The development of a treatment plan for the patient with advanced periodontal disease can be imposing, but with proper sequencing, treatment planning need not be a complex process.1,2 In 1977 Saul Schluger,3 a founder of modern periodontology wrote, It is easy and attractive to adopt a single method to apply to all cases of periodontal disease, no matter how complex. To do that, however, means the lowering of objectives and the acceptance of the loss of teeth that might otherwise have been restored to health… “It also means that all methods at our disposal will be brought to bear, when necessary, in the long-range management of the case.” Today, as in the past, there is no substitute for accurate diagnosis and treatment planning. By taking a comprehensive, multidisciplinary approach, our chances of success are improved.
It is important first to make a diagnosis of all the disease entities contributing to the patients overall disease state. By defining the cause of the patients disease, the therapist can determine how to control the factors that caused it. There are 2 aspects of developing a diagnostic plan: functional needs and aesthetic concerns. An accurate and comprehensive diagnosis will dictate the appropriate treatment for functional needs and enable us to re-establish a healthy dentition.
Before proceeding with therapy, it is equally important to assess the patients aesthetic concerns and expectations and incorporate them into the treatment plan. The integration of procedures to meet these desires is essential to achieve an end result that satisfies everyone. This means that both periodontal and restorative goals must be delineated at the onset. The treatment plan can then be communicated to the patient so the full scope of therapy is understood. By knowing the desired end result, the dental team can develop and execute the most effective treatment plan.
DIAGNOSIS
 |
| Chart 1. Treatment Plan Sheet. |
Diagnosis starts with a thorough examination of the patient. First, an intraoral and extraoral evaluation is necessary to rule out pathology (upper left on Chart 1). To avoid errors, evaluation of a full series of radiographs is essential and should be coordinated with the clinical review.
 |
 |
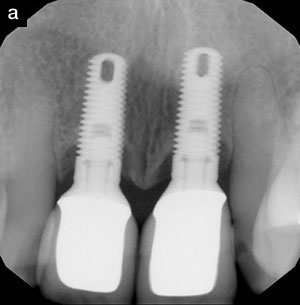
| Figure 1a. Mild horizontal bone loss is present. A periodontal probe is in place directly interproximal. | Figure 1b. Buccal, lingual, and distal walls remain. Without a thorough probing, this lesion would go undetected until either the buccal or lingual bony plates were lost. |
Assessment of periodontal and restorative status is next. Pocket probing, areas of recession, mobility, and mucogingival status should be recorded. Caries and defective restorations are also noted (lower center of Chart 1). Periodontal probing must be accomplished by dragging the probe 360 degrees around the sulcus, including the interproximal areas (not just the line angles), to avoid missing interproximal attachment loss (Figures 1a and 1b). The deepest areas in each of the 6 regions are recorded. The chart is designed so that all aspects of potential dental therapy are reviewed.
| Table 1. Tissue Character and Expected Results From Therapy. | ||||||||||||
|
The status of the deposits present and the status of the tissue should be assessed (bottom center and left sides of Chart 1). This helps the therapist determine what to expect as a result of the first phases of therapy (Table 1). An evaluation of the occlusion is made with respect to bidigital mobility, fremitus, mobility in function, tooth wear, and habits (center portion of Chart 1). Once all of the data is collected, a diagnosis can be made that will define the necessary therapy.
THERAPY: DISEASE CONTROL AND GOALS
It is first necessary to evaluate functional needs, including inflammatory periodontal disease, occlusal factors, and restorative problems due to caries or failing restorations. In addition, teeth with apical infections or hopeless teeth that might be endangering adjacent teeth need to be treated or extracted. This article will focus on inflammatory disease, periodontitis (slight, moderate, and severe), and occlusal trauma (primary and secondary).
 |
 |
| Figure 2a. Preoperative photograph demonstrates extremely swollen gingiva due to heavy calculus. | Figure 2b. Postoperative photograph demonstrates the results of root planing. No surgical therapy was necessary. |
The diagnosis of periodontitis means that there has already been some bone loss, thus the therapist is not treating gingival disease. Plaque control and root planing are the first steps for treating most inflammatory periodontal diseases. Root planing, however, has limitations.4-6 Most authors agree that effective calculus removal cannot surpass 4-mm pocket depth. If pockets are greater than 4 mm and the tissues are edematous, it is possible initially to decrease the pocket depth after the first root-planing visit, thus making more complete calculus removal feasible during subsequent visits. The response to this series of root-planing visits depends on the quality of the tissue (Figures 2a and 2b). Gingiva can be edematous, fibrotic, or fibrous externally with the sulcus being ulcerated (Table 1).
If there is a single site in a quadrant that has pocket depth greater than 5 mm with symptoms of either bleeding or exudates, it may be feasible to utilize site-specific therapy,7 either surgical or chemotherapeutic. If it is feasible to completely remove calculus present on the root and pocket depth and if symptoms remain decreased for a significant amount of time, site-specific therapy would be valuable. However, if uneven patterns of bone loss or calculus cannot be removed, chemotherapeutic therapy would not be indicated.
| Table 2. Types of Occlusal Trauma and Possible Therapy. | |||||||||
|
The effects of occlusal trauma are often overlooked or underestimated. This is unfortunate since trauma from occlusion is one of the most significant contributing factors of periodontal disease and can lead to increased bone loss.8 Occlusal trauma has been shown to cause bone loss without pocket formation.9 In periodontitis, the bone loss initiates from the osseous crest inward. In occlusal disease, the bone loss initiates in the marrow cavities. However, in the presence of inflammatory disease, it often leads to a more rapid progression of bone loss.10,11 This explains why a patient can have a rapid change in alveolar height or a patient with nonprogressive disease suddenly has significant bone loss. Table 2 lists the types of occlusal trauma and possible therapy necessary to control them.
 |
 |
| Figure 3a. A 29-year-old female presented with large diastemas, advanced bone loss, and an unaesthetic appearance. | Figure 3b. After 3 months of tooth movement, the teeth have no diastemas, decreased mobility (they have been bonded for more than 20 years), and a better appearance. |
 |
 |
| Figure 4a. Radiograph demonstrates a mesially tipped molar with an angular defect on the mesial. | Figure 4b. After 4 months of movement, the molars are in improved axial inclinations, the defect on the mesial has leveled, and sulcular depths are minimal. |
 |
 |
| Figure 5a. This radiograph demonstrates advanced bone loss in the mandibular anterior. | Figure 5b. Subsequent to regenerative treatment, there is a marked improvement, improved crown-to-root ratios, and less mobility. This is a 7-year postoperative radiograph. |
Orthodontic movement such as retraction, cross-bite correction, or uprighting of tipped molars can be an aid in the treatment of periodontally diseased teeth (Figures 3a, 3b, 4a, and 4b). Simple orthodontic movement over a limited time (3 to 4 months) can result in improved axial alignment, correction of osseous defects, and improved crown-to-root ratios.12,13 As long as inflammation is controlled and orthodontic forces are not excessive, even teeth with ad-vanced bone loss can be moved.14 Another way to improve the crown-to-root ratio is to use bone regenerative therapy15 (Figures 5a and 5b).
The diagnosis of fremitus in conjunction with mobility warrants interceptive treatment. This indicates trauma from occlusal interferences, and if it is left untreated, the mobility will likely increase. Careful occlusal equilibration will often eliminate the interferences and alleviate this problem. If the problem cannot be relieved by occlusal equilibration, then other therapies such as orthodontics or restorative dentistry should be considered.
There is often controversy regarding the question of when to splint teeth. If there is secondary trauma (inadequate periodontium to support normal forces) and significant mobility present, then splinting can greatly improve the function and comfort of the teeth. If it is determined that splinting is necessary due to mobility and diminished attachment apparatus, then it is important to incorporate this into the first phases of treatment by placing provisional restorations or intracoronal stabilization. This will aid in the stability of the dentition, permit easier access to the teeth during surgery, and commit the patient to the desired endpoint early in treatment. In patients with generalized severe attachment loss and mobility, it may be necessary to extend the posterior splint across the anterior to achieve cross-arch stabilization.9 Control of mobility can be determined by evaluating the provisional restoration.
 |
| Figure 6. Full-arch restoration with implant dentistry was performed 17 years prior. |
If inadequate dentition is left to support function, then prosthetic and implant dentistry should be considered. Implant-supported restorative dentistry will enable the therapist to provide support and function where needed by replacing part of the dentition that was lost. Implant dentistry should also be considered as a technique to break up long-span bridges if the adjacent teeth do not require stabilization. Since the introduction of implant dentistry by Professor P. I. Branmark, dentistry has had a predictable alternative for tooth replacement. The loss of a single tooth no longer dictates full-coverage restorations on the adjacent teeth. In addition, fixed appliances are now possible in situations that once needed removable appliances (Figure 6).
In the first part of therapy, the therapist should accomplish caries control and endodontic treatment on salvageable teeth. Future aesthetic and restorative needs also should be determined during this first phase of treatment. To avoid biologic width problems, the restorative dentist should relate to the periodontist any concerns regarding teeth that have inadequate crown length.16,17 This communication also can include concerns of uneven gingival levels due to recession or altered passive eruption. A diagnostic wax-up often is helpful in communicating the ideal tooth form and soft-tissue concerns (fabricated by the restorative dentist). In this manner, the necessary surgical treatment can be coordinated and planned. The surgical therapy may include both crown lengthening (to expose tooth structure, provide adequate biologic width, and even gingival margins) and gingival grafting (to decrease gingival recession and increase keratinized gingival tissues).
THERAPY: SURGICAL AND RECONSTRUCTIVE
| Table 3. Therapy for Periodontitis of Differing Severities. | ||||||||
|
| Chart 2. Sequence of Therapy |
|
1. Control the cause of the disease process (etiology). 2. Correct the deformities that the disease process has caused. |
Pocket reduction therapy, including apically positioned flaps, osseous corrections, and, if indicated, regenerative therapy, has been shown to be the most effective way to correct periodontal defects, especially in moderate and severe periodontitis.18 If the patient has not responded with significant pocket reduction to scaling and root planing, surgical therapy is the usual treatment choice. The goal of periodontal therapy is to provide an environment that the patient and professionals can maintain over a long-time period. In the 45 to 60 minutes allocated for preventive treatment visits (PTV),* it is much easier to accomplish effective maintenance if there are a minimal number of pockets with depths greater than 5 mm. Once there is sufficient healing time (approximately 8 to 12 weeks), final restorations can be fabricated. Table 3 summarizes the therapy necessary for periodontitis of differing severities.
*PTV is used to replace a recall or maintenance visit. It denotes both prevention (P) and active treatment (T).
SEQUENCE OF THERAPY
Once all diagnostic information is collected and evaluated and the treatment plan developed, the sequence of treatment can be finalized (Chart 2). The first step is bringing the active disease process under control, including both caries and inflammatory periodontal disease. Next, the occlusal disease should be treated and stabilized. The question of when to extract a questionable or hopeless tooth often arises in patients with advanced periodontal disease. It often is advantageous to retain a hopeless tooth through the early phases of treatment unless it is affecting an adjacent tooth. These teeth may help in stabilizing the occlusion on an interim basis. If a tooth needs to be extracted early in treatment, then the extraction should be coordinated between the periodontist and the restorative dentist so any necessary provisional restorations can be constructed and the extraction site augmented at the time of extraction. Often a hopeless or questionable tooth can be retained until periodontal surgery when a final decision can be made, thus avoiding multiple surgeries for the patient. Once the active disease processes are controlled and the patient is stable, the corrective therapy of periodontal surgery and final restorative dentistry can begin. Chart 2 delineates a sequence of treatment, which if followed will provide the therapist with an orderly treatment progression.
CASE REPORT
The following case report demonstrates the integration of several different disciplines (periodontics, orthodontics, and restorative dentistry) to control the factors that cause the disease process and then correct the deformities the disease process caused.
Diagnosis
 |
 |
| Figure 7a. Clinical photograph demonstrates large diastemas in the anterior. | Figure 7b. Radiographs of the maxillary and mandibular anterior teeth demonstrate advanced bone loss. |
 |
 |
| Figures 7c and 7d. Posterior radiographs show many infrabony lesions throughout. |
The patient presented with moderate to advanced periodontal disease with secondary occlusal trauma in the anterior. There was flaring of the maxillary and mandibular anterior teeth (Figure 7a). Radiographic evaluation demonstrated advanced bone loss in the anterior region with vertical bone lesions in the posterior region (Figures 7b, 7c, and 7d).
SEQUENCE OF THERAPY
A consultation with the restorative dentist, orthodontist, and periodontist permitted the team to develop the following treatment plan sequence:
(1) scaling, root planing, and plaque control
(2) occlusal therapy
a. orthodontics (retraction of the maxillary and mandibular anterior teeth)
b. occlusal equilibration
c. stabilization (splint teeth Nos. 4 to 13 and teeth Nos. 22 to 27)
(3) periodontal surgery (regenerative therapy and osseous reshaping)
(4) restorative dentistry
a. fixed bridge for teeth Nos. 4 to 13
b. A-splint teeth Nos. 22 to 27
(5) night guard
(6) preventive treatment visits (every 2 months).
 |
 |
| Figure 7e. Final tooth position was achieved in both maxilla and mandible. The dentition was stabilized. | Figure 7f. This lesion was indicative of others encountered in the posterior region. |
 |
 |
 |
| Figures 7g, 7h, and 7i. Postoperative radiographs show the amount of bone regeneration that has occurred. Note the improved position of the maxillary and mandibular anterior teeth. |
The above treatment plan was followed, first controlling all of the factors that caused the disease and then correcting the deformities it caused. Two visits of root planing were performed in order to control the inflammation. Tooth movement was performed to close the diastema (Figure 7e). Deep infrabony defects were present throughout the dentition (Figure 7f). Significant regeneration of bone is evident in the postoperative radiographs (Figures 7g, 7h, and 7i).
DISCUSSION
| Table 4. Diagnosis and Goals of Treatment. | ||||||||||
|
This patient presented with advanced periodontal disease. A diagnosis of secondary occlusal trauma was made with respect to the anterior segments (inadequate attachment to withstand normal forces). Splinting was required. The maxillary and mandibular anterior teeth exhibited multiple diastemas that prohibited splinting in these areas. In addition, the patient exhibited a strong tongue thrust. Thus, orthodontic therapy was required to close the spaces (Table 4).
A sequence of therapy was followed, which first involved controlling the factors that caused the disease, eg, inflammatory factors (root planing) and occlusal disease (orthodontics, equilibration, splinting). The next phase involved correcting the deformities the disease process caused, eg, periodontal surgery (resective and regenerative) and restorative dentistry (A-splinting and fixed bridgework). Long-term dental health and stability were achieved.
SUMMARY
Through the use of periodontal, orthodontic, and restorative procedures, this patient was restored to function with a stable dentition and minimal pocket depths. The patient was followed for 10 years. All areas exhibited a healthy periodontium with stability of all areas of the dentition.
Acknowledgment
The author wishes to thank Dr. Gordon Douglass for his help in preparation of the manuscript.
References
1. Goldberg PV, Higginbottom FL, Wilson TG. Periodontal considerations in restorative and implant therapy. Periodontol 2000. 2001;25:100-109.
2. Wagenberg BD. Treatment planning the advanced disease case. Periodontal Case Rep. 1986;8:17-26.
3. Schluger S, Yuodelis R, Page RC, et al. Periodontal Disease: Basic Phenomena, Clinical Management, and Occlusal and Restorative Interrelationships. Philadelphia, Pa: Lea & Febiger; 1977:2.
4. Waerhaug J. Healing of the dento-epithelial junction following subgingival plaque control. II: As observed on extracted teeth. J Periodontol. 1978;49:119-134.
5. Stambaugh RV, Dragoo M, Smith DM, et al. The limits of subgingival scaling. Int J Periodontics Restorative Dent. 1981;1:30-41.
6. Cobb CM. Clinical significance of non-surgical periodontal therapy: an evidenced-based perspective of scaling and root planing. J Clin Periodontol. 2002:29(suppl 2):6-16.
7. Williams RC, Paquette DW, Offenbacher S, et al. Treatment of periodontitis by local administration of minocycline microspheres: a controlled trial. J Periodontol. 2001;72:1535-1544.
8. Harrel SK, Nunn ME. The effect of occlusal discrepancies on periodontitis. II. Relationship of occlusal treatment to the progression of periodontal disease. J Periodontol. 2001;72:495-505.
9. Eskow RN, Wagenberg BD. Repair of crestal lesions in primary occlusal trauma: a case report. Int J Periodontics Restorative Dent. 1981;1:70-74.
10. Nyman S, Lindhe J, Ericsson I. The effect of progressive tooth mobility on destructive periodontitis in the dog. J Clin Periodontol. 1978;5:213-225.
11. Polson AM, Zander HA. Effect of periodontal trauma upon intrabony pockets. J Periodontol. 1983;54:586-591.
12. Bednar