Until now it has been difficult to determine which abnormal tissues in the mouth are a cause for concern. In the United States it is estimated that there were 29,370 new cases of oral cancer and 7,320 related deaths in 2005.1 The disease morbidity is directly related to the cancer stage at the time of diagnosis. Consequently, early detection impacts disease mortality and facilitates minimally invasive treatment procedures. Oral squamous cell carcinoma (SCC) is believed to progress from oral premalignant lesions (OPLs) to hyperplasia, increasing dysplasia (mild, moderate, and severe) into carcinoma in situ (CIS), and finally to invasive SCC (from stage I to IV). Unfortunately, the 5-year survival has remained very poor, with little improvement over the last 30 years (<50%), mainly because a significant proportion of these cancers are still diagnosed late (stage III and IV).2
The American Dental Association states that 60% of the US population sees a dentist every year. This obviously provides a potential to include cancer screenings and detection of oral cancer in its early stages. Unfortunately, published studies indicate that currently less than 15% of those who visit a dentist regularly report having had an oral cancer screening. It is now commonplace for women to get an annual PAP smear for cervical cancer or a mammogram to check for breast cancer. In addition, many men at risk receive an annual prostate-specific antigen (PSA) test and digital rectal exam for prostate cancer. These screening efforts have been possible due to public awareness of the value of catching cancers in their earliest forms as well as effective technologies for conducting the examinations. Oral cancer is not different in this regard. In fact, it is potentially easier to obtain patient compliance because unlike many other cancer screening procedures, there is no invasive technique necessary, no discomfort or pain involved, and it can be very cost-effective. Consequently, our dental examinations, when they are properly performed and include screening for oral cancer, will save lives.
There has been a tendency to check these lesions over an extended period of time, which may allow a SCC to grow into later-stage disease, with consequent poorer prognosis and increased morbidity. Therefore, there are 2 separate issues: detection and diagnosis. Detection is the result of thorough visual and manual examinations of all soft tissues of the mouth. This includes manual extension of the tongue to examine its base, a bimanual palpation of the floor of the mouth, and digital examination of the borders of the tongue and the lymph nodes surrounding the oral cavity and in the neck. New detection aids, including lights, dyes, and other techniques have appeared in the marketplace.
LED Medical Diagnostics (LED MD) is a Vancouver-based medical company that has developed an imaging device to assist dentists in screening for early tissue changes (OPLs) that can lead to cancer. In association with scientists at the British Columbia Cancer Agency (BCCA), LED MD jointly developed the VELscope (Figure 1). The VELscope integrates 4 key elements: illumination, sophisticated filtering, natural tissue fluorophores, and the power of human optical and neural physiology. The VELscope has the potential to overcome many of the obstacles presented by conventional methods for screening and aid in the detection of mucosal abnormalities including premalignant and malignant lesions. The VELscope illuminates tissue with specific wavelengths that interact with and provide metabolic and biochemical information about the cells at and just beneath the surface. This gives clinicians the ability to see early biochemical changes before they present more obviously, and therefore detect lesions earlier in the disease process. Using history as the gold standard, the device achieved a sensitivity at 98% and specificity of 100% when discriminating normal tissue from severe dysplasia/CIS or invasive carcinoma, according to the BCCA.
This cost-effective, easy-to-use, direct imaging approach allows the dentist, hygienist, and healthcare providers to find lesions that may be hard to see with normal white light, thus improving the quality of care they give to their patients. When the VELscope is used during routine dental examinations, cancer screens can be provided in an efficient way (Figure 2). The procedure takes from 2 to 4 minutes, which makes it easy to incorporate into the usual office protocols (Figures 3 to 6).
CASE REPORTS
 |
 |
|
Figure 1. The VELscope unit. |
Figure 2. VELscope in clinical use. |
 |
 |
| Figure 3. Image of normal tongue. (Figures 3 to 6 courtesy of the British Columbia Cancer Agency.) |
Figure 4. Normal tongue as it appears under the VELscope. |
 |
 |
|
Figure 5. Area appearing normal under white light. |
Figure 6. Figure 5 as seen under the VELscope. Dark area is VEL-scope-positive, which was confirmed by biopsy as carcinoma in situ. |
The department of Oral Medicine at the University of Washington has, for the past several years, conducted an Oral Dysplasia Clinic that is housed within the Head and Neck Cancer Clinic at the University of Washington Medical Center. It is a regional center that accepts referrals from a 5-state region. The Oral Dysplasia Clinic receives referrals from physicians and dentists treating patients with oral lesions that have or appear to have potential for progression into SCC. The purpose of the clinic is to manage such patients and to follow them periodically to determine if mucosal changes have undergone transformation to aggressive or malignant disease.
The task of periodic evaluation of patients with atypical oral mucosal changes with potential for malignant transformation is difficult and requires judgment calls about the nature of the lesions under observation. Failure to identify malignant transformation effectively can result in a significantly more risky or severe prognosis. Making decisions about whether a lesion represents significant health risk is best described as “making decisions in the presence of uncertainty.” Such situations call for improved methods to assess lesions so that clinical decisions have the highest probability for correctness.
For the past 2 years we have been fortunate to have had access to a prototype VEL-scope unit, and for the past 4 months we have used the newest version of the scope in our clinic. The VELscope has been very helpful in improving our assessment of patients with chronic oral tissue changes and in deciding whether the tissue changes observed using visual inspection are valid or understate the risk of malignant disease. The scope does not ensure that all clinical decisions regarding potentially malignant oral lesions are correct, but it has resulted in diagnoses of malignant disease or very aggressive dysplasia in a number of cases that would have otherwise been judged clinically as negative for dangerous change. Among these cases, 4 specifically come to mind that illustrate the value of the VELscope in the assessment and follow-up of patients who present with oral lesions.
Case No. 1
A 48-year-old female with no history of tobacco use or other risk factors associated with oral cancer presented to the Oral Dysplasia Clinic upon referral from her head and neck cancer specialist. She had undergone excision of a 4×8-mm inflamed lesion on the right lateral aspect of the tongue that was found microscopically to exhibit moderate to severe dysplasia with carcinoma in situ. At the time of referral she was free of any visually detectable lesion of the oral mucosa. She was seen at 2 follow-up visits 3 months apart, and the tissues of the mouth and tongue remained free of visual changes. At the second follow-up visit she reported mild discomfort in the region of the original lesion excision, and it was thought that her symptom might be a residual neurological effect from the surgery. Clinical inspection failed to identify any tissue change, but careful examination of the right lateral border of the tongue using the VELscope demonstrated a 2×4-mm region of intense light absorption, with the visual appearance of deep purple indicating possible dysplastic or malignant cells.
The cancer surgeon was called to the clinic to observe the region of VELscope-positive tissue change. We recommended biopsy with removal of the area of light absorption along with adequate margins. The biopsy specimen again showed severe oral dysplasia with an area of carcinoma in situ with clear margins. All of the clinical experts who observed the area agreed that had the scope not provided a positive finding, the area would not have been considered for removal, and her symptoms would have been attributed to postsurgical neurological damage. Her lack of prior risk factors for oral cancer and the absence of a definitive clinical lesion caused us to put dysplasia or carcinoma lower on our list than would otherwise have occurred. The positive findings with VELscope assessment resulted in a decision to biopsy, resulting in discovery of aggressive tissue changes months before they would have become clinically obvious.
Case No. 2
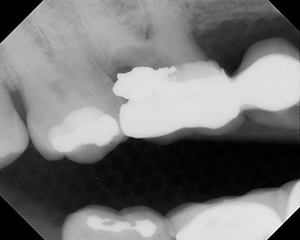
A 62-year-old male with a history of alcohol abuse and heavy use of tobacco for 30 years presented for follow-up of oral lesions on the right posterior of the tongue. Prior biopsy had detected the presence of moderate dysplasia. The patient was followed clinically over a 9-month period at 3 month intervals using very careful visual inspection of the region of prior cellular change. The tissues were palpated, and the patient was cautioned to return earlier than the routine recall date if he noted any tissue change or other symptoms. Clinical inspection of the tongue at each recall visit demonstrated faint leukoplakia that was unchanged in visual appearance or palpation. At the third visit the VELscope examination revealed a 3×4-mm region of dense light absorption in a zone behind the region of leukoplakia. The area was normal to visual inspection using an examination light, and palpation failed to find tactile changes suggestive of thickening of the tissue.
The head and neck surgeon who referred him to the Oral Dysplasia Clinic was informed of the finding and came to the clinic to use the scope to determine the exact region that was VELscope-positive. That area was removed with wide margins, and microscopic examination demonstrated carcinoma with clear margins that did show mild cellular atypia in one region. Use of the scope allowed identification of a region of malignant transformation that was distant from the original site of change and not in the area of leukoplakia that was under close observation.
Case No. 3
A 55-year-old female with a history of SCC of the left posterior maxillary alveolar ridge that had been successfully excised with clear margins was referred to the Oral Dysplasia Clinic for periodic evaluation. She complained of xerostomia and mild oral discomfort that was generalized. Her history was negative for tobacco or alcohol use. Clinical assessment identified a faint generalized mucosal erythema in most areas of the mouth but more dominant on the left than the right, without the presence of any specific oral lesion. The erythema was thought to be associated with the xerostomia, but because of her past history of carcinoma, careful visual inspection of the mucosa along with tissue palpation and VELscope examination was completed. The clinical examination failed to identify specific areas of concern, and no discrete oral lesion was identified. VELscope assessment detected the presence of increased light absorption due to the inflammation in the region, but the combination of VELscope illumination and palpation revealed a 4×5-mm region of light absorption (loss of reflectance) that remained after palpation-induced blanching of the surrounding tissue.
The cancer surgeon who had performed her initial surgery was called to observe the VELscope findings, and upon our recommendation the VELscope-positive region was again excised, resulting in a pathologist finding of severe dysplasia and early carcinoma. The presence of generalized erythema likely masked the presence of the lesion, but use of the VELscope allowed identification of premalignant and malignant tissue change from the surrounding erythema associated with the xerostomia. Without the utilization of the scope it is unlikely that the area would have been detected for several months or until it had developed clinical characteristics different enough from the surrounding inflammatory erythema.
Case No. 4
An 86-year-old female of Danish origin presented to the clinic with a complaint of pain and burning of the tissues of the mouth. She had previously been diagnosed, using biopsies, as having erosive oral lichen planus that involved most of the mucosa of the mouth including the buccal mucosa bilaterally, the attached gingiva, the inner surfaces of the lips, all regions of the tongue, the floor of the mouth, and hard palate. The lesions were a mixture of leukoplakia, erythema, ulceration, and de-squamation. Palpation revealed rough surfaces, tissue friability, and hemorrhage. Her past history was positive for regular alcohol consumption for 40 years, tobacco use for 30 years, but none for the past 30 years. Her dental status was excellent with 28 intact teeth, but with advancing periodontal disease in the presence of the severe erosive lichen planus of the gingiva. Because of her history she was periodically biopsied, and at one recall visit visual changes on the inner aspect of the lower lip generated a decision to biopsy that area. A wide region of severe dysplasia was detected, and the area underwent laser ablation. She continued to be followed, and with the acquisition of the VELscope it was also employed in her periodic assessments. The areas being watched with particular care were the region of the prior laser ablation margins and the tongue, but at recall it was noted that the erosive lichen planus of the right buccal mucosa had become more severe, so that area was also more intensively evaluated clinically and with use of the VELsope.
The region demonstrated intense VELscope light up-take and was biopsied along with several other areas of the mouth that showed increased erosive activity but not VELscope light uptake. The biopsy of the buccal mucosa revealed moderately well-differentiated carcinoma, even though it did not clinically look different than other regions of erosion from lichen planus. Use of the scope allowed us to detect malignant change in the field of tissue changes that were not malignant at the time and to target our observations more carefully. Since the original VELscope-positive finding, we have observed another region positive for VELscope light absorption that also demonstrated severe dysplasia and early carcinoma. The patient continues to be followed at 2-month intervals.
Summary
The VELscope is an important aid in patient assessment, and when added to a well-thought out clinical assessment process that takes into consideration the age of the patient and risk factors that include tobacco, alcohol, and immunologic status, it increases the clinician’s ability to detect oral changes that may represent premalignant or malignant cellular transformation. False positive findings are possible in the presence of highly inflamed lesions, and it is possible that use of the scope alone may result in failure to detect regions of dysplasia, but it has been our experience that use of the VELscope improves clinical decision making about the nature of oral lesions and aids in decisions to biopsy regions of concern.Where tissue changes are generalized or cover significant areas of the mouth, use of the scope has allowed us to identify the best region for biopsy. As with all clinical diagnostic activities, no single system or process is enough, and all clinicians are advised to use good clinical practice to assess patients and to recall and biopsy lesions that do not resolve within a predetermined time frame. Lesions that are VELscope-positive and absorb light need to be followed with particular caution, and if they do not resolve within a 2-week period, then further assessment and biopsy are generally advised. It is much better to occasionally sample tissue that turns out to be benign than to fail to diagnose dysplastic or malignant lesions.
In our fight to protect patients from cancer, the VELscope improves our odds for early detection, hopefully resulting in fewer deaths from oral cancer.
References
1. American Cancer Society. Cancer Facts and Figures 2005. Atlanta, Ga: American Cancer Society; 2005. Available at: www.cancer.org/downloads/STT/CAFF2005f4PWSecured.pdf.
2. Carvalho AL, Nishimoto IN, Califano JA, et al. Trends in incidence and prognosis for head and neck cancer in the United States: a site-specific analysis of the SEER database. Int J Cancer. 2005;114:806-816.
Dr. Kois maintains a private practice limited to prosthodontics in Tacoma and Seattle, Wash, and is an affiliate professor in the Graduate Restorative Program at the University of Washington. He received his DMD degree from the University of Pennsylvania School of Dental Medicine and certificate in periodontal prosthodontics with a MSD degree from the University of Washington School of Dentistry. He continues to lecture nationally and internationally, is reviewer for the International Journal of Prosthodontics, and is a member of the editorial board for The Compendium of Continuing Education in Dentistry. Dr. Kois is the recipient of the 2002 Saul Schluger Memorial Award for Clinical Excellence in Diagnosis and Treatment Planning. His memberships to professional organizations include the American Academy of Restorative Dentistry and American Academy of Esthetic Dentistry. In addition, he continues to work with restorative dentists at the Kois Center, a didactic and clinical teaching program. He can be reached at (800) 457-9165 or drkois@drkois.com or by visiting koiscenter.com.
Dr. Truelove is a member of the American Dental Association and a Fellow in the American College of Dentists, the International College of Dentists, the American Academy of Oral Medicine, the American Academy of Orofacial Pain, and the International Association for Dental Research. He is board certified in oral medicine and is a past president of that board. He has been actively engaged in clinical practice devoted exclusively to oral mucosal disease and facial pain for the past 36 years. He has participated in a number of NIH-funded grants and served on NIH study panels, and has also been active in cancer-related programs sponsored by the American Dental Association and the American Cancer Society. He can be reached at edmondt@u.washington.edu.