The clinical success of an indirect composite resin restoration is measured by function, aesthetics, biocompatibility, and longevity.1 Achieving an ideal restoration begins at the adhesive interface and ends with a proper finishing protocol. Since the principal determinant of the long-term success of these restorations is the strength and durability of the interface,2 this article will describe the fundamental principles for achieving long-term success of these restorations by demonstrating ideal adhesive concepts and proper finishing protocol.
ADHESION AT THE RESTORATIVE INTERFACE
 |
| Figure 1. Scanning electron micrograph of a properly bonded restorative complex. (Courtesy of Dr. Jorge Perdigao.) |
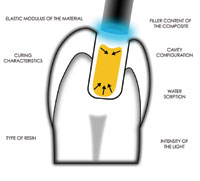
The bonded restorative complex includes the outer layers of the tooth (substrate), the adhesive layer, and the restorative material. The restoration is subject to failure arising from debonding. Defects at the restoration interface result from trapped air voids, voids formed from solvent evaporation, areas of poor wetting, curing shrinkage pores, areas of interfacial contamination, and excess moisture contamination.3 A restorative material properly joined to the tooth substrate will demonstrate (1) a good marginal seal4 with minimal marginal contraction gaps, microleakage, marginal staining, and caries; (2) a durable adhesion between tooth and biomaterial4; (3) reduced stress at the tooth/restorative interface5; (4) biomechanical reinforcement of tooth structure; (5) tissue integrity—specifically, sealing of dentin tubules; (6) long-term functional success5-10; and (7) natural aesthetics and wear resistance5,7-10 (Figure 1).
Achieving a durable adhesion between the tooth and biomaterial depends on the following:
(1) A clean tooth surface.
(2) A low contact angle. Contact angle is the measure of how a fluid wets a solid. A smaller contact angle indicates that a liquid has a good ability to penetrate the micromechanical porosities of a surface. Inherent in the formation of an optimal adhesive bond is the ability of the adhesive to wet and spread on the adherends being joined. Good wetting usually occurs with solids that demonstrate high surface energy. Adhesives should exhibit low viscosities or low surface tension to increase their wetting capabilities. A low contact angle allows the adhesive to spread over the entire surface of the substrate, allowing optimal internal adaptation of the biomaterial to the substrate. This allows an intimate approximation of the material with the substrate without the entrapment of air pockets, which can result in adhesive failure.
(3) Optimal internal adaptation of the biomaterial to the tooth, which promotes an intimate approximation of the material with the tooth.
(4) No entrapment of air pockets.
(5) Sufficient strength to resist stress from polymerization or occlusal forces.
(6) Complete cure of the adhesive.3,11
(7) An understanding of the morphologic, histologic, and physiologic characteristics of the substrate (enamel and dentin).
A fundamental requirement for achieving a successful bonded restoration is isolation of the tooth, which requires use of the rubber dam. Contamination of the enamel and dentin with saliva, blood, and crevicular fluid can compromise the longevity of the adhesive restorations by affecting adhesion at the interface and reducing bond strength.12,13 Numerous studies report microleakage and reduced adhesion and bond strength as a result of contamination of enamel with saliva,14-17 moisture,18-22 and crevicular fluid.23 As for saliva contamination, this fluid acts a film barrier at the contact surface between the resin and the enamel, lowering the surface energy of the enamel and preventing optimal adhesion.17 In addition, saliva contamination of the etched enamel surface affects the morphological characteristics of the surface, and the glycoproteins in the saliva block the micro-pores that were formed during the etching procedure.16,17 If contamination from intraoral humidity results in a thin layer of moisture on the etched enamel, this could prevent maximum adaptation of resin composite to the enamel surface.18,19 Contamination from crevicular fluid has been reported to reduce bond strengths of composite to etched enamel by 70%.22,23 An in vivo study showed that composite resin bonded to etched enamel with rubber dam isolation demonstrated significantly less microleakage compared to isolation with cotton rolls.17,19 Therefore, for optimal bonding, moisture control should be performed throughout the adhesive procedure, and a rubber dam should be used.24
In addition, subgingival preparations must be isolated using proper gingival retraction to control saliva, crevicular fluid, and blood contamination. If this isolation cannot be achieved, then an adhesive restoration is contraindicated and an alternative should be considered.25
Several other clinical factors can influence adhesion, including the thickness of the resin cement, marginal fit of the restoration, stabilization of the hybrid layer, strength and durability of the interface between the resin cement and the processed resin, and the wear of the luting cement.
A well-adapted restoration should have a marginal fit (internal gap) of 100 µm, however, the use of die spaces may increase that distance to 300 µm.26,27 With thin layers of resin cement, the polymerization shrinkage is primarily directed uniaxially.26,28 Under normal clinical conditions, the resulting wall-to-wall contraction of the composite is proportional to the thickness of the cement. Consequently, well-adapted restorations will have less polymerization strain at the adhesive interface and will demonstrate better internal adaptation and seal.26 Although tight-fitting restorations can lessen micromovement of the restoration, larger cementing spaces can partially compensate for the polymerization forces by allowing the restoration and tooth to slightly move during the luting procedure. Marginal integrity with passive insertion is ideal.
During the cementation appointment, precuring the bonding resin after acid etching the tooth can have an adverse effect by preventing correct positioning of the restoration. At the first appointment, prehybridization, dual bonding, or resin bonding prior to impressioning will stabilize the hybrid layer while preventing the ingress of microorganisms through the dentinal tubules.29 It has been suggested that unpolymerized adhesive may be forced into the open dentin tubules from the pressure of seating an indirect restoration. This could disrupt the pressure gradient within the tubules, and after polymerization result in pres-sure on the odontoblastic proces-ses. The result may be postoperative thermal sensitivity, pain on mastication, and possible subsequent irritation of the pulp—all of which could lead to clinical failure.29,30
Adhesive bonding of laboratory-processed composite resins increases their resis-tance to fracture.31 A principal determinant of the long-term success of these restorations is the strength and durability of the interface between the resin cement and the bondable surface of the processed resin.32 The surface of these laboratory-processed composite resins is highly polymerized with no unreacted free-end radicals for bonding to the resin cement.
 |
 |
| Figure 2. The internal surface of the inlay was microetched with aluminum oxide, and the remaining particles were removed with an air syringe. | Figure 3. A thin layer of composite primer was applied to the internal surface of the restoration, lightly air dried, and light-cured for 20 seconds. |
While microleakage has been reported to occur at the interface between the internal surface of the inlay and the resin cement when composite softening agents are not used,33 several surface treatments have been advocated to promote adhesion between the resin cement and the indirect composite restoration. Mechanical roughening of the internal surface of the inlay can be accomplished with diamond burs, or micro-etching can be performed with 50-µm aluminum oxide (AO) particles or 30-µm silan-ized, silica-coated AO particles (CoJet-Sand, 3M ESPE). These procedures create a mechanical retention bond at the microscopic level between the restorative material and the resin cement. In addition to mechanical roughening, an application of proprietary softening agents, wetting agents, or silane has been reported to enhance the bond strength between the restoration and the resin cement34 (Figures 2 and 3).
 |
| Figure 4. The wear pattern of composite luting cements with occlusal surfaces. The cement rapidly undergoes vertical wear until approximately half of the cementing space width is attained. From this point, material loss should be reduced to a minimum. |
At functional tooth surfaces, the wear of resin luting cements is greater than that of the restorative composites.35 Since occlusal wear is directly proportional to the interfacial gap,35 the cementing gap should be reduced in the occlusal aspect (Figure 4). The proper sequence in the luting procedure may balance this interplay between polymerization shrinkage and adhesion. This will also improve marginal adaptation and seal and bond strengths while further reducing polymerization stress at the interface.
REFINING THE RESTORATIVE INTERFACE
In the laboratory phase, careful development and shaping of the composite resin should occur in consideration of the preoperative occlusal registration. This is accomplished prior to curing of the material, thereby allowing the establishment of correct anatomic morphology and occlusal harmony and minimizing the finishing protocol at the time of cementation.36 In addition, anticipating the final result before laboratory and clinical completion will mean that excessive modification of the restoration will not be needed. As a result, the color effects within the restoration as well as the primary and secondary anatomical morphology will not be lost.
A proper intraoral finishing and polishing protocol can influence the longevity of indirect restorations by affecting wear resistance37,38 and marginal integrity. A brief delay before initiating finishing and polishing with various techniques results in a surface of similar hardness to, or harder than, that which is obtained with immediate finishing. The effects of delayed finishing appear to be specific to the bonding system and tissue.39 Specifically, the bond strength of resin to enamel and dentin is higher at 24 hours than immediately after placement.40 Since some of this improvement oc-curs within several minutes after placement of the restoration, it is suggested that a brief delay in the finishing procedure may help to preserve marginal integrity. The margins of indirect composite restorations should then be re-etched and sealed with low-viscosity resins (eg, Optiguard, Sybron/Kerr; Fortify, BISCO; UltraSeal XT plus, Ultradent Products). Application of a composite surface sealant after the initial finishing procedure may help to seal microcracks or microscopic porosities that may have been formed during finishing. In addition, this application has been shown to reduce the wear rate of posterior composite restorations.41
The finishing and polishing procedure depends on the clinician, the composite restorative material used, and the instruments employed. However, a proper finishing and polishing process will not improve the clinical result when there is inadequacy in preparation design, improper restorative material selected, and a deficient or inconsistent adhesive protocol.
CLINICAL RECONSTRUCTIVE PHASE
Adhesive Protocol
 |
| Figure 5. Preoperative occlusal view of a defective composite restoration with recurrent decay on a maxillary left first molar. |
The following clinical protocol is a continuation of the case discussed in Part 1 of this article involving a maxillary left first molar (Figure 5). Once anesthesia had been administered to the patient, the provisional restoration was removed using a spoon excavator to lift it away from the tooth. This is needed since the provisional material flexes. The cavity preparation was cleaned using hand and sonic instruments, and the preparation was rinsed thoroughly to eliminate all residual debris. A throat pack of gauze was placed prior to removal of the provisional restoration and during try-in of the composite inlay to protect the patient from aspirating the restoration.42 The restoration was tried in for the evaluation of color and marginal adaptation. The interproximal contact was inspected, and necessary equilibrations were made.
 |
| Figure 6. The preparation was cleaned with 2% chlorhexidine. |
The tooth was isolated with a rubber dam to protect against contamination and to achieve adequate field control.20,43 The preparation was cleaned with a disinfectant (Consepsis/Consepsis scrub, Ultradent), rinsed, and lightly air dried (Figure 6). The enamel cavosurface was etched with 37.5% acid for 30 seconds, rinsed, and air dried. A self-etching primer (LINKMAX,GC America) was applied with an applicator tip to the entire cavity surface, allowed to remain for 30 seconds, and then lightly air thinned. Any excess material can be removed by blotting with an applicator (Figures 7a and 7b).
 |
 |
| Figures 7a and 7b. A self-etching primer was applied to the entire cavity surface with an applicator tip (a) and allowed to remain for 30 seconds, and then lightly air-thinned (b). |
To improve the adhesion at the interface of the inlay and the luting composite resin cement, the internal surface of the inlay was microetched with aluminum oxide, and any remaining particles were re-moved with an air syringe. A thin layer of composite primer (LINKMAX, GC America) was applied to the internal surface of the inlay, air dried, and light cured for 20 seconds.
 |
 |
| Figure 8. Glycerin was applied to the distal surface of the maxillary left second premolar with unwaxed floss as a separating medium. | Figure 9. The excess resin cement was removed with a No. 00 sable brush using the “wet brush” technique, leaving a residual amount to compensate for polymerization shrinkage. |
After the surface treatment, a small amount of glycerin was applied to the adjacent proximal surface of the second premolar, and the restoration was cemented with a clear, light-cured/dual-cure composite resin cement (LINKMAX, GC America, Figure 8). The cement was mixed and placed onto the internal aspect of the restoration. A blunt tip instrument was used to seat and hold the restoration firmly in place for 1 minute, and the excess cement was removed with a sable brush (Figure 9). It is imperative to leave a residual amount of cement to prevent voids and compensate for the polymerization shrink-age of the cement. Initial polymerization is for 2 seconds while the restoration is held in place with the blunt tip instrument. The residual cement was removed with a scalpel blade (No. 12, Bard Parker), and a thin application of glycerin was applied to all the margins to prevent the formation of an oxygen inhibition layer on the resin cement.44 The restoration was polymerized from all aspects: facial, occlusal, lingual, and proximal surfaces, each for 40 seconds.
Finishing and Polishing
The aesthetic appearance of the surface of a composite resin restoration is a direct reflection of the instrument system and protocol utilized.45 The surface of the composite can be finished and polished with a variety of techniques. Diamonds, multifluted burs, discs, polishing points, and cups have all been used to produce the desired shape, color,46 and luster. Preoperative planning and laboratory procedures employed during the development of the laboratory-processed composite resin restorations can minimize the finishing and polishing procedure.47
 |
| Figure 10. The restorative interface was refined with a 30-fluted, egg-shaped finishing bur. |
The final restorative phase of finishing and polishing was achieved with minimal effort. Occlusal refinement can be achieved with 30-fluted, egg-shaped finishing burs (OS1, Brasseler USA, Figure 10), while the lingual surface can be finished using needle-shaped burs. The cavosurface margins were finished using a dry protocol with light pressure at conventional speed to prevent heat buildup. This dry finishing allows the clinician to observe the tooth/resin interface closely while comparing anatomical contours with the surrounding dentition. The interproximal region was refined with composite polishing paste and aluminum oxide finishing strips. These were used sequentially according to grit and ranged from fine to extra fine.
 |
 |
| Figure 11. The cavosurface margin was re-etched with 37.5% phosphoric acid, rinsed for 5 seconds, and air dried. | Figure 12. A composite surface sealant was applied and light-cured to seal any cracks or microscopic porosities that may have formed during the finishing procedures. |
 |
| Figure 13. Final polishing was accomplished with silicone rubber points and a foam cup with diamond polishing paste. |
After the initial finishing procedure, the margins and surface defects were sealed. All accessible margins were etched with a 37.5% phosphoric acid semigel, rinsed, and air dried (Figure 11). A composite surface sealant was applied and cured to seal any cracks or microscopic porosities that may have formed during finishing procedures (Figure 12). The final polish was initiated with prepolish and high-shine silicone rubber points (Diacomp, Brasseler USA, Figure 13) composed of aluminum oxide particles and silicone that eliminate surface defects. The definitive polish and high luster was accomplished with a foam cup (Enhance, DENTSPLY/Caulk) and a diamond polishing paste (Dia-Polisher, GC America).
 |
 |
| Figures 14a and 14b. Occlusal view of the completed, laboratory-processed composite resin restoration. Note the optical integration of composite resin with the existing tooth structure. |
The rubber dam was removed, and the patient was asked to close with only light contact, followed by closure in centric, protrusive, and lateral excursions. Any necessary equilibration was accomplished with 12 and 30 egg-shaped finishing burs (OS1, Brasseler USA), and the final polishing procedure was repeated. The contact was tested with unwaxed floss to ensure the absence of sealant in the interproximal contact region. The integrity of the margins was then visually inspected with surgical telescopes, and a postoperative radiograph was reviewed. The result is an optimal integration of composite resin with natural tooth structure (Figures 14a and 14b).
Aside from the actual finishing and polishing, the final challenge for the clinician is long-term restorative maintenance of the surface polish. An understanding of the importance of utilizing proper finishing instruments, polishing techniques, and protective surface glazes at maintenance visits will provide a long-lasting, aesthetic restoration.48-50
The surface quality of the restoration is influenced not only by the polishing instruments and polishing pastes used, but also by the composition and the filler characteristics of the composite.51 The newer formulations of indirect resin systems with smaller particle size and increased filler loading allow for improved polishability. Nevertheless, although clinical evidence of polishability of these next generation “ceromers” is promising, the long-term durability of the polish will need to be evaluated in clinical trials.
CONCLUSION
A successful restorative procedure for indirect posterior intracoronal composite resin restorations relies upon good communication between the clinician and laboratory technician, as well as proper cavity design, isolation, occlusion, material selection, and patient compliance.52,53 Fundamental restorative principles include maintenance of sound tooth structure, achieving a sterile, gap-free hybrid layer, and eliminating microleakage by securing a stress-free tooth/restoration interface.
With the emergence of improved restorative materials that have physical properties and characteristics of natural teeth, and the use of restorative techniques that incorporate proper adhesive and finishing protocols, the restorative team (clinician and laboratory technician) can fabricate indirect composite resin restorations that display optimal function, aesthetics, biocompatibility, and longevity.
References
1. Pameijer CH, Grossman O, Adair PJ. Physical properties of a castable ceramic dental restorative material. J Dent Res. 1980;59:474. Abstract 827.
2. Dietschi D, Magne P, Holz J. Recent trends in esthetic restorations for posterior teeth. Quintessence Int. 1994;25:659-677.
3. Craig RG, Powers JM, eds. Restorative Dental Materials. 11th ed. St Louis, Mo: Mosby; 2002.
4. Armstrong SR, Boyer DB, Keller JC. Microtensile bond strength testing and failure analysis of two dentin adhesives. Dent Mater. 1998;14:44-50.
5. Goracci G, Mori G. Esthetic and functional reproduction of occlusal morphology with composite resins. Compend Contin Educ Dent. 1999;20:643-648.
6. Barkmeier WW, Cooley RL. Laboratory evaluation of adhesive systems. Oper Dent. 1992;suppl 5:50-61.
7. Touati B. Bonded ceramic restorations: achieving predictability. Pract Periodontics Aesthet Dent. 1995;7:33-37.
8. Santos J, Bianchi J. Restoration of severely damaged teeth with resin bonding systems: case reports. Quintessence Int. 1991;22:611-615.
9. Van Meerbeek B, Vanherle G, Lambrechts P, et al. Dentin- and enamel-bonding agents. Curr Opin Dent. 1992;2:117-127.
10. Eakle WS. Fracture resistance of teeth restored with class II bonded composite resin. J Dent Res. 1986;65:149-153.
11. Anusavice KJ. Structure of matter and principles of adhesion. In: Anusavice KJ, Phillips RW, eds. Phillips’ Science of Dental Materials. 10th ed. Philadelphia, Pa: WB Saunders Co; 1996.
12. Powers JM, Finger WJ, Xie J. Bonding of composite resin to contaminated human enamel and dentin. J Prosthodont. 1995;4:28-32.
13. Xie J, Powers JM, McGuckin RS. In vitro bond strength of two adhesives to enamel and dentin under normal and contaminated conditions. Dent Mater. 1993;9:295-299.
14. Evans T, Silverstone LM. The effect of salivary contamination in vitro on etched human enamel. J Dent Res. 1981;60:621. Abstract 1247.
15. Silverstone LM. State of the art on sealant research and priorities for further research. J Dent Educ. 1984;48(2 suppl):107-118.
16. Hormati AA, Fuller JL, Denehy GE. Effects of contamination and mechanical disturbance on the quality of acid-etched enamel. J Am Dent Assoc. 1980;100:34-38.
17. Barghi N, Knight GT, Berry TG. Comparing two methods of moisture control in bonding to enamel: a clinical study. Oper Dent. 1991;16:130-135.
18. Knight GT, Berry TG, Barghi N, et al. Effects of two methods of moisture control on marginal microleakage between resin composite and etched enamel: a clinical study. Int J Prosthodont. 1993;6:475-479.
19. Fujii B, Yoshida T, Shimizu T. Effects of humidity on bond strength of composite resins. J Dent Res. 1983;63:664. Abstract 136.
20. Liebenberg WH. General field isolation and the cementation of indirect restorations: Part I. J Dent Assoc S Afr. 1994;49:349-353.
21. Curzon ME, Barenie JT. A simplified rubber dam technique for children’s dentistry. Br Dent J. 1973;135:532-536.
22. Young K, Hussey M, Gillespie F, et al. In vitro studies of physical factors affecting adhesion of fissure sealant to enamel. In: Silverstone LM, Dogon IL, eds. Proceeding of the International Symposium on Acid Etch Technique. St Paul, Minn: North Central Publishing Co; 1975.
23. Stangel I, Nathanson D. An overview of the use of posterior composites in clinical practice. Compendium. 1987;8:800-806.
24. Magne P, Dietschi D, Holz J. Esthetic restorations for posterior teeth: practical and clinical considerations. Int J Periodontics Restorative Dent. 1996;16:104-119.
25. Jackson RD. Indirect resin inlay and onlay restorations: a comprehensive clinical overview. Pract Periodontics Aesthet Dent. 1999;11:891-900.
26. Dietschi D, Spreafico R. Adhesive Metal-Free Restorations: Current Concepts for the Esthetic Treatment of Posterior Teeth. Chicago, Ill: Quintessence Publishing; 1999.
27. Ariyaratnam M, Wilson MA, Wilson NH, et al. Variation in the thickness of the composite lute with an indirect composite inlay system. Restorative Dent. 1990;6:16-18.
28. Feilzer AJ, De Gee AJ, Davidson CL. Increased wall-to-wall curing contraction in thin bonded resin layers. J Dent Res. 1989;68:48-50.
29. Jayasooriya PR, Pereira PN, Nikaido T, et al. The effect of a “resin coating” on the interfacial adaptation of composite inlays. Oper Dent. 2003;28:28-35.
30. Blank JT. Scientifically based rationale and protocol for use of modern indirect resin inlays and onlays. J Esthet Dent. 2000;12:195-208.
31. Jordan RE. Esthetic Composite Bonding: Techniques and Materials. 2nd ed. St Louis, Mo: Mosby-Year Book; 1992.
32. Sun R, Suansuwan N, Kilpatrick N, et al. Characterisation of tribochemically assisted bonding of composite resin to porcelain and metal. J Dent. 2000;28:441-445.
33. Bouschlicher MR, Cobb DS, Vargas MA. Effect of two abrasive systems on resin bonding to laboratory-processed indirect resin composite restorations. J Esthet Dent. 1999;11:185-196.
34. Suzuki S, Leinfelder KF, Shinkai K. Wear resistance of resin cements. Am J Dent. 1995;8:83-87.
35. Noack MJ, De Gee AJ, Roulet JF, et al. Interfacial wear of luting composites ceramic inlays in vitro. J Dent Res. 1992;71:113. Abstr