedation have become important aspects of dental care. It is now becoming more common for general practitioners to provide in-office sedation for routine dental procedures. A segment of the population that would otherwise not seek care because of fear or anxiety is now receiving treatment. The use of sedation for dental care has become a topic of intense interest, and many states are re-writing their regulations to require a special permit to provide this service. The intent of this article is to introduce definitions and concepts pertaining to oral sedation that may be helpful to the general dental practitioner.
|
Table 1. Indications and Contraindications for the Use of Anxiolysis |
||||||||||||||
|
(1) Anxiolysis is a technique that all dentists could implement. Many states (and provinces in Canada) have now developed restrictions on the use of conscious sedation by dentists, thereby limiting the ability to perform needed sedation for certain procedures. These restrictions mostly prevent dentists from administering conscious sedation without a special permit, usually one that requires training in intravenous drug administration. However, as defined above, anxiolysis is permitted in all 50 states and in Canada. (Those dentists who are interested in conscious sedation should consider continuing their sedation training and satisfy their state requirements for a conscious sedation permit).
(2) Anxiolysis provides a light level of sedation. A situation may arise in which the dentist and/or patient desires a lighter level of sedation than conscious sedation provides. An example may be the slightly anxious patient who states that they need the “edge taken off” in order to receive treatment. Anxiolysis could be appropriate for this situation. Many patients in general practice presently benefit from a medication given preoperatively, ultimately helping them relax for a perceived invasive procedure.
(3) Anxiolysis is ideal for shorter sedation appointments. Typical anxiolysis protocol consists of an oral medication given pre-operatively. Some newer sedation medications have short durations, and when given orally, can be effective for a short appointment. If, for instance, the expected length of the procedure is 90 minutes or less, anxiolysis may be indicated. It should be noted, however, that anxiolysis may also be appropriate for longer appointments, up to and sometimes exceeding 4 hours (see Table 1).
ANXIOLYSIS VERSUS CONSCIOUS SEDATION
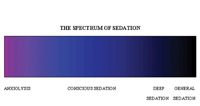 |
| Figure 1. Spectrum of sedation. |
 |
 |
 |
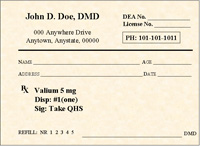 |
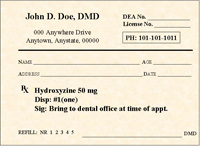
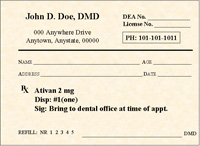
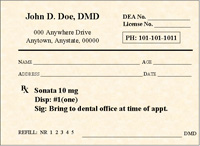
| Figures 2 through 5. Sample anxiolytic protocol prescription. |
There is no clear demarcation between anxiolysis and conscious sedation. Theoretically, all patients pass through a lighter level of sedation (anxiolysis) before entering conscious sedation. As such, the drugs used for anxiolysis produce conscious sedation to one degree or another if given in greater dosages, or in combination with other CNS-altering medications. The definition of anxiolysis involves a patient who can respond to verbal commands and maintains normal respiratory and cardiovascular function. Conscious sedation is defined as, “a minimally depressed level of consciousness that retains the patient’s ability to independently and continuously maintain an airway and respond appropriately to physical stimulation or verbal command and that is produced by a pharmacological or nonpharmacological method or a combination thereof.”2
|
Table 2. Required Monitoring and Emergency Equipment |
||||||||||
|
|
Table 3. Emergency Management for Anxiolysis |
||||||||
Note: The most important aspect of patient discharge is releasing the patient to a responsible companion. |
With regard to procedure protocol, there are more similarities than differences between anxiolysis and conscious sedation. For example: patient assessment, airway management, monitoring, record keeping, documentation, and the verbal skills are identical. Variations relate to the method of administering the anxiolytic drug, the dosages used, and when (if any) subsequent dosages are used. For anxiolysis, the drug(s) is (are) usually not dispensed in the office, but is prescribed in advance. The patient obtains the medication at the pharmacy and takes it as directed by the dentist.
|
Table 4. Preoperative and Postoperative Instructions |
|
Pre-op Post-op |
ANXIOLYTIC MEDICATIONS
Benzodiazepines have become the drug class of choice for sedation in dentistry. Compared with older medications such as barbiturates, they are safer, have a shorter duration, and provide a more clinically significant reduction in anxiety. What follows is a brief description of some of the drug options.
Diazepam
Diazepam (Valium) has a long history of safe and effective use as a sedative/hypnotic agent in dentistry. This benzodiazepine produces a mild level of sleep and amnesia, and has an onset after oral administration of about 1 hour. Diazepam is metabolized by the body into several active metabolites that may also cause sedation, a characteristic that accounts for diazepam’s half-life of 20 to 100 hours. This characteristic also makes diazepam an effective anxiolytic agent for pre-operative use the night before a dental procedure. Diazepam is supplied in 2, 5, and 10 mg tablets. The average dosage for an adult would be 5 to 10 mg.
Lorazepam
Lorazepam (Ativan), another benzodiazepine, can produce a higher level of hypnosis (defined as the ability to cause sleep) and amnesia than diazepam. The usual anxiolytic dosage is 2 to 3 mg. Its oral onset of action, like diazepam, is approximately 1 hour, although its half-life is 12 to 14 hours. Unlike diazepam, lorazepam has no active metabolites, and the effects last about 6 to 8 hours. It is available in 0.5, 1, or 2 mg tablets and, like all benzodiazepines, may be reversed with flumazenil. Precautions should be taken in elderly and debilitated patients, and those patients with impaired renal and hepatic function. Contraindications are: known hypersensitivity, pregnancy, children less than 12 years of age, and acute narrow angle glaucoma.4 Lorazepam is an FDA-approved anxiolytic.
Hydroxyzine
Hydroxyzine (Vistaril or Atarax) is an antihistamine with H1 antagonistic actions. It has bronchodilatory, antisialogogic, antiemetic, muscle relaxant, antiarrhythmic, and ataractic (having a tranquilizer effect) properties.5 Hydroxyzine is useful in reducing the dosage of narcotic and benzodiazepine requirements in preoperative sedation because of synergism. It can produce moderate levels of sleep without amnesia, and has one active metabolite. (The nonsedating anti-histamine Zyrtec [certirizine HCl] is an active metabolite of hydroxiyzine).6 Hydroxyzine has a rapid onset of action (15 minutes), a half-life of 3 to 7 hours, and duration of action of 4 to 6 hours. It is supplied in 10, 25, 50, and 100 mg caps, with an average dosage of 50 to 100 mg. It does not affect GABA receptors. While there is no specific antidote, antihistamine medications remain extremely safe with low incidence of adverse reactions.7 When hydroxyzine is administered concomitantly with another CNS depressant, precautions should be taken. Contraindications include early pregnancy, known hypersensitivity, nursing mothers, children under 1 year, and acute narrow angle glaucoma.7 Hydroxyzine is an FDA-approved anxiolytic.
Zaleplon
Zaleplon (Sonata), a newer generation anxiolytic, is most commonly prescribed for the short-term treatment of insomnia. It is in the pyrazolopyrimidine class, which is structurally different from benzodiazepines, yet it has been shown to affect the GABA receptor mechanism. Animal studies have shown the actions of zaleplon may be reversed with flumazenil, suggesting that this drug appears as a benzodiazepine to the body.8 It produces high levels of sleep, along with moderate levels of amnesia. Zaleplon has a relatively fast rate of onset, half-life, and duration of action (30 minutes, 1 hour, 1 to 2 hours respectively). It is supplied in 5 and 10 mg tabs, with the usual dose being 10 mg. Precautions should be taken with those patients who are elderly, have hepatic impairment, or are on other medications that affect its metabolism. The major pathway for zaleplon’s metabolism is the aldehyde oxidase system and the minor pathway is the cytochrome p450 system (specifically the 3A4 isoenzyme). It has no active metabolites. Zaleplon is contraindicated in children under 18 and in severely depressed patients.9
Triazolam
Triazolam (Halcion) has a long and well-documented record of safe and effective use as a sedative/hypnotic agent in dentistry. This benzodiazepine produces a high level of sleep and amnesia. Triazolam’s onset of action is within 1 hour, with a half-life of 2 to 5 hours, and a duration of action of 2 to 4 hours. Triazolam has been described as “near ideal anti-anxiety medication”10 for oral sedation in dentistry. Despite some past problems related to over-prescribing, it remains extremely safe and effective when used properly. It has not been shown to cause respiratory depression, even at higher than normal doses,11 and along with midazolam, another member of the benzodiazepine family, is described as a short half-life, high-potency benzodiazepine.
Midazolam
Midazolam (Versed), a short acting (1 hour) benzodiazepine, is capable of producing high levels of sleep and amnesia. It can be given orally either as a pre-mixed syrup or by injecting the medication into a liquid and swallowed. (Versed should not be delivered in grapefruit juice because of the potential interaction with the cytochrome p450 enzymes.13) Midazolam has a half-life of 1 to 3 hours, and has no active metabolites. The usual adult dose of oral midazolam is 10 to 15 mg, and for children the dose is 0.5 mg/kg.14,15 Like other benzodiazepines, midazolam effects GABA receptors, and can be reversed with flumazenil. Caution should be observed in combining midazolam with other CNS depressants. Contraindications include known hypersensitivity, acute narrow angle glaucoma, geriatric patients, and pregnant and nursing mothers.16
Nitrous Oxide (N2O)
Nitrous oxide (N2O), an inhalation anesthetic, is the oldest anxiolytic currently in use in dentistry. It is especially useful as a supplement to other anxiolytic agents. It can produce mild sleep, with a very rapid onset of action, usually within 3 minutes, and has no metabolites. The effects of N2O are dependent on length of administration and concentration used. Administration of N2O should always be followed by 100% oxygen flushing to prevent diffusion hypoxia. N2O is not metabolized within the body and is exhaled unchanged after the termination of administration. The effects of N2O can be completely reversed by 100% oxygen. N2O does not affect GABA receptors, and the usual adult dosage is 50% N2O(for children 20% to 30%). It does not produce amnesia. Caution should be observed in patients with chronic obstructive pulmonary disease or patients who are malnourished.17 Pregnancy is an absolute contraindication during the first trimester18 (N2O appears to impair B12 metabolism, which is involved in organogenesis during the first trimester19,20). N2O is an FDA-approved anxiolytic agent.
Additional Medications
There are many choices when selecting a drug regimen for either anxiolysis or conscious sedation. Some other drug classes that have been used for oral sedation are: narcotics, phenothiazines, barbiturates, alcohols, and anxiolytics.
ANXIOLYSIS PROTOCOLS
After determining that a patient is a candidate for oral sedation, the practitioner must decide on the medication(s) to be used. Each individual should refer to their state regulations on what medications can be used and how they should be administered. Typically, medications are administered in one of two ways to achieve anxiolysis. First, a medication can be given the night before to establish a blood level of the drug (and to help the patient rest comfortably), and another dose can be given 1 hour preoperatively. Or, a single oral dose may be given approximately 1 hour before the procedure is expected to begin. Alternatively, the determination of which protocol to use is a combination of several factors: state regulations, level of a patient’s anxiety, intended sedation level, type of dental procedures, and length of appointment.
ADJUSTMENTS TO PROTOCOL FOR THE SECOND APPOINTMENT
Dosage adjustments may need to be made for subsequent appointments based on the anxiolysis experience of the first visit. A positive experience for the patient is one in which the patient achieved a level of relaxation where they could receive treatment with little or no discomfort. A typical response on a postoperative interview is, “I was so relaxed in the chair that I think I dozed off for much of the appointment.” A positive experience for the office is one in which the patient was sufficiently relaxed so the dental team could perform the planned procedures in a timely and effective manner.
PRESCRIPTION EXAMPLES
Figures 2 through 5 are examples of how prescriptions for anxiolytic medications could be written. Dosages would be adjusted according to the individual patient’s needs.
TRAINING
Training courses on enteral sedation are available from several sources. Check with your CE providers to determine if they provide training in anxiolysis.
CONCLUSION
Anxiolysis, when administered properly by a trained general practitioner, can prove to be a safe and effective method of providing dental care to fearful patients. Unlike the incremental conscious sedation, no additional permit is required by state or provincial regulatory agencies. Dental anxiety has been shown to be one of the biggest obstacles for patients seeking needed care.23 The technique of anxiolysis has proven helpful to providers and patients in overcoming this obstacle and achieving oral health.
References
- Newman Dorland WA, Anderson DM. Dorland’s Illustrated Medical Dictionary. 29th ed. Philadelphia, Pa: WB Saunders; 2000:109.
- ADA guidelines for the use of conscious sedation, deep sedation, and general anesthesia for dentists. Available at: www.ada.org/prof/ed/guidelines/cs-guide.html. Accessed on: Nov. 1, 2002.
- Physician’s Desk Reference. 56th ed. Montvalle, NJ: Medical Economics Co; 2002:3047-3048.
- Physician’s Desk Reference. 56th ed. Montvalle, NJ: Medical Economics Co; 2002:3482-3483.
- Hardman JG, Limbird LE, Gilman AF. Goodman & Gilman’s: The Pharmacological Basis of Therapeutics. 10th ed. New York, NY: McGraw-Hill Publishing; 2001:651-657.
- Einarson A, Bailey B, Jung G, et al. Prospective controlled study of hydroxyzine and certirizine in pregnancy. Ann Allergy Asthma Immunol. 1997;78:183-186.
- Physician’s Desk Reference. 56th ed. Montvalle, NJ: Medical Economics Co; 2002:2738-2739.
- Heydorn WE. Zaleplon: a review of a novel sedative hypnotic used in the treatment of insomnia. Expert Opin Investig Drugs. 2000;9:841-858.
- Physician’s Desk Reference. 56th ed. Montvalle, NJ: Medical Economics Co; 2002:3591-3595.
- Dionne RA., Phero JC, Becker DE. Management of Pain and Anxiety in the Dental Office. Philadelphia, Pa: W.B. Saunders; 2002:229.
- Skarud JB, Begle RL, Busch MA. Ventilatory effects of single, high-dose triazolam in awake human subjects. Clin Pharmacol Ther. 1988;44:684-689.
- Physician’s Desk Reference. 56th ed. Montvalle, NJ: Medical Economics Co; 2002:2823-2835.
- Goho C. Oral midazolam: grapefruit juice drug interaction. Pediatric Dent. 2001;23:365.
- Wilson S. Pharmacologic behavior management for pediatric dental trea








