INTRODUCTION
Amelogenesis imperfecta is a collection of genetic conditions that most often presents intraorally with generalized hypomineralization. Treatment requires a multidisciplinary approach and close professional collaboration. Although treatment methods vary, most patients initially require anterior composite restorations and posterior stainless steel crowns on high-risk teeth to allow for healthy psychosocial development and posterior function. Following growth and development, patients often require full-arch restorations in conjunction with crown lengthening surgery since hypomineralization and wear minimize available tooth structure. This case report documents the multidisciplinary treatment of a patient suffering from amelogenesis imperfecta and highlights the significance of interdisciplinary collaboration.
Amelogenesis imperfecta is an uncommon genetic condition affecting the enamel. More specifically, it causes hypomineralization or hypoplasia.1 Epidemiologically, the disease prevalence ranges from 1:700 to 1:14,000.2,3 The different classifications of the disease are organized either by clinical presentation or genetic mutation. Alterations to the secretory stage of tooth development can cause amelogenesis imperfecta via mutations in AMELX (X-linked) or ENAM (autosomal dominant) genes. Likewise, mutations in MMP20 and LKL4 genes (autosomal recessive) result in softer enamel.4 Amelogenesis imperfecta affects enamel of all teeth, and hypoplasia is often associated with discoloration and hypersensitivity.1 Treatment of these patients is very challenging since restorations are required on every tooth. Moreover, the quality of the existing tooth structure can complicate the quality of final restorations as inadequate etching can result in less retention and more leakage. Coronal restorations in patients with amelogenesis imperfecta had a survival rate of 50% compared to a survival rate of 80% in patients with normal enamel.5 A conservative treatment option may include direct resin restorations, but this choice may only be a transitional treatment until patients finish growth.6 More often, full-coverage restorations are necessary for proper restoration and can be metal, stainless steel, ceramic, or porcelain-fused-to-metal.7 Full-coverage restorations in patients with amelogenesis imperfecta are predictable and comparable to full-coverage restorations placed in healthy patients.5 Because of the wear, most full-mouth cases require crown lengthening surgery in order to provide adequate tooth structure.8 Restoring and treating patients with amelogenesis imperfecta is a complicated task that requires an interdisciplinary approach and a comprehensive plan.
CASE REPORT
A 16-year-old healthy male presented to the Rutgers School of Dental Medicine with the following chief complaint: “I have a lot of sensitivity, and I want to fix my smile.” The patient was diagnosed with amelogenesis imperfecta during childhood and received composite restorations in the anterior teeth and stainless steel crowns on the permanent first molar teeth as a provisional means to restore the dentition prior to completion of growth.6 The patient had a history of irregular care over the last several years. His mother stated that her 16-year-old son was reluctant to smile, particularly around his peers in school. The clinical examination revealed defective enamel with dentin exposure, yellow discoloration, tooth sensitivity, and dental caries (Figures 1 to 3). The premolar teeth had short clinical crowns and radiographically revealed large pulp horns. The maxillary and mandibular second molars were covered partially with keratinized mucosa, indicating that passive eruption may not yet have been completed. The maxillary right second molar was completely covered by soft tissue and was radiographically shown to have coronal tooth resorption, called intracoronal resorption. The maxillary arch was oval in shape and exhibited slight constrictions, particularly in the premolar regions. Occlusal examination showed that there was a slight discrepancy between centric relation and maximum intercuspal position with posterior teeth interferences in all excursive movements. Due to the extent of the enamel defects, there was occlusal attrition of the premolars. This led to supra-eruption of the premolar teeth and maxillary canines, causing a reverse smile-line and large gingival display in the maxillary premolar region on the full smile. Although he presented with generalized occlusal attrition, there was no loss of vertical dimension due to the compensatory dentoalveolar movement of the premolar teeth and the presence of stainless steel crowns on the first molar teeth. Radiographically, the coronal portions of the teeth appeared to have a thin layer of enamel, a typical phenomenon of hypoplastic amelogenesis imperfecta. Bite-wing and periapical radiographic films indicated that the pulp horns of the mandibular premolars were close to the external occlusal surfaces of the teeth (Figure 4). Based on the clinical and radiographic findings, a diagnosis of amelogenesis imperfecta was made. This is associated with a thin or no enamel layer (hypoplastic teeth), dental caries, defective composite restorations, occlusal plane discrepancy, occlusal interferences, and unerupted third molar teeth. The patient was treatment planned for a full-mouth rehabilitation with full-coverage restorations. The goals of treatment were to protect the teeth, reduce teeth sensitivity, and restore normal tooth form, function, and aesthetics. The prognosis for the teeth was favorable except for the maxillary right second molar, which was planned for extraction. No implant was planned at this stage since there were occlusal contacts between teeth Nos. 3 and 31, which will maintain the tooth spatial position of tooth No. 31. However, the patient was informed to replace the missing tooth in the future if needed. Because involving third molars in the treatment would complicate the case, the decision was made to extract them at the early stage of the treatment even though they were not yet erupted.

Figure 1. Preoperative frontal view. The patient presented with anterior composite restorations, generalized hypoplasticity, and posterior stainless steel crowns.

Figure 2. Pre-op occlusal view of the maxillary arch.

Figure 3. Pre-op occlusal view of the mandibular arch.
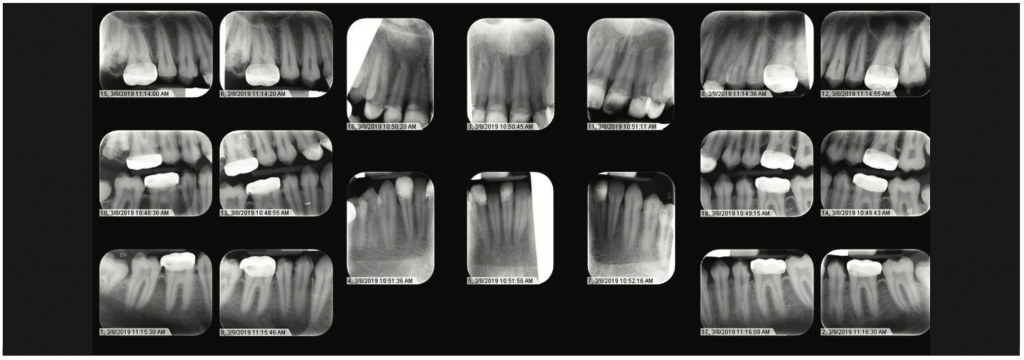
Figure 4. Full-mouth series illustrating extensive mineralization defects.
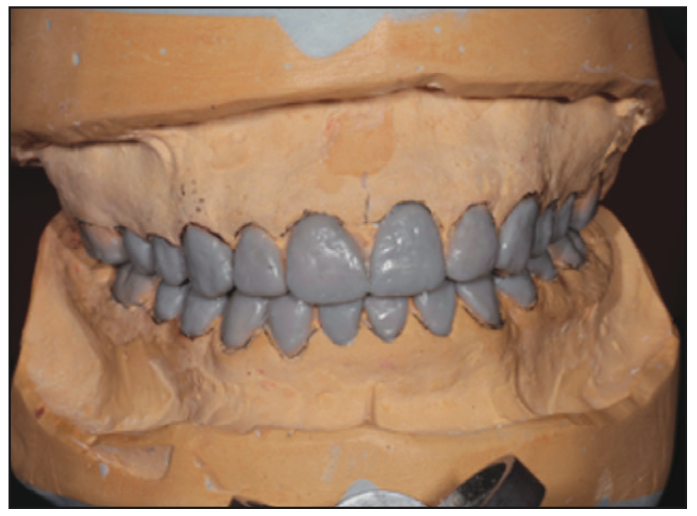
Figure 5. Mounting and wax-up at increased vertical dimension, which was necessary due to extensive wear.

Figure 6. Frontal view of provisional restorations at increased vertical dimension with polymethylmethacrylate.

Figure 7. Occlusal view of the full-arch mandibular temporary prosthesis with composite on second molars to hold the vertical position of the teeth.

Figure 8. Crown lengthening was performed for maxillary and mandibular posterior teeth. Pre-op photograph of the right posterior sextant.
In order to ensure proper delivery of care, an interdisciplinary approach, including prosthetic and periodontal collaboration, was required. Prior to treatment planning, irreversible hydrocolloid impressions (Jeltrate [Dentsply Sirona]) of the maxillary and mandibular arches were made to generate diagnostic stone casts. These casts were mounted in centric relation with a face-bow transfer on a semi-adjustable articulator (Hanau Wide Vue [Whip Mix]). A diagnostic wax-up was then constructed. Since the teeth exhibited large pulp horns, a conservative approach was made to open the vertical dimension by 2 mm in the premolar area and select a restorative material that would accept a minimum occlusal thickness yet restore aesthetics and function. In this case, all-ceramic lithium disilicate material was selected for the anterior and posterior teeth. Full-metal gold restorations were planned for restoration of the second molar teeth to the required restorative space. The first phase of the treatment involved caries control and the extraction of the third molars and the maxillary right second molar. This improved accessibility to the distal surfaces of the second molars. Initially, all teeth were prepared except for the second molars. The patient was provisionalized in the new vertical dimension of occlusion with full-arch splinted fixed temporaries made of milled PMMA resin material relined with chairside auto-polymerized resin material (ALIKE Temporary Crown and Bridge Resin [GC America]) (Figures 5 and 6). Flowable composite (Filtek Supreme Flowable Restorative [3M]) was added to the occlusal pit and fissure of the mandibular second molars to maintain the vertical position of these teeth until the crown lengthening was done, and these teeth were prepared to receive provisional crowns (Figure 7). The provisional restorations and increased vertical dimension were tested for 4 weeks. During this time, there were no TMD symptoms or difficulty in speech or swallowing reported by the patient. After confirming the patient’s comfort, he was seen in the postgraduate periodontics department for crown lengthening of the maxillary arch and mandibular posterior teeth. Prior to crown lengthening, surgical guides were fabricated on models depicting the desired level for the soft tissue. With the aid of the surgical guide, crown lengthening was completed to ensure proper space for biologic width and adequate retention and resistance form (Figure 8). The crown lengthening procedure entailed a full-thickness flap elevated to the mucogingival junction and a split-thickness flap apical to the mucogingival junction (Figure 9). This allowed precise apical repositioning of the flap at the crest following ostectomy and osteoplasty via 4-0 chromic gut sutures (FS2 Ethicon). Also, the amount of keratinized gingiva was maintained (Figure 10). Immediately after crown lengthening and before the flap was sutured, the second molar teeth were prepared, and the temporary crowns were fabricated to ensure the desired preparation design was achieved. After appropriate healing (Figure 11), the finish line margins of the teeth preparations were refined, and the patient received a second set of provisionals to ensure proper aesthetics and function (Figure 12). Prior to final impressions, the patient requested the treatment of pigmented gingiva, which was accomplished by using the Nd:YAG laser (PerioLase MVP-7 [Millennium Dental Technologies]). Maxillary and mandibular frenectomies were performed at the same time (Figure 13). The Nd:YAG laser has a 1,064-nm wavelength, which highly absorbs melanin and pigment, optimizing the depigmentation process.
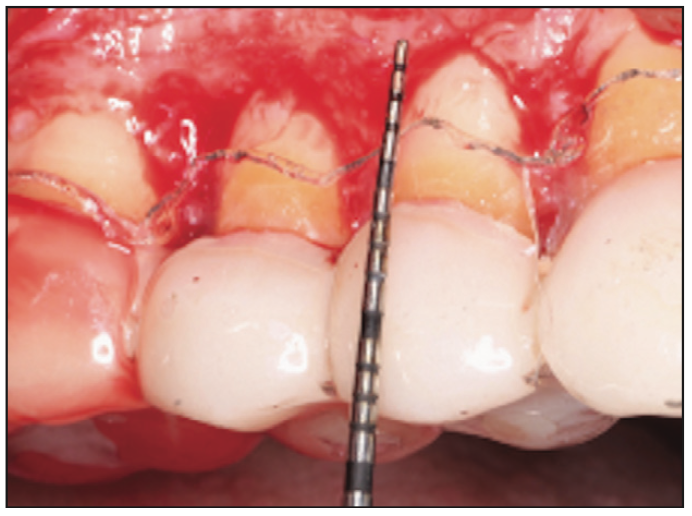
Figure 9. Intraoperative photograph illustrating full-/split-flap elevation and osseous recontouring with a surgical guide to allow for biologic width.

Figure 10. Immediate postoperative photograph of an apically positioned flap following the crown lengthening procedure.

Figure 11. Post-op photograph of one sextant of the crown lengthening procedure.

Figure 12. Post-op photograph after relining provisional restorations.

Figure 13. Intraoperative photograph illustrating the use of an Nd:YAG laser for maxillary and mandibular depigmentation and frenectomies.
RESULTS

Figure 14. Post-op photograph illustrating the result of the depigmentation and frenectomy procedure.
Following healing, the patient was pleased with the aesthetic result (Figure 14). Four months after crown-lengthening surgery and laser therapy, intrasulcular preparations were impressed for delivery of the final prosthetics (Figures 15 to 19). The patient reported the disappearance of teeth sensitivity at the end of the treatment and during followup visits. Moreover, the patient received an aesthetic and functional result (Figures 20 to 22) that restored his functionality and psychosocial health as compared to his initial presentation. Regular maintenance is very crucial for long-term successful treatment. Therefore, he is being placed on a meticulous maintenance schedule of every 3 to 4 months. Oral hygiene has been continually reinforced, and the patient has been placed on PreviDent 5000 (Colgate) and Booster Toothpaste (Colgate).

Figure 15. Frontal view following final delivery of the all-ceramic lithium disilicate restorations.

Figure 16. Right lateral view following final delivery of the all-ceramic lithium disilicate restorations.

Figure 17. Left lateral view following final delivery of the all-ceramic lithium disilicate restorations.

Figure 18. Maxillary occlusal view following final delivery of the all-ceramic lithium disilicate restorations and full-coverage gold restoration of the second molar.

Figure 19. Mandibular occlusal view following final delivery of the all-ceramic lithium disilicate restorations and full-coverage gold restoration of the second molars.
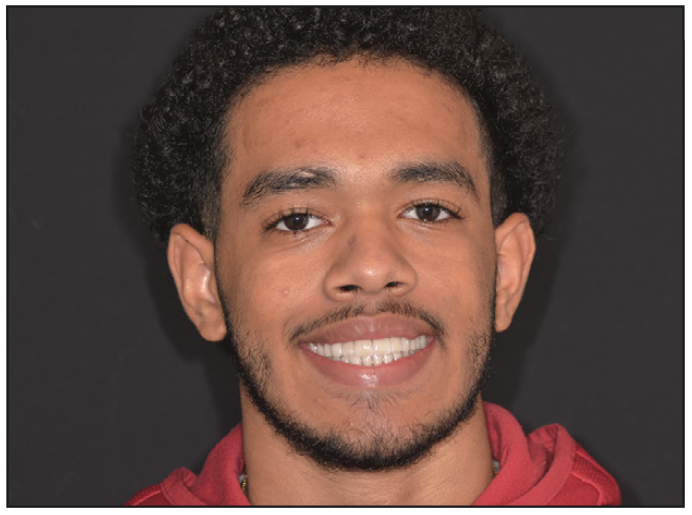
Figure 20. Frontal extraoral photograph of smile following interdisciplinary therapy and full-mouth rehabilitation.

Figure 21. Lateral extraoral photograph at rest following interdisciplinary therapy and full-mouth rehabilitation.

Figure 22. Lateral extraoral photograph of smile following interdisciplinary therapy and full-mouth rehabilitation.
DISCUSSION
Management of these patients is accomplished in 3 phases: temporary, transitional, and permanent.9 The temporary phase of care addresses the primary and mixed dentition, which requires a combination of composite restorations for aesthetic concerns and stainless steel posterior restorations. The transitional phase entails monitoring the patient’s growth and restorative status until the permanent dentition has completed eruption and the patient has ceased active growth. At this time, the patient enters the permanent phase, where a multidisciplinary team provides full-mouth rehabilitation. This case report illustrates the prosthetic and periodontal treatment of a patient entering the permanent phase of care. As Chen et al9 discuss, the patient was properly diagnosed at an early age when he received stainless steel posterior crowns to prevent caries progression and composite anterior restorations. Note that the direct anterior restorations were delivered primarily to improve psychosocial status. Studies regarding amelogenesis imperfecta patients indicate that without aesthetic restorations, their self-esteem decreases, and social dysfunction increases.10 Both indirect and direct restorations have been reported to restore teeth in patients with amelogenesis imperfecta. While guidelines to treat such patients are not yet available, indirect restorations have shown more predictable results when compared to direct restorations.11 Previous research showed that the enamel and dentin in patients with amelogenesis imperfecta are associated with changed properties, which explains why direct restorations have a higher failure rate than indirect restorations. All-ceramic lithium disilicate material was chosen to restore the majority of the teeth in this case. Not only does lithium disilicate material provide excellent optical properties, but it also allows for minimal tooth preparation and possesses acceptable strength and longevity when bonded to tooth structure. Previous reports showed that all-metal, full-gold material would be the material of choice when restoring second molar teeth because of the minimal thickness needed and high fracture strength.
To ensure high longevity of the restorations, retentive grooves were added to the teeth preparations to improve the retention and resistance form. Although the patient presented with limited interocclusal space distance (2 mm), the vertical dimension of occlusion was opened by 1.5 mm, and another 0.5 mm was achieved by guiding the patient to CR position. Such an increase has been reported to be safely introduced when certain considerations are taken.12,13 In addition, the temporary crowns were tested in the patient’s mouth for several months without any signs and symptoms reported by the patient.
One of the main advantages of opening the VDO in such cases is to provide a space for restorative material so that minimum occlusal reduction is needed. This is important since the pulp horns of the mandibular premolars appeared close to the occlusal surfaces due to the patient’s age and the thin enamel layer. Other advantages include maintaining tooth vitality, preserving tooth structure, reducing the amount of adjunctive surgery, and correcting minor irregularities in the occlusal plane.12 Special attention was paid to the thickness of the existing enamel on the tooth surfaces during the examination process. Since there was limited thickness evident clinically, the wax-up was done using an additive approach. Consequently, minimal reduction of the axial walls was needed during tooth preparation.
Growth of the jawbone vertically and horizontally may initiate some spaces between the teeth. However, migration of the teeth should maintain biological and functional contacts. Moreover, with proper margin placement and good restorative material selection, future apical migration of the gingiva in the aesthetic zone should present as a minimal aesthetic concern. Finally, the patient avoided endodontic therapy even though the prevalence of endodontic complications reported ranges between 1% to 3% in patients with amelogenesis imperfecta.14,15 Orthodontic intervention is common due to malocclusion, open bites, delayed tooth eruption, missing teeth, and pathological crown and root formation.9,16 Orthodontic treatment was presented to the patient, and he declined due to the time and cost of the treatment. Since he presented with mild orthodontic issues, the case was successfully managed with proper planning and meticulous periodontal and restorative treatment.
CONCLUSION
This case report discusses one example of amelogenesis imperfecta management. Proper care for patients with this condition is often accomplished in 3 phases, with the final phase requiring full-mouth rehabilitation. This publication highlights the need for interprofessional collaboration and illustrates various challenges that may occur during treatment. It further illustrates the positive impact proper treatment can have on a patient’s social, functional, and aesthetic well-being.
ACKNOWLEDGMENTS
A special thank you to Dr. Neal Lehrman for his guidance with the laser depigmentation therapy. The case was delivered through the Rutgers School of Dentistry Postgraduate Program and made possible with the associated faculty and staff.
REFERENCES
1. Crawford PJ, Aldred M, Bloch-Zupan A. Amelogenesis imperfecta. Orphanet J Rare Dis. 2007;2:17. doi:10.1186/1750-1172-2-17
2. Bäckman B, Holm AK. Amelogenesis imperfecta: prevalence and incidence in a northern Swedish county. Community Dent Oral Epidemiol. 1986;14(1):43-7. doi:10.1111/j.1600-0528.1986.tb01493.x
3. Witkop CJ, Sauk JJ. Heritable defects of enamel. In: Stewart RE, Prescott GH (Eds.), Oral facial genetics. Mosby;1976:151-226.
4. Hu JC, Chun YH, Al Hazzazzi T, et al. Enamel formation and amelogenesis imperfecta. Cells Tissues Organs. 2007;186(1):78-85. doi:10.1159/000102683
5. Pousette Lundgren G, Dahllöf G. Outcome of restorative treatment in young patients with amelogenesis imperfecta. A cross-sectional, retrospective study. J Dent. 2014;42(11):1382–9. doi:10.1016/j.jdent.2014.07.017. Erratum in: J Dent. 2015;43(2):295.
6. Sabatini C, Guzmán-Armstrong S. A conservative treatment for amelogenesis imperfecta with direct resin composite restorations: a case report. J Esthet Restor Dent. 2009;21(3):161–9; discussion 170. doi:10.1111/j.1708-8240.2009.00258.x
7. Sabandal MM, Schäfer E. Amelogenesis imperfecta: review of diagnostic findings and treatment concepts. Odontology. 2016;104(3):245–56. doi:10.1007/s10266-016-0266-1
8. Akin H, Tasveren S, Yeler DY. Interdisciplinary approach to treating a patient with amelogenesis imperfecta: a clinical report. J Esthet Restor Dent. 2007;19(3):131–5; discussion 136. doi:10.1111/j.1708-8240.2007.00083.x
9. Chen CF, Hu JC, Bresciani E, et al. Treatment considerations for patient with Amelogenesis Imperfecta: a review. Braz Dent Sci. 2013;16(4):7-18. doi:10.14295/bds.2013.v16i4.904
10. Coffield KD, Phillips C, Brady M, et al. The psychosocial impact of developmental dental defects in people with hereditary amelogenesis imperfecta. J Am Dent Assoc. 2005;136(5):620–30. doi:10.14219/jada.archive.2005.0233
11. Strauch S, Hahnel S. Restorative treatment in patients with amelogenesis imperfecta: a review. J Prosthodont. 2018;27(7):618–23. doi:10.1111/jopr.12736
12. Abduo J. Safety of increasing vertical dimension of occlusion: a systematic review. Quintessence Int. 2012;43(5):369–80.
13. Fabbri G, Sorrentino R, Cannistraro G, et al. Increasing the vertical dimension of occlusion: a multicenter retrospective clinical comparative study on 100 patients with fixed tooth-supported, mixed, and implant-supported full-arch rehabilitations. Int J Periodontics Restorative Dent. 2018;38(3):323–35. doi:10.11607/prd.3295
14. Lindunger A, Smedberg JI. A retrospective study of the prosthodontic management of patients with amelogenesis imperfecta. Int J Prosthodont. 2005;18(3):189–94.
15. Pousette Lundgren G, Morling Vestlund GI, Trulsson M, et al. A randomized controlled trial of crown therapy in young individuals with amelogenesis imperfecta. J Dent Res. 2015;94(8):1041–7. doi:10.1177/0022034515584385
16. Arkutu N, Gadhia K, McDonald S, et al. Amelogenesis imperfecta: the orthodontic perspective. Br Dent J. 2012;212(10):485–9. doi:10.1038/sj.bdj.2012.415
ABOUT THE AUTHORS
Dr. Murayshed received his BDS degree from the King Saud University College of Dentistry, Riyadh, Saudi Arabia, in 2012. In 2021, he received his postgraduate specialty certificate in prosthodontics and earned a Master of Dental Sciences degree from the Rutgers School of Dental Medicine (RSDM). Currently, Dr. Murayshed is working as faculty in prosthetic dental sciences at Prince Sattam bin Abdulaziz University in Saudi Arabia. He can be reached at drmohammad1@hotmail.com.
Dr. Goldberg is a periodontist working in private practice in New Jersey. He received his DDS degree from Columbia University in 2018 and completed his periodontal residency at Rutgers University in 2021. During his postgraduate tenure, Dr. Goldberg presented at and moderated the Northeastern Implant Symposium, served as chief resident, received a degree from the Institute of Advanced Laser Dentistry, and was awarded the Michael J. Deasy Endowed Scholarship. He currently practices with his father, who is also an established periodontist. He can be reached at adamgoldberg2207@gmail.com.
Dr. Howard Drew is a professor, a director of implantology, and the vice chairman of the Department of Periodontics at RSDM. He received his doctorate and degree in periodontics from RSDM. He has been awarded the RSDM Excellence in Teaching Award, Stuart D. Cook Master Educators Guild Award, and the prestigious AAP Educator Award. Dr. Drew was inducted into the American College of Dentists, and he was awarded the RSDM Alumni Association Decade (1980s) Award. He has more than 25 publications to his name and has lectured throughout the country. He was in full-time clinical practice for more than 25 years. He can be reached at drhjdrew@aol.com.
Dr. Alexander Drew is a maxillofacial prosthodontist with a private practice in Summit, NJ, limited to prosthodontics and restorative dentistry. He received his DMD degree from the University of Pennsylvania. After completing dental school, he earned a specialty certificate in prosthodontics and an MS degree from the Columbia University College of Dental Medicine, where he was the chief resident. He then completed a subspecialty fellowship in maxillofacial prosthetics and was awarded a certificate from Memorial Sloan Kettering Cancer Center. Dr. Drew is a member of the American College of Prosthodontics and the ADA. He is an Associate Fellow of the American Academy of Maxillofacial Prosthetics and an author to research publications in high-impact scientific journals. He can be reached at asdrew1@gmail.com.
Disclosure: The authors report no disclosures.











