INTRODUCTION
In 2023, dental caries is still the most common oral disease in children.1 Not only does this condition affect children’s oral wellness, but it also lowers their self-esteem. This is especially true when dental caries are on the front teeth and easily noticed. The traditional approach is to treat these cases at a more advanced stage of decay. The material of choice was stainless steel crowns, then later tooth-color zirconia crowns. Both children and parents are asking for more natural aesthetics and less invasive treatment instead of amalgam restorations, zirconia, and stainless steel crowns for primary anterior teeth.2
The good news is that the shift to a much more conservative treatment model is here and has been growing since the 1990s. In addition to treating the caries, our focus is more on early caries detection, nutrition and hydration, risk assessment, and airway evaluation. We also have dental materials like flowable composites with improved filler technology and digital dental technology such as intraoral digital scanners, digital design software, and even AI to restore the teeth and fulfill the 3 basic requirements of function, aesthetics, and biocompatibility.3
Recently, VOCO released Admira Fusion Flow, the first-of-its-kind, purely ceramic-based flowable restoration material with no classic monomers. Thanks to the incredibly innovative Nano-ORMOCER technology, the flowable composite has extremely low polymerization shrinkage (2.75% by volume) and particularly low levels of shrinkage stress in comparison to conventional flowable composites. This material achieves a great result thanks to its filler content and excellent surface affinity with complete wetting of the cavity wall. It is very biocompatible and highly resistant to discoloration, which is perfect for pediatric anterior restorations.4
Admira Fusion Flow is known for “flow on demand” because the material becomes flowable only when under pressure or in motion. It has excellent handling characteristics; polishes to a high luster; and, when coupled with high surface hardness, guarantees first-class long-term results.5,6 This works very well for the flowable composite injectable technique, which is simple and efficient, especially for pediatric cases like the ones below.7
CASE REPORTS
Case 1
The patient presented at 4 years old with SDF placed to arrest all 6 maxillary anterior teeth (Figure 1). A comprehensive exam, including risk assessment, nutrition, hydration, and airway evaluation, was completed with an intraoral scan (3Shape TRIOS scanner [3Shape]). The dental lab (Esthetics Dental Studio, Cypress, Texas) completed the digital wax-up and fabricated a matrix with a clear PVS material (EXACLEAR [GC]) (Figure 2). The cavity preps were selectively etched with 32% semi-gel phosphoric acid etchant with benzalkonium chloride (BAC) (Uni-etch [BISCO]) for 10 seconds and rinsed with water for 30 seconds, and the enamel was dried with a warm air tooth dryer (A-dec). Admira Bond (VOCO) was placed as the adhesive, thinned with the warm air tooth dryer, and light-cured for 10 seconds with an LED curing light (VALO [Ultradent Products]). Creative Color Pink Opaque (Cosmedent) was applied in 1.0-mm layers to block out the discoloration and light-cured for 10 seconds (Figure 3).

Figure 1. Preoperative view of the maxillary primary incisors and canines of a 4-year-old patient with extensive caries arrested with SDF.
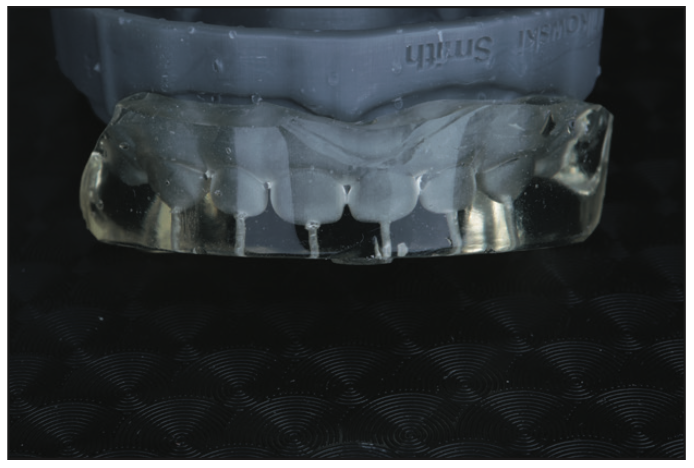
Figure 2. A clear PVS matrix was fabricated to replicate the digital wax-up intraorally.

Figure 3. Existing discoloration blocked out with Creative Color Pink Opaque (Cosmedent).

Figure 4. Immediately after the clear matrix was removed.
A clear PVS matrix was placed after Teflon tape was used to cover the primary premolars. Admira Fusion Flow was injected using the matrix and was light-cured for 10 seconds with an LED curing light. The clear PVS matrix was then removed (Figure 4). The composite was contoured and shaped with an OS1 carbide finishing bur (Brasseler USA). The last step included placing a clear resin coat of varnish (Dreve [anax USA]) over the entire restoration with a microbrush and then light curing for 10 seconds. The oxygen-inhibiting layer was removed by applying DeOx (Ultradent Products) and then light-cured for 10 seconds and rinsed with water for 30 seconds. The final restoration (Figure 5) demonstrates the natural effect of the material with a final finish and high gloss.

Figure 5. The completed maxillary primary restorations.

Figure 6. Retracted view at 18 months postoperative.

Figure 7. Smile view at 18 months post-op.

Figure 8. Retracted view at 30 months post-op.

Figure 9. Smile view at 30 months post-op.

Figure 10. Retracted view at 36 months post-op.

Figure 11. Smile view at 36 months post-op.
The patient came back for followup at 18 months (Figures 6 and 7), again at 30 months (Figures 8 and 9), and at 36 months (Figures 10 and 11).
Case 2
The mother of a 3-year-old patient had concerns about his worn primary dentition, especially the anterior (Figure 12). A comprehensive exam, including dental caries risk assessment, nutrition, hydration, tongue posture, and airway evaluation, was completed with an intraoral scan (TRIOS scanner). The patient was given oral myofunctional exercises to practice at home, nasal hygiene instruction to enhance nasal breathing, and mouth taping at night. The dental lab (Esthetics Dental Studio) completed the digital wax-up and fabricated the clear matrix with clear PVS (EXACLEAR). The teeth were selectively etched with 32% semi-gel phosphoric acid etchant with BAC (Uni-etch) for 10 seconds and rinsed with water for 30 seconds, and the enamel was dried with a warm air tooth dryer (A-dec). Admira Bond was placed as the adhesive, thinned with the warm air tooth dryer, and light-cured for 10 seconds with an LED curing light (VALO). Creative Color Pink Opaque was applied in 1.0-mm layers to block out the discoloration and light-cured for 10 seconds. A clear PVS matrix was placed after Teflon tape was used to cover the primary canines. Admira Fusion Flow was injected using the matrix and was light-cured for 10 seconds with an LED curing light, and the clear PVS matrix was removed. The composite was contoured and shaped with an OS1 carbide finishing bur (Brasseler USA). The last step included placing a clear resin coat of varnish (Dreve) over the entire restoration with a microbrush, which was light-cured for 8 seconds. The oxygen-inhibiting layer was removed by applying DeOx, light-cured for 10 seconds, and then rinsed with water for 30 seconds. The final restoration (Figure 13) demonstrates the natural effect of the material and the final finish and high gloss.

Figure 12. Before the composite bonding.

Figure 13. After the composite bonding on teeth D to G.
CLOSING COMMENTS
With the advancement of biocompatible flowable composites, clinicians now have choices when treating pediatric patients with primary caries in the anterior restorations to obtain function, aesthetics, and biocompatibility. This will help patients to keep healthy teeth and confident smiles. The injectable technique with flowable composite is predictable, efficient, and minimally invasive, which means happier pediatric dental patients and parents.
REFERENCES
1. Beltrán-Aguilar ED, Barker LK, Canto MT, et al; Centers for Disease Control and Prevention (CDC). Surveillance for dental caries, dental sealants, tooth retention, edentulism, and enamel fluorosis—United States, 1988-1994 and 1999-2002. MMWR Surveill Summ. 2005 Aug 26;54(3):1-43.
2. Hyson JM Jr. Amalgam: Its history and perils. J Calif Dent Assoc. 2006;34(3):215–29.
3. Terry DA. Direct applications of a nanocomposite resin system: Part 1—The evolution of contemporary composite materials. Pract Proced Aesthet Dent. 2004 Jul;16(6):417–22.
4. Jefferies SR. The art and science of abrasive finishing and polishing in restorative dentistry. Dent Clin North Am. 1998;42(4):613–27.
5. Hervás-García A, Martínez-Lozano MA, Cabanes-Vila J, et al. Composite resins. A review of the materials and clinical indications. Med Oral Patol Oral Cir Bucal. 2006;11(2):E215-20. English, Spanish.
6. Hosoya Y, Shiraishi T, Oshiro M, et al. Color characteristics of resin composites in different color modes and geometries. J Oral Sci. 2009;51(1):123–30. doi:10.2334/josnusd.51.123
7. Terry DA, Powers JM, Mehta D, et al. A predictable resin composite injection technique, part 2. Dent Today. 2014;33(8):12.
ABOUT THE AUTHOR
Dr. To graduated from the University of Texas Health Science Center in San Antonio in 2010 with distinction in research. She is the founder of Katie To Center of Integrative Wellness and Cosmetic Dentistry, KT Dental Seminars, and the Wellness Dentist Institute. She has maintained a private practice in Katy, Texas, since 2015, emphasizing cosmetic and wellness dentistry. She can be reached at (281) 392-8450, via email at drkatie@thewellnessdentist.com, or at the website thewellnessdentist.com.
Disclosure: Dr. To has no financial interest in any of the companies mentioned in this article but did receive compensation from VOCO for writing this article.











