The most frequently isolated human oral fungal pathogen is Candida albicans.1 Other opportunistic and emerging fungal organisms of the oral cavity include Candida tropicalis, C. parapsilosis, C. glabrata, C. krusei, C. dubliniensis, C. inconspicua, C. lipolytica, C. lusitaniae, C. rugosa, and C. zelanoides.2,3 Candida exists as an oral commensal in 40% to 60% of humans.4 Candida is an opportunistic organism and becomes an infection when the oral environment is modified due to factors such as xerostomia, removable acrylic prosthetic appliances, contact with active infection from another individual or another anatomic location, antibiotic therapy, poor oral hygiene, loss of vertical dimension, nutritional deficiency, pregnancy, steroid therapy, or immunodeficiency.5,6 Candida infection of the tongue is relatively commonplace; these lesions are found in approximately 2% of the general population.7 Terai and Shimahara8 reported 14 patients with tongue atrophy and burning pain (a lack of filiform papillae of the dorsal tongue) secondary to a Candida infection. After antifungal therapy, the tongue pain improved markedly in 80% of cases, and simultaneously, the filiform papillae regenerated. Furthermore, Gorsky, et al9 demonstrated improvement in many patients with intraoral burning pain without clinical findings after antifungal drug therapy.
The pseudomembranous form (also known as thrush) is perhaps the most readily recognized form of oral candidiasis. Thrush is a superficial infection of the outer layers of the epithelium, resulting in the formation of patchy, white removable plaques. These plaques may be removed with relatively gentle rubbing or scraping, and often reveal an underlying area of erythema. This appearance is characteristic, and usually a clinical diagnosis is relatively obvious. However, a smear, culture, or a clinical trial may be helpful when the diagnosis is less certain. Thrush is seen in both children and adults whenever the number of Candida organisms in the oral cavity increase to a level that produces clinical infection. Candida lesions of thrush respond rapidly to therapy. Sometimes Candida lesions disappear spontaneously or with minimal therapy.1,3,6,10
The clinical presentation of oral candidiasis includes both acute and chronic infections. Acute forms include (1) pseudomembranous or thrush form, which demonstrates white plaques that reveal an erythematous base when removed, and (2) erythematous or atrophic form, in which the oral mucosa appears intensely red. Chronic forms include (1) chronic hyperplastic candidiasis, which demonstrates white, nonremovable plaques, (2) denture-induced stomatitis (denture sore mouth), which presents as erythema underneath the denture base, (3) angular cheilitis or perleche, which presents as crusted areas at the corners of the mouth, (4) median rhomboid glossitis, which presents as the absence of filiform papillae and an irregularly shaped erythematous area on the dorsal tongue, (5) a multifocal form, which demonstrates several of the above categories, and (6) a chronic (or acute) atrophic form, which demonstrates a loss of filiform papillae on the dorsal tongue5,8,10 (Figures 1 to 6).
 |
 |
|
Figure 1. Thrush in an infant. |
Figure 2. Thrush in an adult. |
 |
 |
|
Figure 3. Angular cheilitis. |
Figure 4. Chronic hyperplastic candidiasis of the tongue. |
 |
 |
|
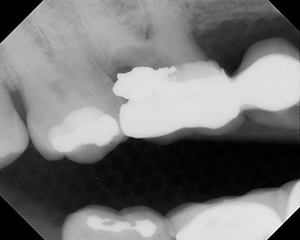
Figure 5. Denture sore mouth. |
Figure 6. Median rhomboid glossitis. |
Case No. 1
 |
 |
|
Figure 7. Diminution of the dorsal filiform papillae of the tongue. |
Figure 8. Minor reduction of the dorsal filiform papillae of the tongue is noted. |
 |
 |
|
Figure 9. Dorsal tongue appears to be normal. |
Figure 10. Normal tongue, but evidence of angular cheilitis. |
A 26-year-old female presented in September of 2005 with a chief complaint of “My mouth hurts and burns.” The pain had persisted for the last 5 years. While she had seen several physicians and dentists, none were able to resolve the problem. The medical history was not contributory, the patient was in excellent health, and she was not currently taking any prescription medications. She had taken over-the-counter (OTC) analgesics such as acetaminophen and ibuprofen, and her physicians had given her antibiotics in the past for medical conditions such as a streptococcal infection. She stated that previous blood studies were negative for anemia.
The oral examination was essentially within normal limits with the exception of a diminution of the dorsal filiform papillae of the tongue (Figure 7). The tentative diagnosis was chronic atrophic oral candidiasis. A prescription was written for a 2-week regimen of clotrimazole 10-mg troches11 with the patient instructed to let 1 troche melt in the mouth 5 times a day. The patient returned for follow-up after 2 weeks, reporting remarkable improvement and the absence of the burning pain. However, the clinical examination revealed that the filiform papillae of the dorsal tongue were still reduced (Figure 8). Further, angular cheilitis was noted (this condition was not noted at the initial visit). The patient was placed on a 2-week regimen of fluconazole 100-mg tablets (15 tablets, 2 tablets immediately and 1 tablet daily).11 The patient returned after 2 weeks, and the dorsal tongue appeared to be normal (Figure 9).
Six weeks later the patient again returned with burning pain associated with the tongue. Her physician had placed her on antibiotics for flu-like symptoms 3 weeks previously. The clinical examination revealed a normal appearance of the tongue but evidence of angular cheilitis (Figure 10). The patient was placed on a 2-week regimen of fluconazole 100-mg tablets (15 tablets, 2 tablets immediately and 1 tablet daily), and subsequently reported by telephone that the burning discomfort was eliminated.
Case No. 2
A 53-year-old male patient presented in December of 2000 with a chief complaint of “My tongue looks strange.” The medical history was significant. The patient reported a heart murmur, a damaged heart valve, and surgery to repair the valve in 1997. He had a previous history of angina and had undergone several angioplasty procedures since 1984, the last of which was only a few weeks prior to his visit. He had a coronary artery bypass in 1986 and a blood transfusion at that time. He also reported a history of arthritis, for which he was taking celecoxib. Other current medications included pravastatin for cholesterol, atenolol and furosemide for hypertension, and daily aspirin for decreased platelet adhesion. He noted neuropathic pain/peripheral neuropathy of the chest and left leg, secondary to previous operations. For this condition he was taking gaba-pentin, clonazepam, dextromethorphan, and oxycodone. He was taking daily folic acid to reduce high serum levels of homocysteine. He was also taking vitamins B12, B6, E, and C. He denied smoking cigarettes and reported moderate alcohol use. He had no known drug allergies. The patient’s general dentist had identified an aberrant appearance of the tongue approximately 2 years prior to his visit to our facility. Within the previous 6 months or so, the patient noticed sensitivity to spicy foods.
No lymphadenopathy was noted. The tongue had an atrophic appearance on the dorsal anterior surface, consistent with the absence of filiform papillae. A visual examination revealed that the major salivary glands did not produce saliva, and the minor salivary glands produced only a limited amount. There were bilateral areas of patchy erythema on the buccal mucosa. The remaining soft and hard oral tissues appeared to be within normal limits. The dentition appeared to be in excellent condition.
The diagnoses were atrophic tongue secondary to candidiasis, and relative xerostomia most probably related to drug therapy. In addition, it was necessary to order a complete blood count to rule out anemia. The patient was placed on a 2-week antifungal regimen of fluconazole 100-mg tablets (15 tablets, 2 tablets immediately and 1 tablet daily) and referred to his physician to evaluate for anemia. Furthermore, he was placed on a dry mouth regimen, which consisted of forcing fluids for hydration, use of a cold-water vaporizer for the bedroom, and OTC products, such as saliva gel, for dry mouth. (Note: Dry mouth products from Laclede include Biotène Oral Balance Mouth Moisturizing Gel, dry mouth toothpaste, saliva spray, nonalcoholic rinse, and dry mouth chewing gum.) The patient reported 2 weeks later that his condition had improved. The blood studies were negative.
 |
 |
|
Figure 11. Reduced filiform papillae on the dorsal tongue, central anterior third. |
Figure 12. Tongue appears normal. |
In August of 2001, the patient returned with a similar presentation. Once again, he was prescribed fluconazole 100-mg tablets (15 tablets, 2 tablets immediately and one tablet daily). The patient reported 2 weeks later that his condition had improved.
In March of 2003, the patient presented once again. A white coating was present on the tongue, and the dorsum demonstrated an erythematous central area consistent with median rhomboid glossitis. Once again, the same fluconazole regimen that had been used previously was prescribed. The patient reported 2 weeks later that his condition had improved.
The patient returned again in June of 2003 with a denuded and sensitive tongue. Once again a prescription was written for a 2-week regimen of fluconazole, with one refill. The patient reported that his symptoms had improved after 1 month.
In November of 2005, the patient presented again with sensitivity of the tongue. A medical update revealed no significant changes, except that the patient was no longer taking celecoxib and was using OTC analgesics. A reduction of the filiform papillae on the dorsal tongue (central anterior third) was noted (Figure 11). A prescription was written for the same 2-week regimen of fluconazole used previously, and at the 2-week follow-up the symptoms were relieved. The clinical appearance of the tongue had returned to normal (Figure 12).
Case No. 3
 |
 |
|
Figure 13. Anterior third of the dorsal tongue is slightly erythematous, with normal distribution of filiform papillae. |
Figure 14. Subtle erythema of the mucosa at the vermilion border of both lips. |
In September of 2005, a 47-year-old female presented with a chief complaint of tongue sensitivity. The medical history did not appear to contribute to the chief complaint. The patient had adult-onset asthma but did not use an inhaler. She had a history of hay fever and sinus complaints, and was receiving treatment (injections) for her allergy every 3 weeks. The patient was taking loratadine as needed for her allergies. There were no known drug allergies, but she reported allergies to pollens, grass, dust, and animals. She did not smoke cigarettes and reported drinking alcohol only on occasion.
The condition began in June or July. The patient had difficulty eating, and perioral lesions appeared. Her physician prescribed tetracycline, and the lesions resolved. She noticed mouth pain, followed by the appearance of lesions on her face. She thought that the problem might have been due to the use of a new toothpaste, because its use caused pain. She also reported similar problems with other toothpastes with spearmint flavoring. She noted problems with spicy foods and acidic beverages, but stated that all foods except yogurt could cause problems. She noticed that the corners of her mouth developed lesions, first on one side and then the other. No treatment seemed to help the condition.
Clinically, no lymphade-nopathy was noted. The anterior third of the dorsal tongue was slightly erythematous but demonstrated a normal distribution of filiform papillae (Figure 13). The tongue also displayed a fissured appearance. Slight erythema was noted at the corners of the mouth. Also, there was a subtle erythema of the mucosa at the vermilion border of both lips (Figure 14). The remaining hard and soft oral tissues appeared within normal limits.
A prescription was written for a 2-week regimen of fluconazole 100-mg tablets (15 tablets, 2 tablets immediately and 1 tablet daily) with 1 refill. It was also suggested that the patient add yogurt containing live cultures to her diet. The plan was that if the prescription was not successful in alleviating her symptoms, referral to her physician would be suggested.
Shortly after the initial evaluation, the patient reported that she used an acrylic guard at night. As the previous history had not noted a removable acrylic appliance, new instructions were provided. The acrylic appliance was to be stored in a solution of water and household bleach (4 or 5 drops of bleach added to a cup of water) to prevent reinfection, and the patient was told to rinse the appliance thoroughly before using it. At the 2-week follow-up, the patient reported that her condition was vastly improved, although only minimal changes were noted in her clinical appearance. One month later she reported that she was still sensitive to certain flavorings (such as mint) and some spicy foods, but these symptoms were minor, and overall her condition was much improved.
DISCUSSION
Atrophic tongue or the absence of filiform papillae on the dorsal surface of the tongue is known to be due to deficiencies in nutrients such as vitamin B12, folic acid, or iron.8,12 Terai and Shimahara8 reported that oral candidiasis was evaluated by both culture and cytologic examination in 40 patients with an atrophic appearance of the dorsal tongue, and positive results for a Candida infection were seen in 72.5% and 82.4% of the patients, respectively. However, in a comparison of 3 identification methods (Micro-stix-Candida strips [Bayer], Oricult-N-plates, and periodic acid-Schiff [PAS] method) used for the diagnosis of candidiasis, Skoglund, et al13 reported differences among the 3 tests. They concluded that the possibility should always be considered that these tests may be inaccurate, particularly if other findings and symptoms disagree with the test results.
Gorsky, et al9 evaluated 130 patients with burning mouth and no clinical evidence of candidiasis or other mucosal conditions. These investigators used exfoliative cytology to evaluate this patient population and demonstrated positive findings for fungal infections in 37 patients. However, only 13 of these 37 patients responded to antifungal therapy with a marked improvement, 1 patient demonstrated slight improvement, 22 patients reported no change, and 1 patient was reported to have worsened. Therefore, it does not appear that positive cytology (for Candida) correlates strongly with successful antifungal therapy. In their 1987 study (without exfoliative cytology), Gorsky, et al14 reported that 13 of the 98 burning mouth syndrome patients without clinical findings improved completely when antifungal therapy was administered. Therefore, it appears that burning symptoms in the oral cavity without clinical findings may be due to a subclinical candidiasis infection. The clinical findings in the first 2 cases presented here were subtle and could have been dismissed as within normal limits.
Live-cultured yogurt containing acidophilus bacteria has demonstrated efficacy in the treatment of mucosal candidiasis.15,16 Therefore, this alternate therapeutic approach can be recommended as adjunctive therapy for oral candidiasis. It is important to note that acrylic removable appliances may harbor Candida organisms. Therefore, it is suggested that appropriate measures be taken to eliminate this source of reinfection.
CONCLUSIONS
This article has reported 3 cases that demonstrated only minimal clinical findings, a complaint of burning mouth, and a presumptive diagnosis of oral candidiasis. One patient demonstrated minor erythema of the tongue, and the other 2 demonstrated only minor depletion of the filiform papillae of the dorsal surface of the tongue. Subsequently, one case later displayed median rhomboid glossitis, and another demonstrated a clinical appearance consistent with angular cheilitis. In one case, the predisposing factor appeared to be the use of systemic antibiotics, in another polypharmacy, and in the last a combination of an acrylic appliance and the use of antihistamine medication. Although there was minimal improvement in the clinical appearances with the use of antifungal medication, all of the patients reported improvement in symptoms.
These cases demonstrate that the oral cavity can be infected with Candida, but may demonstrate a variable yet seemingly innocuous appearance. Burning mouth pain may be reported prior to development of obvious changes in some patients with oral candidiasis.
References
1. Samaranayake LP, Lamey PJ. Oral candidosis: 1. Clinicopathological aspects. Dent Update. 1988;15:227-231.
2. McNeil J, Kan V. Oral yeast colonization of HIV-infected outpatients. AIDS. 1995;9:301-302.
3. Silverman S. Mycotic infections. In: Millard HD, Mason DK, eds. 3rd World Workshop on Oral Medicine. Ann Arbor: University of Michigan; 1998:87-96.
4. Xu YY, Samaranayake LP. Oral Candida albicans biotypes in Chinese patients with and without oral candidosis. Arch Oral Biol. 1995;40:577-579.
5. Scully C, El-Kabir M, Samaranayake LP. Candidosis. In: Millard HD, Mason DK, eds. 2nd World Workshop on Oral Medicine. Ann Arbor: University of Michigan; 1995:27-50.
6. Dreizen S. Oral candidiasis. Am J Med. 1984;77(4D):28-33.
7. Banoczy J, Rigo O, Albrecht M. Prevalence study of tongue lesions in a Hungarian population. Community Dent Oral Epidemiol. 1993;21:224-226.
8. Terai H, Shimahara M. Atrophic tongue associated with Candida. J Oral Pathol Med. 2005;34:397-400.
9. Gorsky M, Silverman S Jr, Chinn H. Clinical characteristics and management outcome in the burning mouth syndrome. An open study of 130 patients. Oral Surg Oral Med Oral Pathol. 1991;72:192-195.
10. Greenberg MS, Glick M, eds. Burket’s Oral Medicine: Diagnosis and Treatment. 10th ed. Hamilton, Ontario, Canada: BC Decker; 2003:95-105.
11. Siegel MA, Silverman S Jr, Sollecito TP, eds. Treatment of Common Oral Conditions. Hamilton, Ontario, Canada: BC Decker; 2001:4-5.
12. Bjorkegren K, Svardsudd K. Reported symptoms and clinical findings in relation to serum cobalamin, folate, methylmalonic acid and total homocysteine among elderly Swedes: a population-based study. J Intern Med. 2003;254:343-352.
13. Skoglund A, Sunzel B, Lerner UH. Comparison of three test methods used for the diagnosis of candidiasis. Scand J Dent Res. 1994;102:295-298.
14. Gorsky M, Silverman S Jr, Chinn H. Burning mouth syndrome: a review of 98 cases. J Oral Med. 1987;42:7-9.
15. Petti S, Tarsitani G, D’Arca AS. A randomized clinical trial of the effect of yoghurt on the human salivary microflora. Arch Oral Biol. 2001;46:705-712.
16. Hilton E, Isenberg HD, Alperstein P, et al. Ingestion of yogurt containing Lactobacillus acidophilus as prophylaxis for candidal vaginitis. Ann Intern Med. 1992;116:353-357.
Dr. Brown is a professor in the departments of Oral and Maxillo-facial Pathology and Oral Diagnosis and Radiology at Howard University College of Dentistry, Washington, DC, and a clinical associate professor in the Department of Otolaryngology at Georgetown University Medical Cen-ter, also in Washington, DC. He is past president of the American Academy of Oral Medicine. He can be reached at (202) 806-6100 or rbrown@howard.edu.
Dr. Bailey is an instructor in the Department of Restorative Dentistry at the Howard University College of Dentistry, Washington, DC. He can be reached at (202) 806-6100 or jbailey@howard.edu.
Dr. Winfree is an instructor in the Department of Restorative Dentistry at the Howard University College of Dentistry, Washington, DC. He can be reached at (202) 806-6100 or wwinfree@howard.edu.
Dr. Harden is an instructor in the Department of Restorative Dentistry at the Howard University College of Dentistry, Washington, DC. He can be reached at (202) 806-6100 or sharden@howard.edu.