This article is not intended to intimidate or scare any of my fellow dental professionals. The purpose of this article is to fulfill a commitment I made to myself. As most of you know, I lecture more than 50 times per year to thousands of dental professionals across the United States. I promised that this would be the year that we need to take oral cancer detection seriously. Some of the hot topics I normally lecture about are in the fields of aesthetic dentistry, practice management, laser dentistry, and the like. Those are the areas that many dentists want to hear about and where many want to find success. The area of oral cancer needs our attention…and it needs it now.
Nearly 8,000 people die each year from oral cancer, about one every hour of every day. This year more than 30,000 new cases of oral cancer will be diagnosed in the United States. Nearly two thirds of all oral cancers are detected in advanced stages when the cancer has already metastasized from its original site to regional lymph nodes and other organ systems. Sixty percent of people diagnosed with oral cancer will survive 5 years or more. Oral cancer is scary because it is so disabling and so disfiguring once it reaches the advanced stage. Typical treatment for moderate to advanced cases can run anywhere from $100,000 to $200,000 and can involve an oral surgeon removing a huge part of the patient’s tongue and jaw. Reconstruction and rehabilitation are difficult, and, costs aside, people are never the same after this kind of treatment, no matter how successful it may be. Oral cancer is responsible for more deaths than cervical cancer, Hodgkin’s disease, and melanoma. It affects more men than women and is the 11th most common cancer worldwide. You can now see that our role as dental professionals in oral cancer detection is extremely important.
Have we been doing the job that we should be doing? The American Cancer Society just came out with a study showing that only 15% of patients who usually go to the dentist have ever reported having an oral cancer examination. Now, I would have to believe that most dentists and hygienists are doing an oral cancer examination. The question is, have we been telling the patient that we have been doing this procedure on them? Obviously, we have not gotten the word out that we are doing this examination. For this reason and many others, consumers just are not taking oral cancer very seriously.
One of the areas that we, as a profession, also have to wake up to is that lifestyle risk factors have dramatically changed the patient’s risk profile. You and I typically think that people at risk for oral cancer are patients around age 40 and older who have lifestyle risk factors of tobacco and alcohol use or have a history of oral cancer. Those indeed are the highest-risk population for oral cancer. A definite increased risk is present, however, in any patient over the age of 18 because of human papilloma virus types 16/18 (HPV), especially among those who are sexually active. According to the American Cancer Society, HPV may contribute to the development of approximately 20% to 30% of oral cancer cases, which completely blows away any of our old concepts of who is at risk for oral cancer.
Now, let’s get to the crux of it. Most of us do an oral cancer examination on a regular basis. Please read carefully what I am going to say at this point: this article was not written to describe how to do an oral cancer examination, which generally is a physical examination where we use our eyes to look for any strange lumps or bumps on the hard and soft tissues that may be abnormal. The exam also includes a physical palpation of lymph nodes and other areas of the head and neck to see if there is anything developing. We are looking for those leukoplakia or erythroplakia areas, which may be any size, and at that point, we would then send the patient for further evaluation. That is the typical oral cancer examination that we perform on most patients.
I want to introduce you to an oral cancer screening. Let me make this point very clear. What you do is an examination, not a screening. An oral cancer screening would be an adjunctive test, much like mammography is to breast cancer detection and a Pap smear is to cervical cancer detection.
Let’s look at this a little more closely. The incidence of oral cancer has stayed the same for approximately 30 years with no decrease in its mortality rates. This is because we have not used any additional screening technologies that can help effect a decrease in death rates. In 1972, mammography was introduced as a regular adjunctive screening test to detect breast cancer. In the more than 30 years since then, there has been a 45% decrease in death rates due to breast cancer. The Pap smear was introduced in 1952, and in the more than 50 years that it has been studied, there has been close to an 80% decrease in death rates. That should pretty much tell you that physical examination alone is not nearly as successful as some kind of adjunctive advanced screening test. If we had and if we used an adjunctive screening test, there is no doubt based on these examples that we can effectuate a decrease in death rates related to oral cancer.
Thankfully, we do have adjunctive screening tests in dentistry for oral cancer that we need to institute in our practices immediately.
VELSCOPE
 |
 |
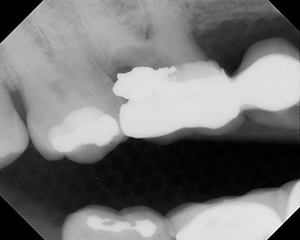
| Figure 1. A suspicious area is found during a typical oral cancer examination using a regular operatory light. (Figures 1 and 2 courtesy of the British Columbia Oral Cancer Prevention Program.) |
Figure 2. The lesion as viewed through a VELscope. |
 |
 |
|
Figure 3. A lesion that was found using the ViziLite system. Notice how the lesion “lights up” using the ViziLite wand. |
Figure 4. The lesion stained with TBlue630—the darkest area is squamous cell carcinoma and is easily identified. |
VELscope (LED Dental) is a device that you insert into the patient’s mouth while you do the oral examination, and, through the process of autofluorescence, it enables you to identify unhealthy soft tissue in the mouth. Healthy tissue has natural fluorescence, and through a VELscope healthy tissue will take on an apple-green tint; abnormal tissue stands out as irregular, dark areas. Suspicious tissue that may be premalignant or malignant has no fluorescence and will look dark through a VELscope (Figures 1 and 2). This is a fairly new device that will require a significant capital investment, and therefore long-term studies are still needed, even though it is based on other established technologies that have not yet been used in the oral cavity.
Recently, based on the peer-reviewed studies done so far, the FDA has given the VELscope expanded indications involving the ability to help detect lesions that may not be visible under white-light examinations, including precancerous and cancerous growths, and the ability to help surgeons ensure that all diseased tissue is successfully removed when excising cancerous lesions.
VIZILITE PLUS WITH TBLUE630
ViziLite Plus with TBlue630 (Zila Pharmaceuticals) is the industry leader in oral cancer screening. ViziLite studies are extensive, and the FDA has long accepted its indication for oral cancer screening. The ViziLite Plus with TBlue630 Oral Lesion Identification and Marking System comprises 2 components: ViziLite, to aid in the early detection of premalignant lesions and oral cancer, and TBlue630 (Zila Tolonium Chloride), a patented, pharmaceutical-grade dye similar to the generic dye known as toluidine blue. The efficacy of chemiluminescence, the technology behind ViziLite, has been evaluated in more than 13,000 patients, including 4 FDA trials, and in multiple published studies in peer-reviewed journals. Chemilumi-nescence has been widely used for more than a decade as an adjunct to the Pap smear, and has been demonstrated to significantly enhance the sensitivity of the Pap smear. There is abundant evidencebased medicine related to the efficacy of generic toluidine blue and its demonstrated use as a preferential stain of premalignant lesions and oral cancer.
The procedure is fairly simple: the patient rinses with a raspberry vinaigrette-tasting solution, a special glow light stick is activated, and this light is then placed in the patient’s mouth. Through the technology of chemiluminescence, healthy tissue will look normal, and unhealthy tissue, which may be premalignant or malignant, will light up and appear whitish in the mouth. These lesions are now very easy to distinguish. If a lesion is found, the toluidine blue in TBlue630 is then used to stain the tissue, and a digital intraoral photograph is taken and sent with the patient to the oral surgeon for further evaluation. TBlue630 is retained in premalignant lesions with a high probability of malignant transformation and oral cancer, and never misses oral cancer (Figures 3 and 4). This is unique to the ViziLite Plus system and is a major leap in oral cancer screening and detection.
ViziLite was FDA-cleared in November 2001; the ViziLite Plus with TBlue630 Oral Lesion Identification and Marking System was FDA-cleared in January 2005. The marking system is FDA-cleared to mark suspicious lesions identified during the ViziLite exam. The ViziLite Plus system is the only FDA-cleared adjunctive screening technology for the identification, evaluation, and monitoring of oral mucosal abnormalities, including premalignant lesions and oral cancer, in a patient population at increased risk for oral cancer (healthy patients age 18 and older).
Much of the ViziLite Plus screening process can be delegated to assistants and hygienists. In our office, the team members will prep the patient, and I will come in and do the screening, even though my dental team will also look into the patient’s mouth and do a screening as well. It never hurts to have an extra set of eyes. This takes approximately 30 seconds of my time for each patient who goes through a ViziLite Plus screening.
This is a very simple system to use, and there is no large initial capital investment to get into this technology. The cost per patient is approximately $19 per use, of which the patient charge for this adjunctive oral cancer screening is a very reasonable $65. Many dental and medical insurances reimburse for this procedure as well. ViziLite Plus is a well-studied system and has proven efficacy in multiple general screening trials.
Even with the best eyes you could possibly have, doing an oral cancer examination is challenging because the mouth has so many different colors and much of the tissue looks the same. In addition, some of these lesions may be a millimeter or less in diameter, and they are easily missed during an examination. ViziLite Plus can help distinguish these lesions so that we can find premalignant and malignant lesions much earlier in the process, thereby giving patients a much better chance at long-term survival.
I could go on and on in this article and try to scare you into doing an oral cancer screening because of the risk management aspects involved. The liability and malpractice issues are huge for cases of oral cancer that have been missed and subsequently not treated. That is not the point of this article. I could even make the case from the revenue perspective about how oral cancer screening can in-crease your production and cash flow. The practice management benefits have been incredible—in addition to lighting up our patients’ mouths with ViziLite Plus, our patients now see us in a different light, as more than dentists but as real physicians of the mouth who are interested in their overall health.
However, the real reason I want you to go ahead and institute oral cancer screening into your office immediately is because it is simply the right thing to do. It is, at this point, an enhanced standard of care. You are doing what is best for your patients who you care so much about, and we as dentists can also be the heroes to our patients. That is what your dental practice is all about.
Dr. Malcmacher is a practicing general dentist in Bay Village, Ohio, and an internationally known lecturer, author, and dental consultant known for his comprehensive and entertaining style. An evaluator for Clinical Research Associates, Dr. Malcmacher has served as a spokesman for the AGD and is a consultant to the Council on Dental Practice of the ADA. He works closely with dental manufacturers as a clinical researcher in developing new products and techniques. For close to 3 decades, Dr. Malcmacher has inspired his audiences and consulting clients to enjoy doing dentistry by providing the knowledge necessary for excellent clinical and practice management. His group dental practice has maintained a 45% overhead since 1988. He can be reached at (440) 892-1810 or dryowza@mail.com. His lecture schedule is available at dentistrytoday.com or commonsense-dentistry.com, where you can also sign up for his monthly practice management teleconferences and free monthly e-newsletter.
Disclosure: Dr. Malcmacher has received educational grant support from Zila for some of his lecture schedule.