The aesthetic zone in patients with a medium or high lip line at smile includes the dentition and the dentogingival area exposed from the most posterior visible maxillary tooth to the midline.1 Aesthetic, anatomic, and biologic parameters provide clinicians with an understanding of the problem. This leads to an accurate diagnosis, then a treatment plan. The result should be successful treatment that meets the patient’s aesthetic expectations. Parameters may include the lip line, gingival margin, texture, color and contour of the gingiva, and tooth length, shape, composition, axis, contact points, occlusal plane, and angulation.2
In patients with a high lip line at smile, excessive gingival display is often observed. It may be due to skeletal reasons or be associated with maxillary prognathism, a short upper lip, and/or incomplete passive eruption (IPE).2,3 The first cause can be corrected if orthognathic surgery is indicated, while the last cause can be managed by aesthetic crown lengthening. In addition to the amount of gingival display, the gingival line is an equally important parameter.4 Ideally, the gingival line should be parallel to both the interpupillary line and the incisal line. The gingival margin of the lateral incisor is often found to be in a slightly coronal position. Discrepancies of the gingival line can also be altered by orthodontic extrusion or intrusion, gingival augmentation, or aesthetic crown lengthening.
Delayed, altered, or incomplete passive eruption are terms that have been used to describe the anatomical condition where the free gingival margin fails to migrate apically in proximity to the cementoenamel junction (CEJ). In this situation it is located more than 2 mm coronal to the CEJ.5-7 Coslet, et al developed a classification and diagnostic system based on both soft-tissue and hard-tissue relationships.8 IPE is classified into 2 types according to the soft-tissue dimension. Type I patients present with a noticeably wider band of gingiva from the gingival margin to the mucogingival junction (MGJ), which extends apical to the alveolar crest. Type II patients present with a band of normal width gingiva in which all of the gingiva is located on the anatomic crown and the MGJ is located at the level of the CEJ. Both types are then divided into subgroups A and B. In the A subgroups, the alveolar crest-to-CEJ dimension is 1.5 to 2.0 mm. In the B subgroups, the alveolar crest-to-CEJ distance is too small for the biological width to be established. Accurate diagnosis is important in the treatment of IPE because it helps the clinician plan the appropriate surgical technique for aesthetic crown lengthening.
Apical to the gingival line the texture, color, and contour of the gingival tissue must be evaluated.2,4 Inflammation associated with gingivitis or periodontitis will result in tissue that appears red and edematous, and stippling may be absent. As a result, the tissue does not appear natural. The presence of an adequate band of attached gingiva in the aesthetic zone is important. Absence of a firm and adequate band of attached gingiva may result in recession,9 a greater likelihood of inflammation, and increased trauma due to oral hygiene. If porcelain-fused-to-metal (PFM) restorations are present, the metal margin is more likely to show through the gingival margin when it is thin, or may be exposed if gingival recession occurs.
An amalgam tattoo is another type of soft-tissue discoloration that is related to amalgam in the tissue. It occurs as a macular or slightly elevated blue, black, or gray pigmentation in the gingiva, alveolar mucosa, buccal mucosa, or mucobuccal fold. Amalgam can be incorporated into the oral mucosa in one of several ways: (1) condensation of the material into the gingival tissue during the placement of an amalgam restoration; (2) damage to the gingiva by a cutting instrument during removal of an existing amalgam restoration; (3) accidental dislodgment into the socket of broken pieces of amalgam restoration during tooth extraction; or (4) corrosion of retrograde amalgam restoration of endodontically treated teeth.10-12 Depending on the particle size, the silver in the amalgam may be directly phagocytized by macrophages or encapsulated by connective tissue.
Uneven gingival line, high smile line, IPE, defective restoration, and amalgam tattoo can be found either individually or combined in a patient. A case is discussed in which the patient presented with all of the aforementioned problems. The diagnostic assessment, treatment planning, and treatment are described to illustrate the importance of multidisciplinary cooperation in a complicated case.
CASE REPORT
Initial Examination
 |
 |
|
Figure 1. The patient with a high lip line at smile. Note the presence of exposed crown margins on the central incisors as well as the bluish hue of the anterior gingiva. |
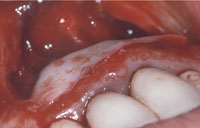
Figure 2. Uneven gingival margin with size and shape discrepancies among the maxillary anterior teeth. Note the presence of a large amalgam tattoo with scarring from previous periapical surgery. |
A 45-year-old healthy white female presented with a chief complaint that she “was embarrassed to smile because of the appearance of her teeth and discolored gums” (Figure 1). She had a high lip line and an uneven gingival line. There was a size and shape discrepancy among her maxillary anterior teeth (Figure 2). The maxillary left central incisor crown was greatly overcontoured. The crown margins of the central incisors were exposed, contributing to the poor aesthetics. Periodontal evaluation determined probing depths of 4 to 5 mm in the anterior sextant, and the tissue bled upon probing. The patient had thick gingiva that appeared edematous, and the marginal tissue was inflamed and enlarged.
Radiographic examination demonstrated mild horizontal bone loss. Multiple discolored and open composite restorations were seen on the remaining incisor and cuspid teeth. A very large area of discoloration was present in the maxillary anterior segment. The patient had a history of apical surgery on all 4 incisor teeth. The tissue was not only discolored but also demonstrated extensive scarring of the mucosa that was further evidence of the previous surgical interventions.
Sequence of Therapy
1. Initial supragingival and subgingival debridement and oral hygiene instruction.
2. Thorough root planing and scaling.
3. Provisional restorations to improve both the patient’s appearance and ability to cleanse the area.
4. Surgical removal of the large amalgam tattoo.
5. Aesthetic crown lengthening to establish symmetry and correct the tooth size/shape discrepancies.
 |
 |
|
Figure 3. The affected hard and soft tissue has been removed. Note the presence of lesions over the apices that were filled with amalgam. |
Figure 4. The beveled edge of the graft placed coronally to blend with the surrounding soft tissue. |
 |
 |
|
Figure 5. One-week follow-up. |
Figure 6. Two-week follow-up. |
 |
 |
|
Figure 7. Aesthetic crown lengthening of maxillary right cuspid, lateral, and central incisor teeth and removal of fibroma between the maxillary central incisors. |
Figure 8. Two-year follow-up. |
Removal of the amalgam tattoo was performed utilizing a circumferential incision with a 1-mm clear border around the margins of the lesion. The affected tissue was excised (Figure 3). The remaining amalgam deposits were debrided first with curettes and later with high-speed rotary instruments utilized on the affected bone. Near the apices of the teeth, large round defects were found to be filled with amalgam and granulomatous tissue. After thoroughly debriding these defects, they were filled with demineralized freeze-dried bone allograft. A large free gingival graft (30 x 10 mm) was then removed from the left side of the posterior palate using an angled blade holder. The graft was placed at the recipient site in such a way that the beveled edge was directed coronally to blend with the surrounding tissues (Figure 4). The graft was then secured with 5-0 chromic gut suture using a continuous loop. It was carefully adapted to the underlying bed with cross-sutures secured to the periosteum. Periodontal dressing (COE-PAK [GC America]) was applied to the graft to protect the wound and maintain vestibular depth.
After one week, the graft appeared to be well vascularized and was beginning to blend in with the surrounding tissue despite slough of the surface epithelium (Figure 5). At 2 weeks, a wide zone of epithelialized at tached gingiva was present. The discolored scar tissue could no longer be observed (Figure 6).
After 8 weeks of healing, the second phase of the periodontal surgery was performed to establish symmetry and correct the size and shape discrepancies in the aesthetic zone. After bone sounding, it was determined that the patient could maintain adequate biologic width even after the removal of 1 to 2 mm of keratinized tissue. Gingivectomy/gingivoplasty was determined to be the least invasive and most efficient approach. After careful measurement, it was decided to remove 1 to 2 mm of gingiva in a scalloped incision on the right cuspid, lateral incisor, and central incisor teeth in order to achieve symmetry with the left side (Figure 7).
After 8 weeks of healing, the final restorations were inserted. The patient was pleased with the aesthetic results that addressed her chief complaint. At the 2-year postoperative visit, the periodontium and anterior dentition appeared to be healthy, and there was no rebound from the crown lengthening, nor was there recurrence of the amalgam tattoo (Figure 8).
DISCUSSION
The patient presented with at least 3 aesthetic problems: an uneven gingival margin when comparing the maxillary right and left anterior segments, an overcontoured crown on the maxillary left central incisor, and a large amalgam tattoo and scar tissue in the anterior apical area. The patient also had a high lip line. Discussion and communication with the pa tient and restorative dentist are crucial in a case with multiple problems, and should be accomplished very early in the sequence of appointments. In this case, the goal of the initial treatment (scaling and root planing, provisional restoration) was to reduce gingival inflammation and improve home care. Only when gingival inflammation has been reduced can the treatment plan, including consideration of aesthetic concerns, be fully developed. During the surgical phase the unpleasant amalgam tattoo and scar tissue were re moved, and the gingival line was altered by means of aesthetic crown lengthening. Finally, permanent crowns with proper contour and color were fabricated.
Several surgical modalities have been advocated for the treatment of an amalgam tattoo.10,13-17 One of the first approaches that was introduced for small, superficial lesions is to perform a localized gingivoplasty with a rotary instrument.10 Ashinoff and Tanenbaum documented the use of a Q-switched ruby laser in the anterior maxilla area.13 For larger lesions, a free gingival autograft, sub-epithelial connective tissue graft, or an allograft (acellular dermal matrix) have been suggested approaches.14,16-17 Autogenous soft-tissue grafts are limited by tissue availability and the second surgical site to collect donor tissue. This donor site may increase postsurgical complications and patient discomfort. In one technique, a second-stage surgery is required for further removal of tissue that contains amalgam.16 Allo-graft substitution, as described by Griffin, et al, eliminates the need for a second surgical donor site.17 Patient acceptance is often a consideration. In this case, after clinical examination it was found that not only did the patient have what can be described as a thick periodontium, but also that an adequate amount of autogenous tissue could be harvested from the palate. Therefore, based on the clinical findings and with consideration of the patient’s desires, a free gingival autograft technique was chosen.
Techniques of aesthetic crown lengthening and their indications have been described in the literature.7,18-19 Prior to the procedure, the following criteria should be considered:
• ideal gingival line
• amount of keratinized tissue that is present
• crown-to-root ratio
• characteristics of the periodontium, ie, thickness
• biological width.
Then, an appropriate surgical technique is applied based on the evaluation. If removal of marginal alveolar bone is not required and the amount of attached gingiva is adequate (ie, Type IA), then gingivectomy is the choice with or without gingivoplasty. If an adequate amount of attached gingiva (ie, Type IIA) and biological width needs to be established (ie, Type B subgroups) by removing labial crestal alveolar bone, then a flap procedure is employed for access. In the case presented, since the base of the sulcus was at least 2 mm away from the future crown margin and there was an adequate amount of keratinized tissue (ie, Type 1A), it was determined that gingivectomy by internal bevel incision was the best approach to achieve the desired final result.
CONCLUSION
A case has been described in which the patient presented with multiple aesthetic, prosthetic, and periodontal problems. The diagnostic assessment, treatment planning, and surgical procedures used to address these problems illustrate the importance of a multidisciplinary approach in the restoration of such cases.
References
1. Dong JK, Jin TH, Cho HW, et al. The esthetics of the smile: a review of some recent studies. Int J Prosthondont. 1999;12:9-19.
2. Garber DA, Salama MA. The aesthetic smile: diagnosis and treatment. Periodontol 2000. 1996;11:18-28.
3. Ezquerra F, Berrazueta MJ, Ruiz-Capillas A, et al. New approach to the gummy smile. Plast Reconstr Surg. 1999;104:1143-1152.
4. Caudill R, Chiche G. Establishing an esthetic gingival appearance. In: Chiche GJ, Pinault A. Esthetics of Anterior Fixed Prosthodontics. Hanover Park, Ill: Quintessence Publishing Co; 1994.
5. Weinberg MA, Eskow RN. An overview of delayed passive eruption. Compend Contin Educ Dent. 2000;21:511-518.
6. Dolt AH III, Robbins JW. Altered passive eruption: an etiology of short clinical crowns. Quintessence Int. 1997;28:363-372.
7. Hempton TJ, Esrason F. Crown lengthening to facilitate restorative treatment in the presence of incomplete passive eruption. J Mass Dent Soc. 1999;47:17-24.
8. Coslet JG, Vanarsdall R, Weisgold A. Diagnosis and classification of delayed passive eruption of the dentogingival junction in the adult. Alpha Omegan. 1977;70:24-28.
9. Kennedy JE, Bird WC, Palcanis KG, et al. A longitudinal evaluation of varying widths of attached gingiva. J Clin Periodontol. 1985;12:667-675.
10. Buchner A, Hansen LS. Amalgam pigmentation (amalgam tattoo) of the oral mucosa. A clinicopathologic study of 268 cases. Oral Surg Oral Med Oral Pathol. 1980;49:139-147.
11. Holmstrup P. Reactions of the oral mucosa related to silver amalgam: a review. J Oral Pathol Med. 1991;20:1-7.
12. Owens BM, Schuman NJ, Johnson WW. Oral amalgam tattoos: a diagnostic study. Compendium. 1993;14:210-214.
13. Ashinoff R, Tanenbaum D. Treatment of an amalgam tattoo with the Q-switched ruby laser. Cutis. 1994;54:269-270.
14. Dello Russo NM. Esthetic use of a free gingival autograft to cover an amalgam tattoo: report of case. J Am Dent Assoc. 1981;102:334-335.
15. Shiloah J, Covington JS, Schuman NJ. Reconstructive mucogingival surgery: the management of amalgam tattoo. Quintessence Int. 1988;19:489-492.
16. Kissel SO, Hanratty JJ. Periodontal treatment of an amalgam tattoo. Compend Contin Educ Dent. 2002;
23:930-936.
17. Griffin TJ, Banjar SA, Cheung WS. Reconstructive surgical management of an amalgam tattoo utilizing an acellular dermal matrix graft: case reports. Compend Contin Educ Dent. 2005;26:853-859.
18. Minsk L. Esthetic crown lengthening. Compend Contin Educ Dent. 2001;22:562-569.
19. Sonick M. Esthetic crown lengthening for maxillary anterior teeth. Compend Contin Educ Dent. 1997;18:807-819.
Acknowledgment
The authors wish to acknowledge Dr. Andrew Kurban, who was the restorative dentist involved in this case.
Dr. Griffin received both his DMD and his Certificate of Advanced Graduate Studies in Periodontology from Tufts University. He is a Diplomate of the American Board of Periodontology and is chair and director of postdoctoral periodontology at Tufts University School of Dental Medicine. He has published articles on periodontal plastic surgery and implantology in a variety of journals and has lectured nationally and in 19 foreign countries. He is a former president of the Massachusetts Periodontal Society. Dr. Griffin also maintains a practice in Boston limited to periodontology, implantology, and oral diagnosis. He can be reached at (617) 536-4545 or terrence.griffin@tufts.edu.
Dr. Engler-Hamm serves on the board of the Magazine Dentale Implantologie und Parodontologie as a consultant, and he has published several case reports in the field of periodontology and implant dentistry. At present, he is a third-year resident in the post-graduate periodontics program at Tufts University School of Dental Medicine. He is also the 2006 Lazzara Scholarship recipient from the American Academy of Periodontology Foundation. He can be reached at (617) 636-6531 or Daniel.Engler_Hamm@tufts.edu.
Dr. Cheung completed her residency in periodontics and earned a master’s of science degree from the graduate school of Tufts University. She is a Diplomate of the American Board of Periodontology and has authored articles on periodontal plastic surgery and implantology. She is currently an assistant professor in the Department of Periodontology, Tufts University School of Dental Medicine. She can be reached at (617) 636-6531 or wai.cheung@tufts.edu.
|
Continuing Education Test No. 83.1 |
After reading this article, the individual will learn:
• the crucial factors in making a diagnosis and case assessment in the aesthetic zone, and
• to identify incomplete passive eruption and amalgam tattoo lesions, and treatment modalities to correct these problems.
1. The reasons for excessive gingival display at smile could be ____.
a. skeletal, eg, associated with maxillary prognathism
b. a short upper lip
c. incomplete passive eruption (IPE)
d. all the above
2. Incomplete passive eruption (IPE) is a term used to describe the anatomical condition where the free gingival margin is located more than ____ coronal to the cementoenamel junction (CEJ).
a. 1 mm
b. 2 mm
c. 4 mm
d. 6 mm
3. Incomplete passive eruption (IPE) can be managed by ____.
a. making a longer crown
b. making a longer veneer
c. aesthetic crown lengthening
d. observing
4. Coslet, et al classified incomplete passive eruption (IPE) into 2 types according to ____.
a. hard-tissue relationship
b. length of the affected tooth
c. soft-tissue dimensions
d. thickness of the alveolar crest
5. Coslet, et al further divided incomplete passive eruption (IPE) into 2 subgroups
according to ____.
a. hard-tissue relationship
b. length of the affected tooth
c. soft-tissue dimension
d. thickness of the alveolar crest
6. Amalgam can be incorporated into the oral mucosa through ____.
a. condensation of the material into gingival tissue during the placement of amalgam restoration
b. damage to the gingiva by a cutting instrument during removal of an existing amalgam restoration
c. corrosion of retrograde amalgam restoration of endodontically treated teeth
d. all the above
7. Surgical approaches in the treatment of amalgam tattoo lesions include the use of ____.
a. free gingival autograft
b. subepithelial connective tissue graft
c. acellular dermal matrix allograft
d. all the above
8. In a case with multiple problems, ____ are crucial and should be accomplished very early in the sequence of appointments.
a. discussion and communication with the patient and restorative dentist
b. oral hygiene instruction, scaling, and root planing
c. discussion with the patient and oral hygiene instruction
d. communication with the restorative dentist and oral hygiene instruction to the patient
To submit Continuing Education answers, download the answer sheet in PDF format (click Download Now button below). Print the answer sheet, identify the article (this one is Test 83.1), place an X in the box corresponding to the answer you believe is correct, and mail to Dentistry Today Department of Continuing Education (complete address is on the answer sheet).










