
As dentists, we have been comfortable working in a 2D world when evaluating our patients. However, an orthopedic physician’s assistant once told me that one x-ray view is no x-ray views. I took that to heart when I bought my cone-beam CT (CBCT) scanner.
After endless research of multiple companies, I decided on a new company in the market, HDXWILL, for its clarity and ability to provide 3D tools that can enhance every aspect of my practice.
Entering the 3D realm, I created protocols that would define when I would choose to use the 3D CBCT for my patients. With the information I was able to obtain for my diagnosis and the diagnostic clarity that a 3D image has in comparison to a 2D image, my protocols have grown. With this valuable tool and its ease of use, I can provide a much more comprehensive diagnosis and treatment plan to my patients.
Case Report
A patient came to my office complaining of a lump on his palate. In the past, I would have taken a 2D x-ray and referred him to my endodontist. Periapical radiographs are only 26% to 48% accurate in diagnosing a periodical lesion (Figure 1).1
However, CBCT is more accurate than periapical radiographs in revealing periapical pathosis.2,3 CBCT is also more accurate than periapical radiographs in identifying apical periodontitis, especially when lesions are greater than 1.4 mm.2,3 CBCT, with its high specificity and accuracy, can enhance pre-op diagnoses as well as post-op evaluation of treatment.
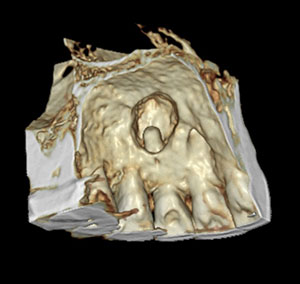
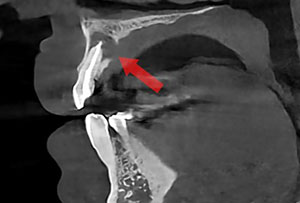
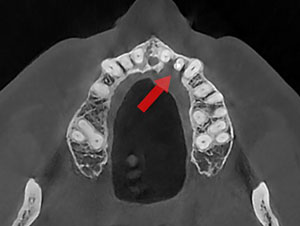
After reviewing the CBCT imaging, I was able to explain to the patient that he had a periapical lesion that had caused the bone to resorb (Figures 2 and 3). I showed him the effects of the infection including the bone resorption with a 3D image that he could understand, and we discussed how and why some cases require periapical surgery.
I also informed the patient that, due to the size of the lesion, there was a possibility the endodontist would have to repair the lesion in two visits instead of the one visit that previous root canals required.
 |
 |
| Figure 2. Bone mode in a CBCT scan provides a 3D rendering. | Figure 3. Teeth mode in a CBCT scan provides a 3D rendering. |
 |
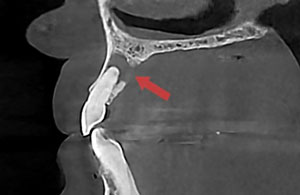 |
| Figure 4. The axial view in a CBCT scan shows lingual bone resorption. | Figure 5. The saggital view in a CBCT scan shows lingual bone resorption. |
 |
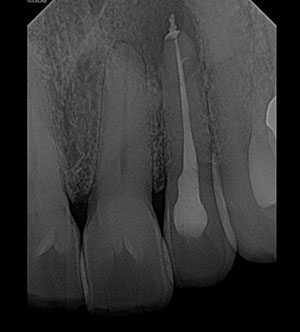 |
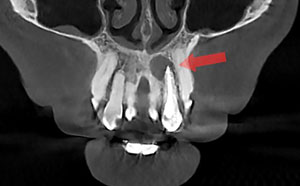
| Figure 6. The CBCT scan can provide a coronal view. | Figure 7. The post-op periapical image shows tooth No. 10. |
 |
 |
| Figure 8. The post-op CBCT scan can provide a coronal view. | Figure 9. The post-op CBCT scan can provide a saggital view. |
 |
 |
| Figure 10. The post-op CBCT scan in teeth mode can provide a 3D rendering. |
Figure 11. The post-op CBCT scan can provide an axial view. |
In this scenario, the patient and I both participated in the diagnosis and decision-making process. Before this technology, treatment was decided at the specialist’s office without input from the referring dentist.
The 2D image showed a lesion, but it did not define the buccal/lingual extent the lesion had progressed. With multiple 3D slices, the true nature of the lesion could be defined (Figures 4, 5, and 6). The 3D rendering of where the lesion had erupted through the lingual wall provided a comprehensive visual for diagnosis (Figure 2 again).
That visual was also paramount in demonstrating the issue in a way that was easier for my patient to visualize and understand. I passionately believe that with patient understanding, the appropriate treatment plan is much easier to actuate and gain acceptance.
I scheduled a six-month return to my office post-treatment to assess the healing of the lesion and the endodontic procedure (Figures 4, 5, and 6 again and Figures 7 through 10).
Overall Benefits
This information is then used in the overall assessment of the root canal’s healing and provides information on the long-term prognosis of the tooth involved. Both non-surgical and surgical endodontic treatments have shown a very high success rate.
In post-op evaluations, it should be noted endodontic periapical lesions do remain in some cases.4 In order to assess the healing of the lesion, a six- to 12-month follow-up is recommended (Figure 10 again).5 CBCT evaluation of the shaping and sealing of the canal can help in detecting possible inadequacies in the obliteration on the canal that conventional 2D x-rays cannot provide (Figures 8 and 9 again and Figure 11).
Changes in the periapical lesion can be shown in the merging of subsequent CBCTs over the six-month time frame, providing visualization of the lesion in all three orthogonal planes for dimensional changes. Decisions can then be made concerning restorative options and time frame based off of this information.
As dentists, we need to perform a thorough assessment, evaluation, and diagnosis of our patients. This can be accomplished more readily by incorporating advanced diagnostic technologies such as the CBCT. In this way, we are not just focusing on the dentition and surrounding periodontal tissue, but can expand to other parts of the oral cavity, head, and neck.
Before, I was transferring this responsibility to several specialists, excluding me from the continuity of care for my patients. Now, I can be more focused and inclusive of my diagnosis and needed referrals, saving my patient both time and money. Moving into the 3D realm has immensely helped my practice to better accomplish the universal goal of creating a comprehensive treatment continuity that works toward a better outcome for every patient.
References
- Mortensesn H, Winther J, Birn H. Periapical granulomas and cysts: An investigation of 1,600 cases. Eur J Oral Sci. 1970;78(1-4):241-50.
- Estrela C, Bueno MR, Azevedo BC, Azevedo JR, Pécora JD. A new periapical index based on cone beam computed tomography. J Endod. 2008;34(11):1325-31.
- Tsai P, Torabinejad M, Rice D, Azevedo B. Accuracy of cone-beam computed tomography and periapical radiography in detecting small periapical lesions. J Endod. 2012;38(7):965-70.
- Karamifar, K. (2020). Endodontic Periapical Lesion: An Overview on Etiology, Diagnosis and Current Treatment Modalities. European Endodontic Journal, 1–6. https://doi.org/10.14744/eej.2020.42714
- Orstavik D. Time-course and risk analyses of the development and healing of chronic apical periodontitis in man. Int Endod J. 1996;29(3):150-5.
Dr. Steffen is a general dentist in private practice in Tulsa, Oklahoma. He received his dental training at Washington University in St. Louis. He also maintains an academic presence by lecturing and teaching. He currently works with many major dental companies on the development of digital workflows in the dental office. He has a non-paid consultant position with HDXWILL as well.
Related Articles
Reconstruction of the Nose and Maxillary Arch
Treating a Patient With Inadequate Restorative Space
CBCT System Boasts Ultra-HD Imagery











