
Dental zirconia has gained wide popularity in the dental market, causing many clinicians to inquire about the best cementation techniques for zirconia restorations. The following issues can be critically important when selecting cement for zirconia restorations:
1. You’re Not Sure What Type of Zirconia Your Dental Lab Used
There are different types of zirconia available in the market, including zirconia with (1) lithium disilicate-like translucency (KATANA UTML) and the flexural strength of approximately 550 to 600 MPa, (2) conventional strength and more than 1,000 MPa with high flexural strength and low translucency (KATANA HT, etc), and (3) intermediate strength of approximately 750 to 800 MPa and high translucency (KATANA STML, etc). These materials have different mechanical properties which may influence bonding procedures.
Conventional high-strength-type zirconia has shown long-term clinical success cementing resin-modified glass ionomers. Recent research has reported, however, that the resin cements should be used for translucent zirconia materials because of their comparatively lower mechanical strength compared to conventional high-strength materials (eg, Original 10-MDP-based PANAVIA V5, PANAVIA SA Cement Plus). Furthermore, one recent research study (poster presented at 2017 IADR/AADR/CADR General Session, March 24, 2017, presentation ID: 2002) shows that sandblasting high-translucent zirconia can weaken the material in a bonded restoration. If you are not sure what type of zirconia your dental lab used, adhering to bonding protocol with your routine sandblasting technique may help to produce a predictable outcome.
 |
 |
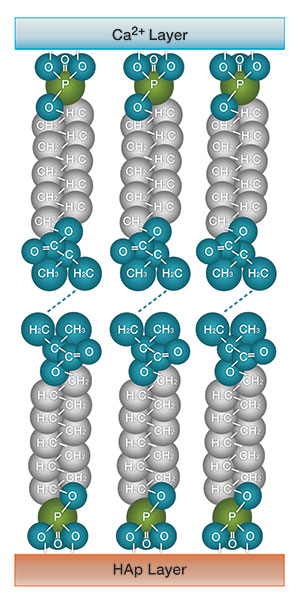
| Figure 1. Considered the most important monomer, 10-MDP forms a chemically stable bond to hydroxyapatite. This schematic diagram shows the bond between a 10-MDP monomer and tooth substrate (hydroxyapatite). | Figure 2. A schematic diagram showing a 10-MDP monomer chemically bonding to zirconia. |
2. Ensuring Better Margins
Good marginal fit of prosthetic crowns is an essential requirement to achieve a durable restoration. Despite all technological advances, obtaining an effective, long-lasting marginal seal at the tooth-crown interface still can be a great challenge. Marginal fit discrepancy can cause clinical problems. The technique used when manufacturing crowns using CAD/CAM may also influence the marginal gap compared to conventional cast crowns. In several studies (eg, Acta Biomater. 2011;7:3187-3195), MDP-based adhesive restorations showed durable bonding to hydroxyapatite (Figure 1). 10-MDP has been shown to adhere very well to zirconia (Figure 2). An MDP-based resin cement, such as PANAVIA V5 and PANAVIA SA Cement Plus, would be a good option to achieve a successful clinical outcome.
3. Major Improvements in Resin Cements Have Made Them So Easy to Use
Many clinicians liked glass ionomer-type cements due to their user-friendly features, such as no pre-treatment steps and easy excess removal. In the past, resin cements like PANAVIA F 2.0 required that clinicians mix primers and caused a difficult removal of excess cement. Currently, we have cements like PANAVIA V5, which is easy to use and offers the ability to easily remove excess cement with tack-curing. Most clinicians prefer the cost effectiveness of zirconia and its ease of cementation. With recent advancements in resin cements, PANAVIA V5 can be a good choice of cement for zirconia crowns.
Using 10-MDP-based resin cement can be a key factor in the reliable adhesive cementation of zirconia restorations.
For more information, call Kuraray America at (800) 879-1676 or visit kuraraydental.com.












