INTRODUCTION
Porcelain veneers, fabricated from conventional feldspathic porcelain, are perhaps the most aesthetic restoration we can provide to our patients. Early papers by Calamia1,2 and Horn3 described porcelain veneers and mainly centered on no or minimal preparations. Friedman4 noted in a 15-year retrospective that 76% of porcelain veneer failures were fractures. In addition, adhesive failures were rarely observed when porcelain was bonded to etched enamel.
So, since minimally invasive dentistry is firmly ensconced in the mainstream of dentistry and bonding to enamel is generally acknowledged to be a prime factor in the success rate of veneers, the trend toward ultrathin (< 0.5 mm) veneers makes perfect sense.
CASE REPORT
Diagnosis and Treatment Planning
A 31-year-old patient presented to our office with a chief complaint of a fractured DIFL composite restoration on tooth No. 8 (Figure 1). However, teeth Nos. 8 and 9 had facial enamel defects, presumably as a result of indiscriminate orthodontic bracket removal. In addition, the patient was not pleased with the appearance of the 10-year-old lithium disilicate implant crowns on teeth Nos. 7 and 10 due to their unaesthetic length-to-width ratios (Figure 2).
The initial treatment consisted of repairing tooth No. 8. However, a more definitive treatment plan for teeth Nos. 7 to 10 was also proposed, including a diagnostic wax-up, followed by ultrathin veneers to be fabricated by our lab team using a recently introduced high translucency (HT) zirconia (KATANA [Kuraray Noritake Dental]). We discussed remaking the implant crowns on teeth Nos. 7 and 10, but the patient preferred the veneers since they were much more conservative and substantially less invasive.
 |
 |
| Figure 1. Maxillary central incisors preoperatively exhibited enamel defects in addition to a DIFL fracture of tooth No. 8. | Figure 2. The patient’s pre-op smile suffers from asymmetric central incisors and short, opaque implant crowns on lateral incisors. |
The first step was to have the dental laboratory team fabricate a diagnostic wax-up from which a template was used for an intraoral mockup made out of a provisional composite material (MirrorImage [Cosmedent]) (Figure 3). This mockup, which was fabricated over her existing dentition, showed the patient—in her own mouth—how her smile would be improved with the 4 new veneers. She then consented to the treatment plan, and the mockup was removed from her unmodified teeth.
Clinical Protocol
For the prep appointment, a new mockup was fabricated directly in the patient’s mouth to function as a preparation guide. Depth cuts for teeth Nos. 8 and 9 were made in the mockup, which was then removed. The depth grooves in the enamel guided the facial and incisal tooth reduction of teeth Nos. 8 and 9 (Figure 4). The initial plan for teeth Nos. 7 and 10 was no reduction at all, but due to proximal undercuts, minor reduction was also necessary for the crowns (Figure 5). The impression was done using a quality vinyl polysiloxane material (Aquasil Ultra+ [Dentsply Sirona Restorative]), and an accurate bite registration was taken using Futar D Fast (Kettenbach LP).
 |
 |
| Figure 3. The diagnostic wax-up was re-created in the patient’s mouth using provisional material. | Figure 4. Depth cuts were placed in the provisional material on tooth No. 8 and into the enamel of tooth No. 9 after removing the provisional material. |
 |
 |
| Figure 5. Completed preparations, teeth Nos. 7 to 10. | Figure 6. KATANA UTML (Kuraray Noritake Dental) high translucency zirconia veneers. |
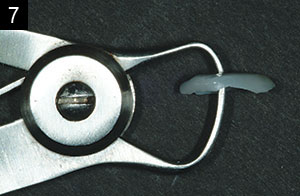
The completed 0.45-mm-thick veneers, milled from the KATANA UTML zirconia (Figure 6), were returned from the dental lab (Figures 7 and 8). The veneers for the natural central incisors were bonded simultaneously using Phil Bond (Dental Savings Club) in an etch-and-rinse technique on the enamel, while the intaglio surfaces of the veneers were sandblasted with 50-µm aluminum oxide using a MicroEtcher IIA (Zest Dental Solutions); rinsed; dried with air; primed with Clearfil Ceramic Primer Plus (Kuraray America); dried with air again; wetted with E-Bond (Zest Dental Solutions); and finally luted into place using a light-cured resin cement (Vitique [DMG America]), which was specially designed for efficient and exacting veneer placement. Each veneer for the lateral incisors was bonded one at a time. The soft tissue was covered with resin shield material (LC Block-Out Resin [Ultradent Products]) (Figure 9) while the adjacent tooth/veneer surfaces were protected by a Mylar strip (Figure 10). The prepped surface of each lithium disilicate crown was then sandblasted (Figures 11 and 12), followed by etching with hydrofluoric (HF) acid (Porcelain Etch [Ultradent Products]) (Figures 13 and 14). After thoroughly rinsing off the HF gel and air-drying, Clearfil Ceramic Primer Plus was applied to the ceramic surfaces and air-dried. E-Bond was again used as a wetting agent, and the veneers were bonded into place using Vitique.
At 18 months, the patient returned to the office for a routine veneer check. Despite the fact that the margins are visible at high magnification (Figures 15 to 17), we found that the veneers were functioning well, and the patient was still thrilled with her smile (Figure 18).
 |
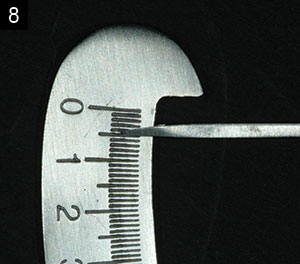 |
| Figures 7 and 8. The facial thickness of one veneer is measured to be 0.45 mm. |
 |
 |
| Figure 9. Resin shield material (LC Block-Out Resin [Ultradent Products]) was placed to protect the gingiva of tooth No. 7 before sandblasting. | Figure 10. A mylar strip was placed to protect teeth Nos. 6 and 8 from sandblasting. |
DISCUSSION
It is well known that the strength of feldspathic porcelain may be less than optimal for ultrathin versions of veneers. This is where HT zirconia may hold the promise of being both very aesthetic and strong. Kwon et al5 found the translucent zirconia included in their study to have a flexural strength of 688 MPa. This compares to 342 to 450 MPa for IPS e.max CAD5,6 and 143 MPa for feldspathic porcelain.7
 |
 |
| Figures 11 and 12. Tooth No. 7 was sandblasted (MicroEtcher IIA [Zest Dental Solutions]) to enhance micromechanical adhesion of the veneer to the crown. |
 |
 |
| Figure 13. The sandblasted surface of tooth No. 7 was etched with 9% hydrofluoric acid gel for 60 seconds. | Figure 14. The sandblasted and etched tooth No. 7 before application of the silane coupling agent (Clearfil Ceramic Primer Plus [Kuraray America]). |
 |
 |
 |
 |
| Figures 15 to 18. View at the 18-month followup. Even though the margins did not totally cover 100% of the visible tooth and crown surfaces, the patient was very satisfied by the appearance and function of the veneers. |
KATANA UTML (Kuraray Noritake Dental), the material used for this case, has the most translucency among the KATANA Zirconia series and is available in both standard and enamel shades. According to Kuraray Noritake Dental, KATANA UTML has 1.4 times more translucency than conventional zirconia. In addition, most commercially available zirconia materials are presumably fabricated from zirconia powder from one industrial source. However, Kuraray Noritake Dental uses its own powder, which is stated to provide more control over powder particle size, yttria concentration, binders, etc.
IN SUMMARY
This case illustrates that, under certain parameters, ultrathin zirconia such as KATANA can be used successfully for veneers. It also demonstrates that unaesthetic crowns can be veneered instead of being remade.
Acknowledgment:
The author thanks Jean Chiha of North Star Dental Lab in Irvine, Calif, for the excellent artistry in this case.
References
- Calamia JR. Etched porcelain facial veneers: a new treatment modality based on scientific and clinical evidence. N Y J Dent. 1983;53:255-259.
- Calamia JR. Etched porcelain veneers: the current state of the art. Quintessence Int. 1985;16:5-12.
- Horn HR. A new lamination: porcelain bonded to enamel. N Y State Dent J. 1983;49:401-403.
- Friedman MJ. A 15-year review of porcelain veneer failure—a clinician’s observations. Compend Contin Educ Dent. 1998;19:625-638.
- Kwon SJ, Lawson NC, McClaren EE, et al. Comparison of the mechanical properties of translucent zirconia and lithium disilicate. J Prosthet Dent. 2018;120:132-137.
- Leung BT, Tsoi JK, Matinlinna JP, et al. Comparison of mechanical properties of three machinable ceramics with an experimental fluorophlogopite glass ceramic. J Prosthet Dent. 2015;114:440-446.
- Venturini AB, Prochnow C, May LG, et al. Influence of hydrofluoric acid concentration on the flexural strength of a feldspathic ceramic. J Mech Behav Biomed Mater. 2015;48:241-248.
Dr. Miller received his DDS in 1974 from the University of Maryland and a GPR certificate from the Veterans Administration Hospital in Houston in 1975. In 1976, he opened a private practice in West Houston, and, in 2014, he joined the faculty at the University of Texas School of Dentistry in Houston as a clinical associate professor and director of the center for sports dentistry. Dr. Miller is a founding member of the American Academy of Cosmetic Dentistry (AACD) and created its highly acclaimed accreditation program. In 1986, he founded Reality Publishing Company, which is one of the leading non-commercial product evaluation testing sources in the world today. Dr. Miller is a Fellow of the AGD, an accredited member and Fellow of the AACD, and a member of the International Association of Dental Research. Dr. Miller has also lectured extensively nationally and internationally for more than 30 years. He can be reached at michael.b.miller@uth.tmc.edu.
Disclosure: Kuraray Noritake paid the lab fee for this case.
Related Articles
Delving Into Reality: A Conversation With Dr. Michael Miller
No-Preparation Porcelain Veneers
Correction of Extremely Dark Anterior Teeth











