INTRODUCTION
Gingival harmony plays a key role in an aesthetic smile.1 Altered passive eruption (APE) can adversely affect gingival architecture due to the failure of the soft tissue to recede apically to the cervical convexity of the tooth.2 APE is also one of the leading causes of gingival excess,3 or “gummy smile,”4,5 where the patient exposes more than 3 to 4 mm of continuous gingiva upon a full smile. This presents a plethora of clinical challenges, including short clinical crowns, disproportionate interproximal papilla,6 uneven and asymmetric gingival margin positions,7 and invasion of biologic width.5
Coslet et al8 categorize APE into 4 different types, according to the width of gingiva and the relationship between the cemento-enamel junction (CEJ) and alveolar crest (AC). It was found that Type 1B with a wide band of gingiva and CEJ coincident with AC was the most common.3 The recommended treatment for APE Type 1B is aesthetic crown lengthening, which includes an inverse bevel gingivectomy followed by surgical crown lengthening with ostectomy and osteoplasty.
There have been several different approaches to aesthetic crown lengthening, including the use of a proportion gauge9 and fabrication of a clear matrix based on a diagnostic wax-up. The advent of intraoral scanners and planning software has allowed for a digital approach to aesthetic crown lengthening. The following clinical case incorporates digital smile design software, a digital wax-up, and 3D printing in combination with a multi-tissue laser to deliver an efficient and predictable clinical outcome for a patient undergoing aesthetic crown lengthening.
CASE REPORT
A 21-year-old female patient with a nonsignificant medical history presented to our practice with a chief complaint of “short and discolored teeth.” The patient demonstrated congenital enamel hypoplasia resulting in discoloration and cold sensitivity (Figure 1).

Figure 1. Preoperative, full-smile photo of the patient.
She was looking to improve the aesthetics of her smile with fixed restorations. Comprehensive examination revealed a high smile line and short clinical crowns without any signs of wear as well as uneven gingival margins and deficient interproximal papillae between maxillary laterals and canines. The patient was diagnosed as having APE Type 1B per Coslet classification.5
Digital Smile Design
A series of extraoral photos was taken for 2D digital smile design, and 2 different versions were created: one without aesthetic crown lengthening and another with aesthetic crown lengthening (Figures 2 and 3). This was a powerful motivational tool for the patient to preview 2 different clinical outcomes without having to undergo a traditional diagnostic wax-up and an intraoral mockup.10 The patient elected to complete the restorative work with aesthetic crown lengthening to achieve the most optimal clinical outcome.
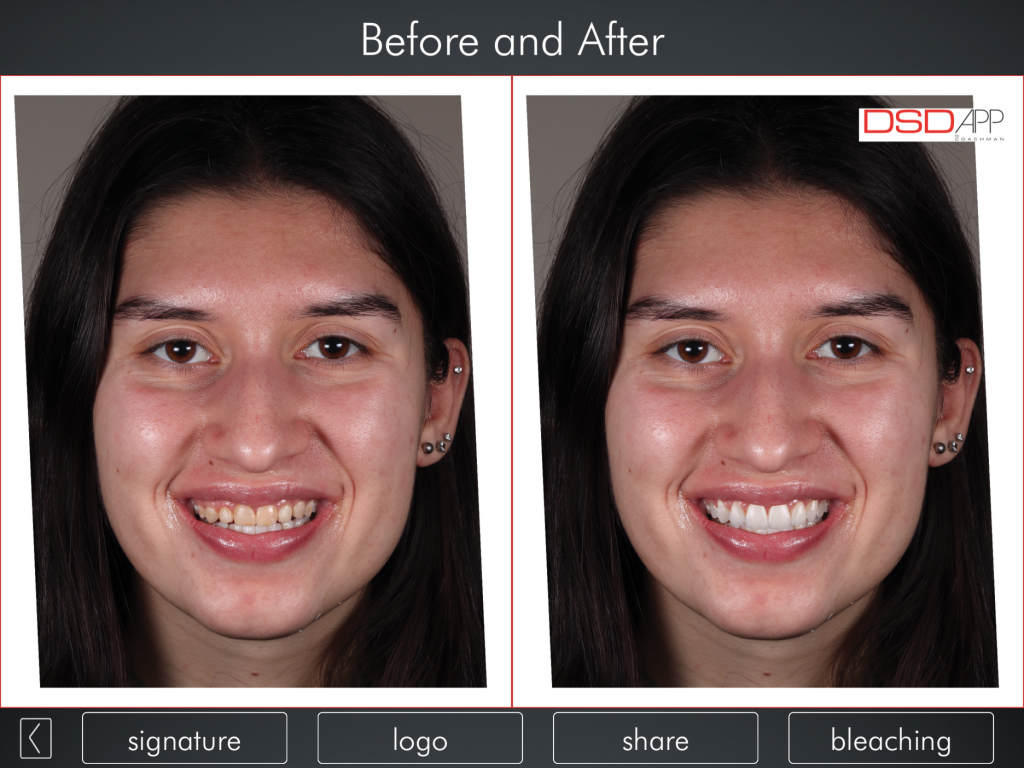
Figures 2 and 3. Digital smile design without aesthetic crown lengthening (Figure 2), and digital smile design with aesthetic crown lengthening (Figure 3).
Digital Wax-Up
She was scanned intraorally using the iTero Element 2 (Align Technology) in centric relation. The STL file was exported to the laboratory, where a digital wax-up was completed using DentalCAD (exocad GmbH) (Figures 4 and 5).
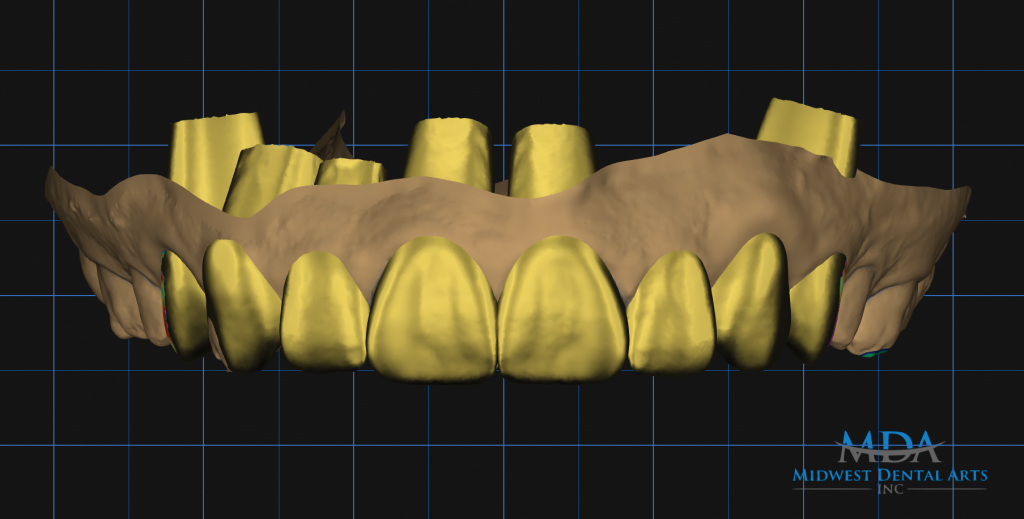
Figure 4.
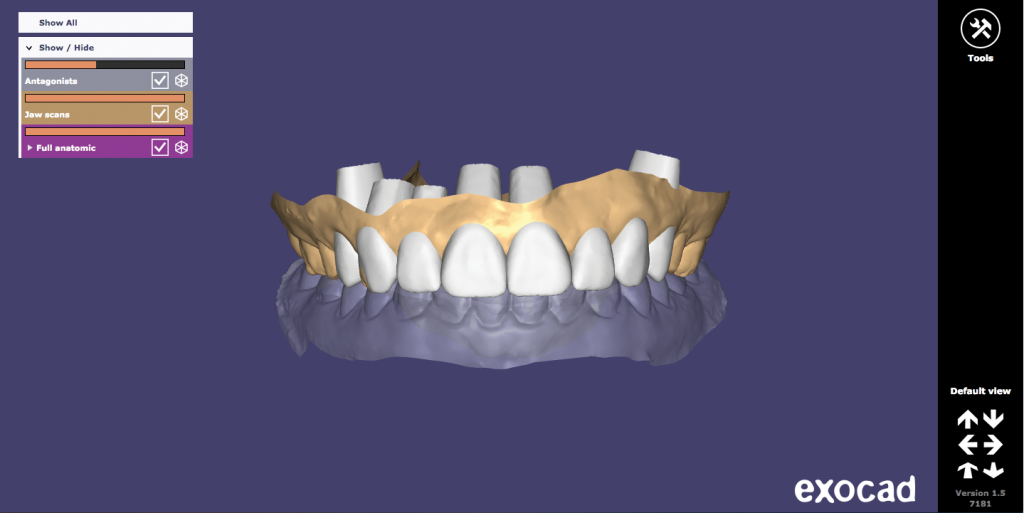
Figure 5. – Figures 4 and 5. Digital wax-up of the maxillary arch (Figure 4) and in occlusion in exocad DentalCAD (exocad GmbH) (Figure 5).
This digital wax-up was first overlaid with the digital smile design to verify the wax-up with respect to the patient’s face for facially driven treatment planning. The digital wax-up was then overlaid with the preoperative STL file to create the dual-zone crown lengthening guide (Figure 6).

Figure 6. A 3D printed pre-op model and digital wax-up.
The surgical guide contained 2 reference points: one for desired gingival margin position and another for desired osseous crest position set to 3 mm from the proposed restorative margin (Figure 7). The pre-op model, digital wax-up, and surgical guide were 3D printed in addition to a clear preparation guide and putty matrix for provisional fabrication.

Figure 7. A dual-zone surgical crown lengthening guide was printed and placed on the pre-op model.
Aesthetic Crown Lengthening
The patient was advised not to eat for 6 hours prior to the procedure in preparation for intravenous sedation. Following sedation, the patient was locally anesthetized using 4% Septocaine (1:100,000 epinephrine) (Septodont) (Figure 8).

Figure 8.

Figure 9.

Figure 10.

Figure 11.

Figure 12. – Figures 8 to 12. Pre-op view of aesthetic crown lengthening following administration of local anesthesia (Figure 8). Gingivectomy was completed using the Er,Cr:YSGG laser and dual-zone surgical crown lengthening guide (Figures 9 and 10). Ostectomy and osteoplasty were completed with the Er,Cr:YSGG laser and a round bur on a high-speed handpiece (Figure 11). Final closure was done using chromic gut sutures (Figure 12).
The dual-zone surgical crown lengthening guide was seated (Figure 9), and gingivectomy was completed using an Er,Cr:YSGG laser (Waterlase Express [BIOLASE]) (Figure 10). A full-thickness flap was raised from teeth Nos. 3 to 14 beyond the mucogingival junction to gain access to the facial and interproximal hard tissue. With the surgical guide in place, the biologic width of 3 mm was established from the future crown margin (Figure 11). Festooning of interproximal hard tissue was completed using a round diamond bur on a high-speed handpiece. The flap was replaced using a combination of 4-0 and 5-0 chromic gut sutures via vertical mattress for improved control of the interproximal papillae (Figure 12). The flap was replaced slightly coronal to the desired gingival margin position to account for shrinkage during healing. Postoperative instructions were given, including administration of Ibuprofen 800 mg every 8 hours, followed by Tylenol 1,000 mg for pain management.
Soft-Tissue Modification
The patient was seen for followup at 2 weeks for suture removal and at 8 weeks for soft-tissue modification (Figures 13 and 14). No local anesthesia was required for this visit, and soft-tissue modification was completed using the Er,Cr:YSGG laser to achieve symmetry and to idealize the gingival margin and zenith position.7 Detailed home care instructions were given, including brushing with the Roll technique and flossing only up to the contact area between each tooth.

Figure 13.

Figure 14. – Figures 13 and 14. A photo of 8-week postoperative healing, during which soft-tissue modification was completed using the Er,Cr:YSGG laser.
Preparation and Provisionalization
After 16 weeks of healing, the patient returned for preparation and provisionalization. Following administration of local anesthesia, teeth Nos. 5 to 12 were prepared to receive full-coverage crowns using the clear preparation guide, and provisionals were fabricated with Luxatemp Ultra (DMG America) shade A1 using the putty matrix that was based on the digital wax-up.
Whitening of Mandibular Dentition
The patient was advised to “test drive” the provisionals in order to make any necessary adjustments. During this time, the patient whitened her mandibular dentition using Opalescence Go (Ultradent Products) containing 10% hydrogen peroxide solution, which was used for 30 minutes per day for 10 days.
Final Prosthesis
The final impression was taken using Impregum (3M) with a 2-cord technique. The final shade of OM3 using VITA Toothguide 3D-Master (VITA North America) was selected with the patient’s input for IPS e.max Press (Ivoclar Vivadent). Crown Nos. 5 to 12 were cemented using NX3 Nexus Third Generation (Kerr Corporation). Occlusion was adjusted, and mutually protected occlusion was verified. The patient was seen for one-week, 3-month, and 12-month post-op visits (Figures 15 and 16).

Figure 15.

Figure 16. – Figures 15 and 16. The one-year post-op view with full smile (Figure 15), and a close-up view of the final prosthesis (Figure 16).
DISCUSSION
APE—one of the main causes of excess gingival display3,5—adversely affects both gingival architecture and tooth proportion. Clinical challenges include aberrant gingival margin position and papilla proportion as well as short clinical crowns and lack of retention and resistance form.5 The treatment of choice for APE is aesthetic crown lengthening, which includes inverse bevel gingivectomy in combination with osteoplasty and ostectomy.
There have been several clinical approaches to aesthetic crown lengthening, mostly based on analog methods, including the use of a proportion gauge9 and clear matrix based on a diagnostic wax-up. The proportion gauge, while providing an efficient method of verifying the desired width-to-length ratio of 75% to 80% and an osseous reduction of 3 mm,9 can be laborious for the operator since each anterior tooth has to be measured individually11 and also challenging when incisal edge positions are different from tooth to tooth. While it is based on a diagnostic wax-up, the clear matrix has its limitations when it comes to communicating exact gingival margin and zenith positions to the surgeon. The utilization of digital technology allows for visualization of the desired clinical outcome prior to surgery. This results in clear communication of the position and shape of the gingival margin and zenith as well as the osseous crest location to the surgeon so that aesthetic crown lengthening can be completed in a precise and exact manner.
CONCLUSION
The advent of digital technology has allowed for a novel approach to aesthetic crown lengthening. Digital smile design, a digital wax-up, and 3D printing provide an opportunity for facially driven treatment planning and an agreement in aesthetic parameters among the restorative dentist, surgeon, ceramist, and patient.
In the case described above, digital technology was able to improve communication between providers, and the incorporation of cutting-edge technology such as the Er,Cr;YSGG laser resulted in an aesthetic and a personalized clinical outcome for our patient.
ACKNOWLEDGMENTS
We would like to thank Calvin Mun from Jason J. Kim Dental Aesthetics Laboratory in Port Washington, NY, for the ceramic work and Dr. Jonathan Mendia of Advanced Sedation in Old Tappan, NJ, for keeping the patient comfortable with intravenous sedation.
REFERENCES
1. Fradeani M. Esthetic analysis: a systemic approach to prosthetic treatment. Quintessence Publishing Company; 2004.
2. Goldman HM, Cohen DW. Periodontal therapy. 4th ed. C.V. Mosby Company; 1968.
3. Robbins JW. Differential diagnosis and treatment of excess gingival display. Pract Periodontics Aesthet Dent. 1999;11(2):265–72.
4. Tjan AH, Miller GD, The JG. Some esthetic factors in a smile. J Prosthet Dent. 1984;51(1):24–8. doi:10.1016/s0022-3913(84)80097-9
5. Dolt AH 3rd, Robbins JW. Altered passive eruption: an etiology of short clinical crowns. Quintessence Int. 1997;28(6):363–72.
6. Chu SJ, Tarnow DP, Tan JH, et al. Papilla proportions in the maxillary anterior dentition. Int J Periodontics Restorative Dent. 2009;29(4):385–93.
7. Chu SJ, Tan JH, Stappert CF, et al. Gingival zenith positions and levels of the maxillary anterior dentition. J Esthet Restor Dent. 2009;21(2):113–20. doi:10.1111/j.1708-8240.2009.00242.x
8. Coslet JG, Vanarsdall R, Weisgold A. Diagnosis and classification of delayed passive eruption of the dentogingival junction in the adult. Alpha Omegan. 1977;70(3):24–8.
9. Fletcher P. Biologic rationale of esthetic crown lengthening using innovative proportion gauges. Int J Periodontics Restorative Dent. 2011;31(5):523–32.
10. Jafri Z, Ahmad N, Sawai M, et al. Digital smile design—An innovative tool in aesthetic dentistry. J Oral Biol Craniofac Res. 2020;10(2):194–8. doi:10.1016/j.jobcr.2020.04.010
11. Chu SJ. Range and mean distribution frequency of individual tooth width of the maxillary anterior dentition. Pract Proced Aesthet Dent. 2007;19(4):209–15.
ABOUT THE AUTHORS
Dr. Kang received his DMD degree from the University of Pennsylvania and his MS in Periodontics from Columbia University. He is a Diplomate of the American Board of Periodontology. Dr. Kang serves as Clinical Advisor for Geistlich Biomaterials and is a member and reviewer of the e-Poster Committee at the Academy of Osseointegration Annual Meeting. Dr. Kang employs cutting-edge technology, such as an Er,Cr;YSGG laser, for minimally invasive treatment of periodontal disease and peri-implantitis and for aesthetic crown lengthening. He can be reached at justintkang@gmail.com.
Dr. Hon received her DMD degree from University of Medicine and Dentistry of New Jersey and completed her general practice residency at the VA Medical Center in East Orange, NJ. Dr. Hon specializes in cosmetic dentistry and Invisalign. When not practicing, Dr. Hon is a busy mother of 2 boys and enjoys playing tennis. She can be reached at hon.dmd@gmail.com.
Dr. Resnick received his DDS degree from New York University (NYU) and continued his training in prosthodontics at Montefiore Medical Center in the Bronx, NY. Dr. Resnick is a dual-trained specialist in both prosthodontics and implant surgery with a special focus on porcelain veneers and cosmetic dentistry. Dr. Resnick enjoys traveling with his family, playing golf, and cooking. He can be reached at leonardresnick@gmail.com.
Mr. McElroy is VP of business development at Midwest Dental Arts in Sarasota, Fla. He completed a digital smile design residency at NYU and has been an active contributor to the digital smile design concept. Mr. McElroy also teaches dental photography and digital workflows across the country. He can be reached at midwestdentalarts@gmail.com.
Disclosure: The authors report no disclosures.












