INTRODUCTION
Surgical placement of dental implants has become routine for many general practitioners. With the advent of CBCT diagnosis and treatment planning, critical anatomy is understood and evaluated. Endosseous dental implants have come a long way with design improvements that perform at a high level and create excellent long-term prognoses. The surgical burs used to form the osteotomy sites are precise and predictable. With proper education and training, the GP can perform many surgical procedures to restore form and function to patients. Dental implants are simply pieces of titanium, which is a biocompatible material used by our orthopedic surgeon colleagues in knee and hip replacements. These orthopedic titanium replacements have a long-standing track record of integrating bone into the surface of the implant bodies.1
There are several criteria for a patient who requests dental implants. First, the patient must be relatively healthy, with no uncontrolled medical conditions that could affect healing around the dental implant. These include uncontrolled hypertension; uncontrolled diabetes; and immunosuppressive diseases, such as AIDS. The second criterion that must be considered is the amount of available hard tissue in the edentulous space. There must be adequate vertical height and width of bone to accept the proper size of the implant. A good rule of thumb is that the implant body chosen should be one-half the width of the edentulous space.2 This will maximize emergence profile and create a tooth restoration that will be both functional and aesthetic. However, horizontal width is often the limiting factor in choosing the size of the implant for this space. Bone grafting procedures are often needed to build available hard tissue to maximize the final result, or the final prosthesis may be compromised to some degree. This should be addressed with the patient prior to any surgical intervention.
 |
 |
| Figure 1. CBCT analysis (Green CT [Vatech America]) allows for concise evaluation of available hard tissue in the edentulous area. | Figure 2. The dental implant (Hahn Tapered Implant System [Glidewell]) is precisely positioned to maximize emergence profile. Because initial torque exceeds 25 Ncm, a taller healing abutment is positioned, eliminating the need for future anesthesia and tissue uncovering after the implant is integrated. This is referred to as a one-stage surgical procedure. |
The placement of dental implants has become rather routine for the practitioner, if not the patient. Because bone is not innervated, there are no pain receptors, so the soft-tissue site can normally be infiltrated with a local anesthetic. The practitioner will then decide whether to reflect the tissue to have visualization of the available bone or do a flapless procedure that allows the implant to be placed through the attached gingiva without reflection. CBCT analysis allows the dentist to visualize available anatomy and helps determine if a case is one that should be attempted without more invasive procedures. Once anesthesia is performed, the implant surgical kit allows for precise preparation of the implant osteotomy. In most systems, we start with a small-diameter pilot bur that is 2.4 mm in diameter. This bur is the most critical bur in the kit in that it provides angulation mesial-distally and facial-lingually. Depth is then determined using the apices of the adjacent roots as a guide. Because there is no blocking of the posterior site, only soft tissue is numbed. Any symptomatic reaction by the patient can be evaluated. The osteotomy site is prepared to proper angulation and depth, and the implant is torqued to place. Initial stability is created by the apical 2 mm of the implant.2 If initial torque exceeds 25 Ncm, then a healing abutment can be placed into the implant and torqued. This eliminates the need for secondary uncovering of the implant and anesthesia and is referred to as a one-stage surgical procedure. A tissue cuff is formed around the healing abutment, providing periodontal health. Once the implant has integrated, an impression of the internal design of the implant is made. Conventionally, an impression coping engages the implant, and the impression is made, usually with a polyvinylsiloxane material.
An open tray impression can be made where the impression tray is prepared so that the tall pin of the impression coping penetrates through the tray. The impression coping is thus removed with the impression. A closed tray impression is made when an impression coping engages the implant and the impression is made. Upon removal, the impression coping is necessarily unthreaded and then reinserted into the newly formed impression. The third and most popular method of making an accurate impression of the internal design of the integrated implant is using a scanning technique. The dental laboratory can then take the information gathered through conventional techniques or with the newest digital scan and create the final implant-retained prosthesis.3 This is normally done using CAD/CAM technology and milling.
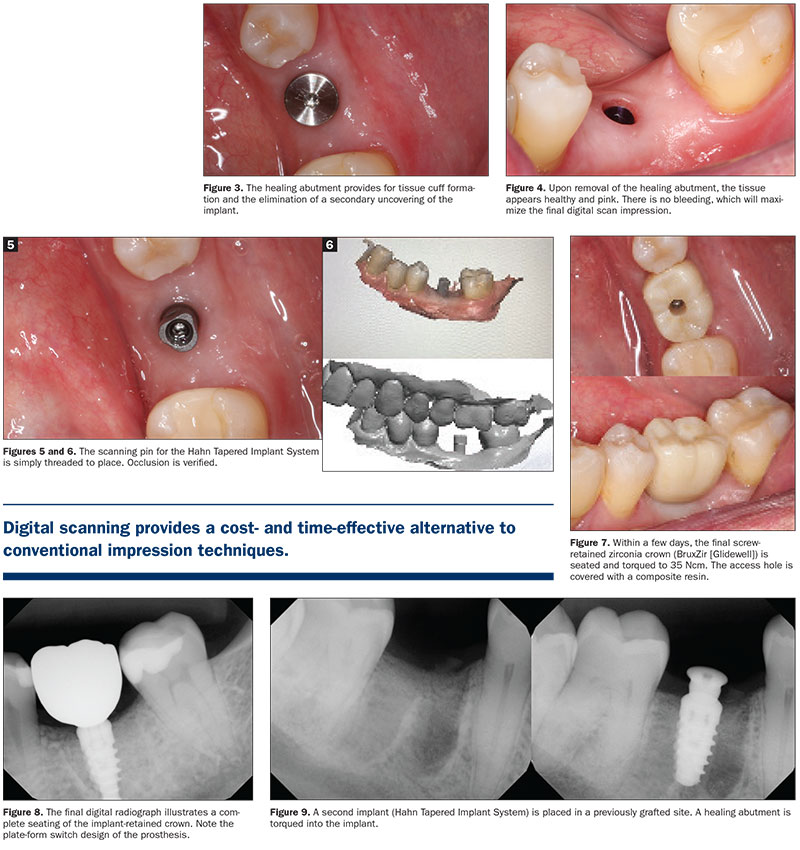 |
Digital scanning is an easy and efficient way to make a high-quality, accurate implant-level impression.4 Figure 1 illustrates CBCT analysis (Green CT [Vatech America]), which allows for concise evaluation of available hard tissue in the edentulous area. The dental implant (Hahn Tapered Implant System [Glidewell]) is precisely positioned to maximize the emergence profile. Because initial torque exceeds 25 Ncm, a taller healing abutment is positioned, eliminating the need for future anesthesia and tissue uncovering after the implant is integrated. This is referred to as a one-stage surgical procedure (Figure 2). The healing abutment provides for tissue cuff formation and the elimination of a secondary uncovering of the implant (Figure 3).
Upon removal of the healing abutment, the tissue appears healthy and pink. There is no bleeding, which will maximize the final digital scan impression (Figure 4). The scanning pin specific for the Hahn implant system is simply threaded to place (Figure 5). Occlusion is verified with the intraoral scanner (IOS) system (Figure 6). Within a few days, the final screw-retained zirconia crown (BruxZir [Glidewell]) is seated and torqued to 35 Ncm. The access hole is covered with a composite resin (Figure 7). The final digital radiograph illustrates a complete seating of the implant-retained crown. Note the plate-form switch design of the prosthesis (Figure 8).
A second implant (Hahn) is placed in a previously grafted site. A healing abutment is torqued into the implant (Figure 9). The healing abutment again provides for the formation of a healthy tissue cuff. Following integration, the healing abutment is removed, and the tissue is evaluated (Figure 10). Here, a closed tray impression coping is threaded into the implant, and a conventional polyvinylsiloxane material is used to impress the implant-level coping (Figure 11). Accuracy is critical for the laboratory to fabricate a proper implant-retained crown. The final screw-retained BruxZir zirconia crown is torqued to place, and the final digital radiograph is evaluated for a complete seat (Figure 12).
Using either conventional or optical scanning provides outstanding clinical aesthetic and functional results when the dental implants are properly positioned and integrated. Digital scanning provides a cost- and time-effective alternative to conventional impression techniques.
INTRAORAL SCANNING
Choosing the right intraoral scanning tool for predictable digital impressions can be a challenge. There are many high-quality products available that improve productivity using this technology. However, there needs to be a discussion on the return on investment.5 Certainly, conventional impression techniques are adequate to create crowns and bridges over our dental implants, but digital scanning may have advantages for the practitioner. Items to consider include the initial investment of the armamentarium, time savings during the procedure, the ability of the dental team to accept the technology and use it, and the response of our patients.6
Here we will discuss the use of the Medit i500 IOS. This open-system device can be used with all our dental laboratories. The initial investment is reasonable, and the initial training with the team is seamless. A conventional impression technique of a dental implant may take 4 to 6 minutes of impression set time. Scanning can reduce this time to just a couple of minutes. Scan bodies are unique to each individual implant system yet are readily available. Although the digital impression is electronically sent to my dental laboratory, there is still a cost savings when compared to milling my own implant crowns. The lab decreases the final crown and bridge cost as compared to mailing a conventional impression. Infection control is more streamlined, too, in that there is no need for the staff and dental laboratory to go through the process of sterilization. The practitioner needs to evaluate the cost savings of trays, impression materials, and packaging and shipping. Finally, not having to use impression materials in our patients’ mouths creates the patients’ positive response.7
 |
 |
| Figure 10. The healing abutment again provides for formation of a healthy tissue cuff. Following integration, the healing abutment is removed, and the tissue is evaluated. | Figure 11. Here, a closed tray impression coping is threaded into the implant, and a conventional polyvinylsiloxane material is used to impress the implant-level coping. Accuracy is critical for the laboratory to fabricate a proper implant-retained crown. |
 |
| Figure 12. The final screw-retained BruxZir zirconia crown is torqued to place, and the final digital radiograph is evaluated for a complete seat. |
Intraoral scanners have become a modern method of directly capturing crown and bridge and denture impressions. The rationale for their use includes accuracy, time efficiency, and simple clinical protocols that minimize discomfort for the patient. Accuracy is immediately determined, and the information is used for chairside milling or for virtual deposition to a dental laboratory. Digital designs can be created and approved.3-5 It is imperative that the site be digitally impressed and blood-free. Very deep margins can be challenging to duplicate. These optical impressions may reduce working time as compared to conventional impression techniques. This time saving can help to reduce the overall cost of any prosthesis. The time needed to design and fabricate is also reduced. Potentially, there is no sterilization of the impression material needed, no mailing costs, no stone model fabrication, and no trimming of dyes. Chairside milling provides the patient fast and efficient delivery of his or her prosthesis and eliminates the need for transitional restorations. Obviously, there is a learning curve with this technology, so an integrated team process is required. The more optical scans that are done, the easier they become.6,7 Any errors can be immediately evaluated, digitally deleted, and redone. Quality of the final prosthesis is paramount to a successful restoration and patient satisfaction. Scanning and digital design has proven to be a most efficient technique. Patients can also be directly involved with this technology, which has proven to be an excellent internal marketing tool. The initial investment seems to be the biggest hurdle in accepting this technology into one’s practice.8-11 Upgrades may be required in the future. Open systems, meaning that any dental laboratory can use the information created, may be important for some clinicians. The practitioner needs to be aware of any additional costs of providing this service.
Accuracy is the primary reason to incorporate this technology into our dental practices. Accuracy is defined as “the sum of trueness and precision.”4 Trueness is defined as the “closeness of agreement between the expectation of a test result or a measurement result and a true value.” Precision is defined as “closeness of agreement between indications or measure quantity values obtained by replicate measurements on the same objects under specified conditions.” The literature seems to agree that scanned impressions are similarly accurate to conventional impression techniques.5
CONCLUSION
The Medit i500 IOS is a cost-savings tool that is easily incorporated into dental therapy. The cost of this open system device is reasonable and includes 12 hours of continuing education and training. Productivity is improved. It has a small footprint and fast optical scanning speed and can be used for single, multiple, and full-arch impressions. It is a powderless system. Vivid colors distinguishing soft tissue, plaque, and teeth create high-resolution images. The internal design of any implant system is captured using scanning abutments particular to each type of fixture. For impressions of natural teeth, margin lines can be created automatically or manually. Occlusion is accurately determined using an analysis function. A color map indicates the degree of occlusion requested.
Using scanned impressions appears to have several significant advantages over our conventional polyvinylsiloxane materials. Patient responses have been outstanding, creating interest in our techniques, saving time in the process, minimizing gagging, and reducing patient anxiety. Design communication is improved with both the patient and the dental laboratory technician.
References
- Misch CE. Contemporary Implant Dentistry. 3rd ed. St. Louis, MO: Mosby Elsevier; 2008.
- Kosinski TF. Placing implants in sites lacking keratinized tissue. Inside Dentistry. October 2017; Inside Implants: 42-50.
- Mangano F, Gandolfi A, Luongo G, et al. Intraoral scanners in dentistry: a review of the current literature. BMC Oral Health. 2017;17(1):149. doi:10.1186/s12903-017-0442-x
- Ting-Shu S, Jian S. Intraoral digital impression technique: a review. J Prosthodont. 2015;24(4):313-21. doi:10.1111/jopr.12218
- Zimmermann M, Mehl A, Mörmann WH, et al. Intraoral scanning systems — a current overview. Int J Comput Dent. 2015;18(2):101-29.
- Imburgia M, Logozzo S, Hauschild U, et al. Accuracy of four intraoral scanners in oral implantology: a comparative in vitro study. BMC Oral Health. 2017;17(1):92. doi:10.1186/s12903-017-0383-4
- Ahlholm P, Sipilä K, Vallittu P, et al. Digital versus conventional impressions in fixed prosthodontics: a review. J Prosthodont. 2018;27(1):35-41. doi:10.1111/jopr.12527
- Schepke U, Meijer HJ, Kerdijk W, et al. Digital versus analog complete-arch impressions for single-unit premolar implant crowns: operating time and patient preference. J Prosthet Dent. 2015;
114(3):403–6.e1. doi:10.1016/j.prosdent.2015.04.003 - JJoda T, Brägger U. Digital vs. conventional implant prosthetic workflows: a cost/time analysis. Clin Oral Implants Res. 2015;26(12):1430–5. doi:10.1111/clr.12476
- Joda T, Lenherr P, Dedem P, et al. Time efficiency, difficulty, and operator’s preference comparing digital and conventional implant impressions: a randomized controlled trial. Clin Oral Implants Res. 2017;28(10):1318-1323. doi:10.1111/clr.12982
- Mandelli F, Ferrini F, Gastaldi G, et al. Improvement of a digital impression with conventional materials: overcoming intraoral scanner limitations. Int J Prosthodont. 2017;30(4):373-376. doi:10.11607/ijp.5138
Dr. Kosinski received his DDS degree from the University of Detroit Mercy School of Dentistry (Detroit Mercy Dental) and his Mastership in Biochemistry from the Wayne State University School of Medicine. He is an affiliated adjunct clinical professor at Detroit Mercy Dental, currently serves as the associate editor of the AGD journals, and was recently named implants editor at Dentistry Today. He is a past president of the Michigan Academy of General Dentistry. Dr. Kosinski is a Diplomate of the American Board of Oral Implantology/Implant Dentistry, the International Congress of Oral Implantologists (ICOI), and the American Society of Osseointegration. He is a Fellow of the American Academy of Implant Dentistry and received his Mastership in the AGD. He can be reached at drkosin@aol.com.
Disclosure: Dr. Kosinski reports no disclosures.
Related Articles
Proper Preparation for Prosthetically Driven Implants: CBCT Diagnosing and Surgical Protocol
Creating an Autogenous Graft From Extracted Teeth: A Faster Implant Integration Time
Trephine Removal of a Damaged Implant











