During the past few years, the literature has been strongly supportive of a distinct link between oral disease, mainly periodontitis, and a host of systemic entities. It has become more and more apparent that the relationship is related to the inflammatory response. The host immune mechanism, which is both a local and a systemic phenomenon, is an integral part of the puzzle, inasmuch as it is so intimately a part of the inflammatory process.
The contemporary and constantly evolving standard of care now dictates that the general dentist be an integral part of the recognition and control of the oral inflammatory pathoses. As healthcare providers, we share the responsibility for our patients’ general medical health.1 The most ubiquitous conditions within our purview, with the greatest incidence, are the periodontal diseases. This article will review the development of the inflammatory response in the periodontal patient, discuss its relationship to systemic disease, and outline the dentist’s role in recognition and management.
 |
 |
|
Figure 1. Pathologic inflammatory reaction. |
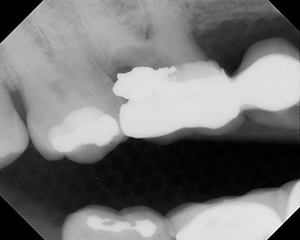
Figure 2. Type III periodontitis in diabetic with poor glycemic control. |
 |
 |
|
Figure 3. Lateral border of tongue. |
Figure 4. Fluorescence with ViziLite (Zila Pharmaceuticals). |
 |
| Figure 5. Retention of toluidine blue, later diagnosed through biopsy as severe dysplasia. |
| Table 1. |
||||
“The red cluster” of critical periodontal pathogens
|
The gram negative periodontopathogens, especially those in the “red cluster or complex” (Table 1),5 appear to have the capacity to initiate the production of a number of inflammatory mediators, such as cytokines,6,7 in addition to their direct invasive, destructive roles. The primary goal of early intervention in periodontal anti-infective therapy is to reduce the bacterial load, and thus limit the inflammatory response of the immune system. Removal of the subgingival biofilm by instrumentation can remove up to 90% of the microbial deposits on the root surface.8
There are a number of mechanisms that constitute part of the host immune response that either protect the tissues or initiate and promote destruction. This variability of the responses is an important factor in how the periodontal diseases are expressed in the population.9,10 It is the immunopathologic aspect of the immune response that creates the inflammatory response and the subsequent destruction (Figure 1). There are numerous contributory risk factors that may affect the nature and intensity of the immune response, in addition to host variability. These factors that modify the host response contribute to the systemic nature of the inflammation. For example, smoking has been shown to impair polymorphonuclear leukocyte function and promote the production of proinflammatory cytokines.11,12 Table 2 lists some, but not all, of the many risk factors that influence the nature of the inflammatory response in contributing to the onset of periodontal pathosis and its sequelae.
The immune response, resulting in inflammation and tissue destruction, is a complex interaction of cellular events resulting in the release of metabolites that result in destruction of the collagen supporting the connective tissue, and eventually supporting alveolar bone. The highly cellular local response revolves around the chemotactic response of leukocytes, the influx of B and T lymphocytes, macrophages, and the presence of fibroblasts, all of which contribute to the admix of cytokines, leukotrienes, and other destructive metabolites.13,14 The resulting inflammatory response is far from purely a localized phenomenon. While periodontal disease is, indeed, often a site-specific phenomenon, the mediators or metabolites produced are disseminated systemically. This is the critical rationale for suppression or reduction of the immune inflammatory response of periodontal disease.
| Table 2. | ||||||||||||
|
| Table 3. | ||||||||||||
Systemic conditions with evidence linked to periodontal inflammation
|
The added risk of CHD in combination with diabetes makes cardiovascular disease the number one cause of mortality in diabetics.18,24 Again, it is because of the compromised immune system of the diabetic, resulting in altered inflammatory responses, that periodontitis is considered the sixth complication of diabetes.25 The diabetic with periodontal inflammation, as in Figure 2, presents with reduced glucose tolerance, increased resistance to insulin, and dramatically increased risk for all of the complications of diabetes including cardiovascular disease.
There are numerous other systemic sequelae linked to periodontal inflammation, with more links and associations being suggested almost daily in the literature.26-32 There is another relationship with inflammatory periodontal disease that, currently, is being intensively investigated. The alarming morbidity and mortality of oral/pharyngeal cancer, especially oral squamous cell carcinoma (OSCC), appears to have a definitive relationship to oral inflammation and to the human papilloma virus (HPV).32 Chronic periodontitis is associated with increased risk for cancer of the tongue33, and pancreatic cancer in men has been linked to poor oral hygiene and periodontal disease.34 It is suggested that elevated levels of nitrosamines in the gut react with digestive chemicals to create conditions that favor development of pancreatic cancer. The elevated levels of C reactive protein (CRP) are part of an early immune system response to persistent inflammation, and have been linked to the development of pancreatic cancer.35,36
The consistent thread that binds all of these observations together is the presence of inflammation, resulting from periodontal pathology. The implications for dentistry are enormous. The dental profession, armed with the ability to detect the early changes in oral tissues by using currently available technology, such as adjunctive oral cancer screen-ing techniques (eg, ViziLite [Zila Pharmaceuticals]) (Figures 3 to 5), is in a position to reverse the ominous trends in morbidity and mortality of OSCC by visualizing cellular changes before they can be seen by the unaided eye. This noninvasive test, with a 99% negative predictive value, is a major step forward in early detection.
CONCLUSION
The inflammatory component of both cancer and other systemic entities is within our control. Understanding the importance of early recognition and instituting measures for control is precisely what periodontal management is all about. Our ability to suppress the inflammatory response with instrumentation, adjunctive therapy (including host modulation), and daily disease control, puts the general practitioner and hygienist at the forefront of this enormous public health issue, and we can make a huge difference.
References
- Glick M. Exploring our role as health care providers: the oral-medical connection. J Am Dent Assoc. 2005;136:716-720.
- Paster BJ, Olsen I, Aas JA, et al. The breadth of bacterial diversity in the human periodontal pocket and other oral sites. Periodontol 2000. 2006;42:80-87.
- Kroes I, Lepp PW, Relman DA. Bacterial diversity within the human subgingival crevice. Proc Natl Acad Sci U S A. 1999;96:14547-14552.
- Feng Z, Weinberg A. Role of bacteria in health and disease of periodontal tissues. Periodontol 2000. 2006;40:50-76.
- Socransky SS, Haffajee AD. Periodontal microbial ecology. Periodontol 2000. 2005;38:
135-187. - Tonetti MS, Gerber L, Lang NP. Vascular adhesion molecules and initial development of inflammation in clinically healthy human keratinized mucosa around teeth and osseointegrated implants. J Periodontal Res. 1994;29:386-392.
- Gemmell E, Marshall RI, et al. Cytokines and prostaglandins in immune homeostasis and tissue destruction in periodontal disease. Periodontol 2000. 1997;14:112-143.
- Teles RP, Haffajee AD, Socransky SS. Microbio-logical goals of periodontal therapy. Periodontol 2000. 2006;42:180-218.
- Van Dyke TE, Sheilesh D. Risk factors for periodontitis. J Int Acad Periodontol. 2005;7:3-7.
- Schenkein HA. Host responses in maintaining periodontal health and determining periodontal disease. Periodontol 2000. 2006;40:77-93.
- van der Vaart H, Postma DS, Timens W, et al. Acute effects of cigarette smoke on inflammation and oxidative stress: a review. Thorax. 2004;59:713-721.
- Bostrom L, Linder LE, Bergstrom J. Smoking and cervicular fluid levels of IL-6 and TNF-alpha in periodontal disease. J Clin Periodontol. 1999;26:352-357.
- Page RC, Schroeder HE. Pathogenesis of in-flammatory periodontal disease. A summary of current work. Lab Invest. 1976;34:235-249.
- Teng YT. The role of acquired immunity and periodontal disease progression. Crit Rev Oral Biol Med. 2003;14:237-252.
- Loos BG. Systemic markers of inflammation in periodontitis. J Periodontol. 2005;76(11 suppl):
2106-2115. - Beck JD, Eke P, Heiss G, et al. Periodontal disease and coronary heart disease: a reappraisal of the exposure. Circulation. 2005;112:19-24.
- Offenbacher S, Boggess KA, Murtha AP, et al. Progressive periodontal disease and risk of very preterm delivery [published correction appears in Obstet Gynecol. May 2006;107:1171]. Obstet Gynecol. Jan 2006;107:29-36.
- Saremi A, Nelson RG, Tulloch-Reid M, et al. Periodontal disease and mortality in type 2 diabetes. Diabetes Care. 2005;28:27-32.
- Williams RC, Offenbacher S. Periodontal medicine: the emergence of a new branch of periodontology. Periodontol 2000. 2000;23:9-12.
- Grau AJ, Becher H, Ziegler CM, et al. Periodontal disease as a risk factor for ischemic stroke. Stroke. 2004;35:496-501.
- Haraszthy VI, Zambon JJ, Trevisan M, et al. Identification of periodontal pathogens in atheromatous plaques. J Periodontol. 2000;71:1554-1560.
- Starkhammar Johansson C, Richter A, Lundstrom A, et al. Periodontal conditions in patients with coronary heart disease: a case control study. J Clin Periodontol. 2008;35:199-205.
- Turkoglu O, Baris N, Kutukculer N, et al. Evaluation of serum anti-cardiolipin and oxidized low-density lipoprotein levels in chronic periodontitis patients with essential hypertension. J Periodontol. 2008;79:332-340.
- Thorstensson H, Kuylenstierna J, Hugoson A. Medical status and complications in relation to periodontal disease experience in insulin-dependent diabetics. J Clin Periodontol. 1996;23(3 pt 1):194-202.
- Loe H. Periodontal disease: the sixth complication of diabetes mellitus. Diabetes Care. 1993;16:329-334.
- Scannapieco FA. Periodontal inflammation: from gingivitis to systemic disease? Compend Contin Educ Dent. 2004;25(7 suppl 1):16-25.
- Scannapieco FA, Bush RB, Paju S. Associations between periodontal disease and risk for nosocomial bacterial pneumonia and chronic obstructive pulmonary disease: a systematic review. Ann Periodontol. 2003;8:54-69.
- Krall EA. The periodontal-systemic connection: implications for treatment of patients with osteoporosis and periodontal disease. Ann Periodontol. 2001;6:209-213.
- Kunnen A, Blaauw J, van Doormaal JJ, et al. Women with a recent history of early-onset pre-eclampsia have a worse periodontal condition. J Clin Periodontol. 2007;34:202-207.
- Stein PS, Desrosiers M, Donegan SJ, et al. Tooth loss, dementia and neuropathology in the Nun study. J Am Dent Assoc. 2007;138:1314-1322.
- Ebersole JL, Machen RL, Steffen MJ, et al. Systemic acute-phase reactants, C-reactive protein and haptoglobin, in adult periodontitis. Clin Exp Immunol. 1997;107:347-352.
- Chaturvedi AK, Engels EA, Anderson WF, et al. Incidence trends for human papillomavirus-related and -unrelated oral squamous cell carcinomas in the United States. J Clin Oncol. 2008;26:612-619.
- Garcia RI, Henshaw MM, Krall EA. Relationship between periodontal disease and systemic health. Periodontol 2000. 2001;25:21-36.
- Tezal M, Sullivan MA, Reid ME, et al. Chronic periodontitis and the risk of tongue cancer. Arch Otolaryngol Head Neck Surg. 2007;133:450-454.
- Michaud DS, Joshipura K, Giovannucci E, et al. A prospective study of periodontal disease and pancreatic cancer in US male health professionals. J Natl Cancer Inst. 2007;99:171-175.
- Glick M. Risky liaisons: what is the relationship between oral conditions and nonoral diseases? J Am Dent Assoc. 2007;138:1056-1060.
Dr. Bader practices periodontics and implant dentistry in Concord, Mass. He is a graduate of NYU College of Dentistry, and in 1966 completed a residency in periodontology at the Harvard School of Dental Medicine, where he currently serves as lecturer in postgraduate periodontology. He is a fellow of the American College of Dentists, International College of Dentists, and American Academy of Osseointegration. He has been published in the Journal of Dental Research, Journal of Periodontology, Journal of Clinical Periodon-tology, and the American Journal of Dentistry. He can be reached at redabsr@aol.com.