INTRODUCTION
The use of implants in the edentulous patient is intended as an adjunctive means to improve retention of prosthesis. In many instances, in an effort to help the patient, the dentist may choose to focus on placement of implants utilizing the patient’s existing prosthesis, possibly in an effort to assist a patient financially. In this scenario, the patient’s concerns may divert the focus on finding a means to increase retention of ill-fitting prostheses versus evaluation of the quality of prostheses prior to implant placement. Evaluation of existing prostheses can reveal that problems may lie in the quality of what exists, and if treatment is continued without considering the physiologic-functioning of the patient, then the existing prosthesis may direct less optimal implant placement which could compromise both aesthetic and functional results.
Edentulism can be considered a form of disability that includes problems with self-esteem, speech, inefficient mastication, and persistent discomfort of the supporting soft and hard tissues. When a patient presents for treatment and the diagnosis is edentulism, the Prosthodontic Diagnostic Index (PDI)1 classification helps the dentist understand the degree of difficulty when evaluating the patient for prosthodontic rehabilitation.
CASE REPORT
 |
| Frontal views of the patient as shown, with the pretreatment photo on the left and the postoperative photo on the right. |
 |
 |
|
Figure 1. The intraoral view of the maxillary and mandibular dentures, with the patient in maximum intercuspation. |
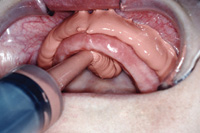
Figure 2. Intraoral view showing the residual anatomy of the patient’s right side of the mandible. Note the spiny ridge. |
 |
 |
|
Figure 3. Intraoral view showing the residual anatomy of the patient’s left side of the mandible with high frenum attachment relative to the height of the residual ridge. |
Figure 4. The mandibular master cast demonstrates excessive residual ridge atrophy. This contributed to a lack of stability for the patient’s mandibular complete denture. |
 |
|
Figure 5. The panoramic radiograph shows demarcation lines anterior to the mental foramina, demonstrating the anatomic limits to placement of implants without concern of bilateral impingement on the inferior alveolar nerve. |
A 80-year-old male presented to the practice for a comprehensive examination. He presented with existing maxillary and mandibular complete dentures. The mandibular prosthesis was unstable and food particles migrated under and around the prosthesis. The patient had seen several dentists prior to seeking additional care and was told he had insufficient bone structure for placement of implants.
Pretreatment conditions showed (Before image) there was a lack of adequate buccal corridor space bilaterally with the existing dentures. The view of the patient in maximum intercuspation with the prostheses in position (Figure 1) also demonstrated a worn denture dentition. The patient’s chief complaint was focused on his perception that the dentures “felt full but not natural.” The residual mandible (Figures 2 to 5) exhibited severe atrophy of the bone, residual spiny ridge, and high frenum attachments relative to the height of the residual alveolar bone. Additionally, the tissue character demonstrated thin mucosa overlying the residual ridge, highly mobile in a facial-lingual direction with mobility in excess of 2 mm.
Technique
The trial denture fabrication2 followed clinical prosthodontic techniques including: the layering method for the final functional impression procedures; evaluation of the occlusal vertical dimension; utilizing the exhaustive approach to obtain a repeatable resting position and factor in closest speaking space; and registration of the centric relation records using the jaw relation recorder which allows the patient to generate a gothic arch tracing, while allowing the patient’s muscles of mastication to deprogram from the positions used from wearing the worn older prostheses with inadequate occlusal vertical dimension. Most importantly, identifying the functional tooth position following the neutral zone technique principles3 allows the capture of functional muscle actions during swallowing, speaking, and mastication. The dentist will place softened impression compound (modeling plastic) attached to the acrylic record base similar to wax formed on the occlusion rim and record base. The patient is then asked to swallow while drinking warm water. This action will allow the muscles to shape the softened compound rim and identifying the functional location of the anterior and posterior teeth in facial and lingual positions. This procedure will allow any prosthesis to be designed in a neutral space thereby reducing unwanted movement. The “neutral zone” technique is an important procedure that allows the clinician to determine the mandibular anterior and posterior denture tooth positions.
 |
 |
| Figure 6. Wax trial dentures shown on mounted master casts. This view the occlusal scheme is a reverse occlusion (crossbite), determined by the physiologic method in fabrication of dentures, using the neutral zone record base. |
Figure 7. The intaglio surface of the mandibular trial denture shows the metal framework embedded within the resin record base. |
 |
 |
|
Figure 8. The occlusal and intaglio views of the processed mandibular denture demonstrating that the intaglio surface has been relieved generously. By incorporating a mandibular frame, the strength of the prosthesis is preserved, even after extensive relief over the implant positions. |
Figure 9. Following the technique of making cameo surface impressions that capture functional movements on the buccal/facial and lingual surfaces, the metal framework is not visible since there is adequate thickness of resin on all surfaces of the mandibular denture. |
 |
 |
|
Figure 10. The panoramic radiograph demonstrates the positions of the micro implants on the day of insertion. |
Figure 11. The jaw relation index is made with the patient in their centric relation position using a VPS (Regisil Rigid Registration Material [DENTSPLY Caulk]). The index is used to help replicate and guide the patient into position intraorally. The view shows the index prior to trimming. |
After following the fabrication technique (Figure 6), the resulting occlusal scheme for this patient is in reverse occlusion (crossbite). The concept of “engineering” the prosthesis for specific treatment includes fabrication of a cast metal framework4 for the mandibular trial denture that defined the facial, lingual, and distal limits of implant placement (Figure 7). Another indication for incorporating the metal framework is to add strength to the prosthesis since the intaglio surface may need to be relieved when attachments are incorporated for retention.
When there is an attempt to work with ill-fitting prostheses versus fabrication of new prostheses, the previous prosthesis may have many features that are incorrect for the patient such as the centric relation position, aesthetic positioning of the denture teeth, and inappropriate occlusal vertical dimension, to name a few. The dentist should avoid using the existing dentures when treatment planning placement of implants. Correct implant placement for a new implant-retained mandibular overdenture requires “engineering” the positions of the implants to best support the prosthesis, rather than using the existing denture to determine the position of the implants. New dentures should be fabricated incorporating a metal framework in the mandibular overdenture to support the placement of implants based on anatomical and functional limitations.
After fabrication of the mandibular overdenture, the intaglio surface over the area of the implants can be relieved excessively for pick-up of implant attachments knowing that the mandibular metal framework is incorporated for strength (Figures 8 and 9). The panoramic radiograph shows the positions of the mandibular one-piece implants (3.25 mm diameter, ERA Mini Dental Implant [Sterngold Dental]) (Figure 10). The implants have been placed in the mandibular anterior area bound by the mental foramina.5 In order to complete the pick-up procedure of the implant locations as accurately as possible, the dentures are placed intraorally and markings on the denture reflect the patient’s mandibular position in centric relation occlusion. An occlusal index is made to replicate the centric relation position. This occlusal index is placed intraorally and the patient is asked to close into the index, replicating centric relation position with assurance, regardless of the influence when using anaesthetic or if the patient lacks sufficient coordination to repeat the position reliably during the various dental procedures (Figure 11).
 |
 |
|
Figure 12. The micro implant is shown being surgically placed in the patient’s mandibular anterior left area. |
Figure 13. View of the intaglio surface of the mandibular denture after intraoral pick-up of the attachments; the metal housings are shown with the black processing caps. Note the proximity of adjacent metal housing to the metal framework allowing relief of the resin. |
 |
 |
|
Figure 14. This photo shows the difference in diameter measurements between the standard ERA metal housing and the micro attachment housing. |
Figure 15. The tool is used to remove the black processing caps and the least retentive elements are placed into the housings as shown. |
 |
 |
|
Figure 16. At the 3-month post-treatment appointment, plaque is evident demonstrating a lack of proper oral hygiene maintenance of the implants. Also note the height difference between implants. This cannot be altered since these are one-piece implants after surgical placement. |
Figure 17. After reinforcement of patient hygiene instruction and care, the implants can be maintained long-term. The overlaying schematic shows the Oral-B Triumph with Floss Action Head (Procter & Gamble) that patients use to help maintain the implant overdenture abutments. |
The 3.25-mm diameter implant is placed where bone is available in the mandible since it was decided mutually between the dentist and the patient that there would not be additional adjunctive surgical intervention such as bone grafts to accommodate standard size implants (Figure 12). The processing caps are shown in the mandibular denture (Figure 13). The use of the mandibular frame allows the dentist to relieve the intaglio surface of the mandibular denture while maintaining the integrity and strength of the denture.
As shown in Figure 14, the occlusal diameter is measured at 4.4 mm. This allows 1.0 mm of potential clearance space, as compared to use of the standard diameter attachment of 5.5 mm, typically used with the ERA housing. The tool is utilized to remove the processing caps and place the retentive elements within the metal housings in the mandibular prosthesis (Figure 15). The white-colored elements represent the least amount of retentive force.
The post-treatment frontal view of the patient demonstrates improved aesthetic results, including restoration of the buccal corridors bilaterally. (Figure 16) The use of one-piece implants requires careful planning in selection of the appropriate collar height at time of surgical placement. A limitation of the one-piece implant is the collar height since the transmucosal/transgingival element cannot be interchanged. The implant positions were determined solely by the residual bone and did not require adjunctive grafting procedures.
As with any dental procedure, the patient must be on a hygiene maintenance protocol, since the reason for tooth loss may have been directly related to inadequate hygiene maintenance of the natural teeth as a contributing factor (Figure 17 and After Image). The patient emphasized that “he couldn’t even tell they (the dentures) were there (in his mouth).”
DISCUSSION AND SUMMARY
The technique presented shows how important it is to focus on the prosthetically driven treatment plan to balance the needs of the patient. In many instances, the patient’s chief complaint is important to the outcome. However, evaluation of the existing prosthesis should be a part of the comprehensive examination procedure as you plan to place implants that will be used to assist in retention. By incorporating and engineering prosthetic components, such as the metal framework embedded in the mandibular overdenture, the integrity and strength of the prosthesis are maintained even when it is necessary to relieve areas to accommodate attachment housings.
Key to the patient treatment is following predictable and critical fabrication techniques that create a final prosthesis that meets aesthetic desires and is a physiologically functional prosthesis. The outcome is reflected in the patient’s statement that “I no longer get food under the dentures,” “they fit snug and tight,” and “they fit so well that you don’t realize you even have them in your mouth.”
References
- McGarry TJ, Nimmo A, Skiba JF, et al. Classification system for complete edentulism. The American College of Prosthodontics. J Prosthodont. 1999;8:27-39.
- Massad J, Lobel W, Garcia LT, et al. Building the edentulous impression—a layering technique using multiple viscosities of impression material. Compend Contin Educ Dent. 2006;27:446-451.
- Beresin VE, Schiesser FJ. The neutral zone in complete dentures. J Prosthet Dent. 1976;36:356-367.
- Rodrigues AH. Metal reinforcement for implant-supported mandibular overdentures. J Prosthet Dent. 2000;83:511-513.
- Doundoulakis JH, Eckert SE, Lindquist CC, et al. The implant-supported overdenture as an alternative to the complete mandibular denture. J Am Dent Assoc. 2003;134:1455-1458.
Dr. Massad is adjunct associate faculty, Tufts University School of Dental Medicine, and adjunct associate faculty, Department of Prosthodontics, University of Texas Health Science Center, San Antonio. He is the director of removable prosthodontics at the Scottsdale Center for Dentistry. He has published articles in the Journal of Prosthetic Dentistry, International Journal of Periodontal and Restorative Dentistry, Compendium of Continuing Dental Education, The Independent Journal England, The Pankey Gram, Bulletin of American Association of Dental Examiners, Journal of the Oklahoma Dental Association, Dentistry Today, Dental Economics, and others. He can be reached at (918) 749-5600 or joe@joemassad.com.
Disclosure: Dr. Massad was and is an independent paid consultant for many dental companies, such as Harry J. Bosworth, Ivoclar USA and Europe, DENTSPLY Trubyte, Chattem Consumer Products, Laclede Professional Products, Brassler USA, Simplified Notes Company, Proctor and Gamble, Austenal, Inc, and GC America.
Dr. Bohnenkamp is director of the International Dentist Education Program at the University of Texas Health Science Center Dental School in San Antonio. He is the author of numerous manuscripts published in referred dental journals and has served on the editorial review board of the Journal of Prosthetic Dentistry. He is currently authoring a chapter “Clinical Patient Scenarios” for a work entitled Osseointegration and Occlusal Rehabilitation and Removable Partial Dentures—A Clinical Guide. He can be reached at bohnenkamp@uthscsa.edu.
Disclosure: Dr. Bohnenkamp reports no conflict of interest.
Dr. Garcia is professor and chair of the Department of Prosthodontics at the University of Texas Health Science Center San Antonio. She received her DDS from Baylor College of Dentistry and her Certificate and MS degree from the University of Texas Health Science Center San Antonio. She is a Diplomate of the American Board of Prosthodontics and Fellow of the American College of Prosthodontists. She has published numerous articles and abstracts, edited several dental textbooks, has served as a reviewer and editorial board member for several scientific journals, and co-authored the text Osseointegration and Occlusal Rehabilitation and Removable Partial Dentures–A Clinician’s Guide. (The latter is in press.) She maintains a practice limited to prosthodontics. She can be reached at GARCIALT@uthscsa.edu.
Disclosure: Dr. Garcia reports no conflict of interest.