In cases when patients present with severe tooth wear, it is incumbent upon the clinician to determine the etiology of the wear prior to initiating restorative treatment. The nature of a patient’s particular type of tooth wear could adversely affect the long-term success of any proposed restorative treatment plan. A systematic analysis and diagnosis of dental wear is essential to determining its etiologies, since there could be a mechanical cause, a chemical cause, or combination of causes.1
ATTRITION, ABRASION, AND EROSION
There are essentially 3 types of wear on teeth that clinicians may encounter: attrition, abrasion, and erosion.2 However, the literature repeatedly notes that wear mechanisms rarely occur alone, instead acting in combination with each other.2,3
Attrition is seen often in dentistry and is typically described as tooth-to-tooth wear caused either by bruxism, tooth grinding, or any condition in which the teeth actually wear down because they are rubbing against each other.2 Wear from attrition may appear in the mouth as flattened incisal and/or occlusal tooth surfaces that still accurately close together.3,4
Abrasion is tooth wear that’s usually caused by some external material or substance that actually wears the teeth (eg, abrasive dental paste, toothbrush).2 Abrasive wear is seen in a wide range of patients.5 It usually presents as lesions that are wider than they are deep, and these are located at the cervical areas of the teeth.4
Erosion involves the irreversible loss of dental hard tissue by chemical (eg, acid) breakdown, of which there are 2 types—intrinsic and extrinsic.2,4 It usually results in smooth lesions on the teeth that appear as cupped occlusal/incisal and concave buccal/lingual surfaces.3 Regardless of the origin, acid erosion has the potential to cause significant tooth wear.3
Extrinsic erosion is caused by something outside of the body, such as acidic fruit drinks, carbonated beverages, or a diet high in acidic substances.3 Intrinsic erosion is caused by stomach acids (eg, from forced vomiting in bulimia; acid reflux from gastroesophageal reflux disease [GERD]).3,6 According to one literature review, the prevalence of dental erosion in patients with GERD was 24%, with a large range (eg, 5% to 47.5%); the median prevalence of GERD in dental erosion adult patients was 32.5%, with a range of 21% to 83%.6 GERD and resulting dental erosion can also affect children.
It has been suggested that the severity of dental erosion is correlated with the presence of GERD symptoms.6 GERD can be described as the involuntary relaxation of the upper esophageal sphincter that allows refluxed acid to move up the esophagus into the mouth.7 Oral symptoms associated with GERD include, but are not limited to: burning mouth syndrome, tooth sensitivity, loss of vertical dimension, and aesthetic changes (eg, color, shape of teeth).4,7
When diagnosing erosion in particular, it is important for clinicians to differentiate between the 2 types (ie, intrinsic and extrinsic). The causative agents of the erosion must be removed and/or healed in order to ensure that no further damage to the tooth structure prior to initiating restorative treatment.4,7 This may require referring the patient to a gastroenterologist if GERD is suspected, or counseling the patient about abstaining from acidic foods or drinks if dietary causes are suspected. Then, depending on the extent of tooth wear, restorative treatment could vary from direct composite restorations to full-mouth reconstruction with metal-free or ceramometal restorations.4,7,8
Similarly, when tooth wear is due to attrition (eg, bruxism), such conditions could adversely affect the long-term success of treatment and might require a stronger type of restoration (eg, zirconium oxide or ceramometal) than if the tooth wear were caused by erosion alone. Such factors should be considered when treatment planning a patient.8 Furthermore, in cases where little (if any) enamel or dentin remains—even if the cause of wear is erosion—it might be more advisable to consider a full-crown preparation. This is because the ability to bond to enamel is very important when placing porcelain restorations.9,10 Enamel bonding has been shown to be predictable, effective, and long-lasting; bonding to dentin is also clinically viable, but only in the right circumstances.8,11
Of course, ceramometal and zirconia restorations can be conventionally cemented and successful luting procedures are not dependent on whether the preparation is in enamel or dentin.
 |
 |
|
Figure 1. Preoperative full-face photo of the patient with a natural smile. Note the short clinical crown length evident along the smile line due to wear. |
Figure 2. Close-up preoperative view of the natural smile. Note that the wear and discoloration are more clearly visible in this photo. |
 |
 |
|
Figure 3. Close-up preoperative retracted view of the patient’s teeth demonstrating the extent of wear of the maxillary teeth compared to the mandibular dentition. |
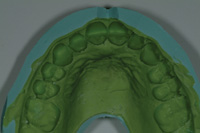
Figure 4. Preoperative occlusal view of the patient’s maxillary arch reveals the extent of lingual wear. |
Diagnosis and Treatment Planning
A medical history revealed that the patient had a history of treatment for GERD. Upon questioning, she stated being unaware of any nocturnal bruxism, nor had she ever been told that she was a bruxer. A clinical, periodontal, and radiographic examination was performed, after which it was determined that the patient was healthy and stable, with no joint problems, muscle soreness or tenderness, and her mandibular teeth showed little or no signs of wear/erosion. This point was significant, since no wear on the mandibular teeth confirmed that the maxillary wear was due to erosion and not attrition. Attrition would have resulted in wear to both arches.4 It is important to reiterate that identifying the etiology of the patient’s tooth wear—and confirming that it is under control—is significant to ensuring the long-term success of any proposed restorative treatment, since halting the disease process needs to be ensured; otherwise, the erosive process will continue to destroy tooth structure.12
Although it has become possible to restore eroded teeth in less invasive ways with the advent of composite materials and adhesive techniques, in cases of severe dental erosion, the placement of more extensive all-ceramic crown restorations may be required.12,13 In this case, a desirable treatment option was to place bonded pressed-ceramic restorations for teeth Nos. 3 to 14. This was discussed with the patient and subsequently accepted. The goals of treatment were to open the bite approximately 1.0 mm posteriorly in order to gain an estimated 3.0 mm of space in the anterior region. This would provide the space needed for aesthetically restoring the anterior teeth, while simultaneously enabling the development of anterior guidance and posterior disclusion within the patient’s envelope of function.10,14 It would also provide for: an increase in the size (display) of the teeth in order to expand the arch form posteriorly to correct the posterior crossbite while decreasing the negative space in the buccal corridors; a conservative restoration of the eroded lingual and occlusal surfaces: a whiter, brighter smile for the patient by utilizing the most aesthetic restorative materials available.
The restorative material selected for this case was a pressed-ceramic (IPS Empress Esthetic [Ivoclar Vivadent]). Such a material would provide the desired aesthetic results,9 particularly when waxed and pressed to full contour, then cut back and layered with a compatible aesthetic porcelain. When placed properly using adhesive bonding techniques, these materials are strong, predictable, and kind to the opposing natural dentition. When bonding to enamel, these materials also provide conservative tooth preparation options,15 requiring less tooth structure to be removed than with full crowns, thereby preserving some of the enamel on the facial surfaces. Furthermore, these materials allow the dental technician to fabricate full contour wax-ups on mounted casts, and to evaluate the occlusion before pressing. As a result, these porcelain materials have been increasingly used to develop anterior guidance, provided that sufficient tooth structure remains to support the bonded porcelain.10
 |
 |
|
Figure 5. Lingual view of the maxillary diagnostic wax-up that was created to achieve the objectives of the case. |
Figure 6. Facial view of the maxillary diagnostic wax-up. |
The laboratory was instructed to fabricate the diagnostic wax-up using 11.0 mm as the final length of the central incisors.
The diagnostic wax-up would also establish the new anterior guidance, as well as the aesthetic and functional requirements of the case.14 The diagnostic wax-up would give the dentist, the dental ceramist, and the patient the ability to identify any potential obstacles that could affect the definitive results.17 The putty matrix of the wax-up would be used to transfer this information to the mouth in the form of the provisional restorations. The provisional restorations would then be used by the patient to evaluate the proposed treatment; in terms of the goals for smile and bite alterations, as well as serve as a blueprint for the laboratory when constructing the definitive restorations.
 |
 |
|
Figure 7. The prepared maxillary teeth. |
Figure 8. A face-bow transfer (Artex [Jensen industries]) was done. |
 |
 |
|
Figure 9. A silicone putty (Siltech [Ivoclar Vivadent]) matrix was created for use in fabricating the provisional restorations. |
Figure 10. View of the putty matrix after the provisional material was injected. |
 |
 |
|
Figure 11. Retracted view of the provisional restorations immediately following placement. |
Figure 12. A model of the impressions was used in the dental laboratory for fabricating the pressed ceramic restorations as prescribed. |
Following tooth preparation and a full-arch polyether impression (Impregum Soft [3M ESPE]), a new face-bow transfer (Artex, Jensen Industries) (Figure 8) and CR bite was taken, In addition, a stick bite for horizontal reference, a dentin (“stump”) shade of the prepared teeth, and photographs of the preparations were done. The provisional restorations were fabricated utilizing the putty matrix (Sil-Tech [Ivoclar Vivadent]) (Figure 9) that was fabricated using the diagnostic wax-up. The temporary material (Luxatemp Shade BL [Zenith DMG]) was injected into the matrix (Figure 10) to create the provisionals. Next, the margins were finished, the gingival embrasures opened, and the occlusion adjusted. Finally, the provisional restorations were polished (Figure 11).
Provisional restorations are very important for both doctor-patient and doctor-dental technician communication. In cases such as this, provisional restorations are critical to success because they help determine many aspects of the final restorations (Figure 12). This includes such things as incisal edge position, anterior guidance, overbite, overjet, occlusal relationships, and proper width in the buccal corridors.
Ultimately, well-done provisionals enable the patient to “try-out” and “adapt” to the changes in their new smile and teeth.16 The patient can go through phonetic exercises to ensure that speech is not affected by the new length, and valuable feedback about the appearance and color of their teeth can be obtained. In cases such as this when the bite is altered, it is important to evaluate the patient aesthetically, functionally, and phonetically at a postoperative appointment when the patient is not numb. This is an ideal time to assess and fully establish patient comfort, function, and satisfaction. It allows one to communicate any necessary changes or modifications to the dental laboratory team. In this particular case, minor occlusal adjustments were made. An impression and photographs of the provisionals were then taken and forwarded to the laboratory. The patient remained in provisionals for 4 weeks, during which time she experienced no problems and expressed satisfaction with the appearance and color of her new smile.
 |
 |
|
Figure 13. Occlusal view of the maxillary pressed ceramic restorations (IPS Empress [Ivoclar Vivadent]) on the model. |
Figure 14. Close-up postoperative retracted view of the patient’s maxillary teeth. Note the enhanced arch form, and the overall aesthetics and proportion of the dentition compared to Figure 3. |
 |
 |
|
Figure 15. Retracted postoperative right-lateral view of the restorations. |
Figure 16. Retracted postoperative left-lateral view of the restorations. |
Next, a rubber dam was placed and the restorations were cleaned with a chlorhexidine scrub (Consepsis [Ultradent Products]). Subsequently, the teeth were etched with phosphoric acid gel for 10 seconds and thoroughly rinsed. Multiple coats of a fifth generation bonding agent (Prime & Bond NT [DENTSPLY Caulk]) was applied, lightly air-dried, and then light-cured for 10 seconds per tooth.
A light-cured luting cement (Variolink Veneer [Ivoclar Vivadent]) (shade +1) was placed on the internal surface of the restorations, and the restorations were then seated into place. Excess cement was cleaned from the facial and lingual surfaces with cotton rolls and brushes. The restorations were then tacked into place at the gingival margin using a 3-mm curing light tacking tip for 5 seconds per tooth. Excess cement was then removed interproximally with dental floss, followed by light-curing (one minute each from the facial and lingual surfaces) with an LED curing light (Bluephase 16i [Ivoclar Vivadent]).
The rubber dam was then removed, and the occlusion was verified. Finally, the restorations were polished using rubber points (Ceramisté [Shofu]) and polishing paste (Porcelize [Cosmedent]) on a felt wheel.
The patient was seen briefly the next day and then one week later. Occlusal adjustments were made and the restorations were evaluated for aesthetics, function, and phonetics. The patient said that she had experienced very minimal discomfort, no problems chewing or speaking, and was very happy with the feel of her teeth and the appearance of her smile.
 |
 |
|
Figure 17. Close-up postoperative view of the patient’s natural smile. Note the enhanced length and dimensions of the teeth after restoration of the clinical crown form. |
Figure 18. Final postoperative full-face view of the patient’s natural smile. Note the enhanced smile aesthetics and proportions. |
However, equally significant is the diagnostic process. In cases involving tooth wear, determining the correct cause(s) and nature of the wear is vital. Doing so enables the clinician to properly treatment plan the case and to select and utilize the most appropriate and predictable restorative materials to ensure long-term aesthetic and functional success. In this case, all of the patient’s and clinician’s goals were met using a pressed-ceramic material and fabricating the restorations according to the diagnostic wax-up (Figures 17 and 18) formulated from the diagnosis and treatment plan.
Acknowledgement
The author wishes to acknowledge Frontier Dental Laboratory in El Dorado Hills, Calif, for creating the ceramic restorations featured in this article.
References
- Verrett RG. Analyzing the etiology of an extremely worn dentition. J Prosthodont. 2001;10:224-233.
- Addy M, Shellis RP. Interaction between attrition, abrasion and erosion in tooth wear. Monogr Oral Sci. 2006;20:17-31.
- Bartlett DW. The role of erosion in tooth wear: aetiology, prevention and management. Int Dent J. 2005;55(4 suppl 1):277-284.
- Gandara BK, Truelove EL. Diagnosis and management of dental erosion. J Contemp Dent Pract. 1999;1:16-23.
- Barbour ME, Rees GD. The role of erosion, abrasion and attrition in tooth wear. J Clin Dent. 2006;17:88-93.
- Pace F, Pallotta S, Tonini M, et al. Systematic review: gastrooesopha-geal reflux disease and dental lesions. Aliment Pharmacol Ther. 2008;27:1179-1186.
- Ali DA, Brown RS, Rodriguez LO, et al. Dental erosion caused by silent gastroesophageal reflux disease. J Am Dent Assoc. 2002;133:734-737.
- Griffin JD Jr. Anterior CEREC CAD/CAM porcelain treatment of GERD eroded teeth. Contemp Esthet. 2006;10:32-39.
- Christensen GJ. A void in U.S. restorative dentistry. J Am Dent Assoc. 1995;126:244-247.
- Cho GC, Donovan TE, Chee WW. Clinical experiences with bonded porcelain laminate veneers. J Calif Dent Assoc. 1998;26:121-127.
- Sundaram G, Bartlett D, Watson T. Bonding to and protecting worn palatal surfaces of teeth with dentine bonding agents. J Oral Rehabil. 2004;31:505-509.
- Jaeggi T, Gruninger A, Lussi A. Restorative therapy of erosion. Monogr Oral Sci. 2006;20:200-214.
- Yip KH, Smales RJ, Kaidonis JA. Case report: management of tooth tissue loss from intrinsic acid erosion. Eur J Prosthodont Restor Dent. 2003;11:101-106.
- McIntyre F. Restoring esthetics and anterior guidance in worn anterior teeth. A conservative multidisciplinary approach. J Am Dent Assoc. 2000;131:1279-1283.
- Hastings JH. Conservative restoration of function and aesthetics in a bulimic patient: a case report. Pract Periodontics Aesthet Dent. 1996; 8:729-736.
- Achieving predictable, beautiful smiles using a dento-facial esthetic diagnosis system. Compend Contin Educ Dent. 2007;28:50-55.
- Garcia LT, Bohnenkamp DM. The use of diagnostic wax-ups in treatment planning. Compend Contin Educ Dent. 2003;24:210-214.
- Magne P, Belser UC. Novel porcelain laminate preparation approach driven by a diagnostic mock-up. J Esthet Restor Dent. 2004;16:7-16.
- Magne P, Magne M. Use of additive waxup and direct intraoral mock-up for enamel preservation with porcelain laminate veneers. Eur J Esthet Dent. 2006;1:10-19.
Dr. Dudney is a 1977 graduate of University of Alabama in Birmingham School of Dentistry. He has served as the clinical director for the Aesthetic Advantage hands-on programs taught by Dr. Larry Rosenthal at New York University and the Eastman Dental Clinic in London. He is presently the program director for the California Center for Advanced Dental Studies programs taught in the United States and the United Kingdom. In addition to teaching and lecturing, Dr. Dudney has authored several articles on aesthetic dentistry. He maintains a private practice with an emphasis on aesthetic and restorative dentistry in Birmingham, Alabama. He can be reached at (205) 663-6545 or by e-mail at tedudneydmd@aol.com.
Disclosure: Dr. Dudney reports no conflict of interest.











