Today’s dental practices are seeing a substantial amount of hemorrhaging, and I’m not just talking about bleeding gums. Dental practices’ profits are hemorrhaging from last-minute hygiene appointment cancellations and countless missed opportunities in the nonsurgical periodontal treatment profit center. Far too many patients are receiving just a prophy when they really need nonsurgical periodontal therapy or periodontal maintenance (also known as supportive periodontal therapy [SPT]). Many dental professionals are aware of this but don’t know how to step off the daily prophy treadmill, evaluate and communicate the need for periodontal maintenance, and the kicker, convince the patient to embark on this journey for supportive preventive and nonsurgical periodontal therapy. Some dental offices will even avoid doing nonsurgical periodontal treatment and routine SPT appointments because they don’t understand how to code the procedure for insurance payment, and they don’t want to deal with chasing down a patient for money when insurance won’t pay for it.
Patients themselves add to the challenges of scheduling dental hygiene preventive care and SPT appointments. The average patient is either unaware of his or her need for routine SPT appointments or chooses to forego scheduling regular dental hygiene appointments. Patients’ financial stresses are an ever-increasing reason for cancelled appointments, but simply not knowing the importance of regular preventive care and routine SPT appointments is the major tipping point of patients saying no to the treatments they need. Most patients won’t say yes to a simple supportive therapy to prevent disease when they don’t understand the valuable health benefits (Table 1).
Do these issues sound all too familiar in today’s world of dentistry? Is your dental office hemorrhaging and feeling the same pain? The good news: Today, thousands of dental practices are sitting on an untapped gold mine worth thousands of dollars annually in profits to the dental hygiene department—and that gold mine comes straight from those patients whose mouths are literally hemorrhaging from periodontal disease. Nonsurgical periodontal treatment is only one of several profit centers in the dental hygiene department. If you can imagine the possibility of growing just this one profit center, usually by thousands of dollars, imagine the glowing potential of your entire practice and the value that you will bring as a member of the dental team.
| Table 1. How Cancellations Will Cause Your Practice to Lose Income | ||||||||||||||||||||||||||||||
aAny production number varies by fees charged in your area.
bAverage of approximately $1,000/day of patient restorative treatments on doctors’ schedules should come from the hygiene treatment room daily. From the example above, due to cancellations in the hygiene department, the lost income for the practice is $280,000! |
Now that we know the common barriers to getting a yes to the proper treatment plan, the goal of this article is to show you creative ways to overcome these barriers. In doing so, you will play a huge role in growing the nonsurgical periodontal treatment profit center in the dental hygiene department. So how do you get your patients to say yes to optimal health?
ARM YOURSELF WITH THE SCIENCE
The latest research and science behind periodontal disease is your biggest tool to convince a patient to begin—and stick with—preventive and SPT appointments. The first step is to clearly understand the information behind your case to the patient. The following are key points about periodontal disease to have in your toolbox when you talk to patients.
Periodontal disease is an inflammatory disease that affects the soft and hard tissues that support the teeth. The early stage of this disease is gingivitis. In later stages, the teeth may become loose, and the bone surrounding the teeth can degenerate. The most advanced stage of periodontitis is termed chronic periodontitis.1 Major risk factors for this disease include an inherited or a genetic predisposition, smoking, lack of routine home care, age, diet, certain systemic diseases, and various medications.2
Any time bleeding is present, pathological change is occurring in your patient’s mouth that needs to be evaluated and appropriately treated sooner rather than later. When periodontal disease is present, the potential for bone loss has already begun. Depending upon the patient’s risk factors, bone loss can occur quickly and become aggressive very easily. In patients with few or no risk factors, periodontal disease can be reversed with early nonsurgical intervention.3 With this knowledge, a patient will be much more likely to say yes to your treatment plan.
Phase 1 treatment is complete after the patient undergoes scaling and root planing, followed by a successful postoperative report from the 6-week re-evaluation appointment. This 6-week re-evaluation appointment is the first of the SPT appointments. During the early stage of periodontal disease and at the end of phase 1, the periodontium has the best chance to reverse the diseased state and, in many cases, halt the progression of further oral and systemic disease. Patients need to know, however, that this is not the end of the story. After phase 1 therapy is complete, a patient is now and forever considered a periodontal patient, which means regular SPT is a must to prevent active disease. A regular prophy just won’t do. If your patient were to ask, alternating prophylaxis appointments with SPT appointments is not appropriate and should not be considered as an appropriate phase for future treatment. Bone loss is not reversible, and it is imperative that patients understand this. Removal of the biofilm and microbiological factors also becomes very important for future health of the patient.4
For years, we have understood that periodontal disease is episodic. Make sure your patients understand what that means. It is another key point to use when explaining why regular periodontal maintenance is crucial. Periodontal pathogens will repopulate a healthy and recently scaled sulcus as early as 9 to 12 weeks post-scaling.5 That means a patient can brush and floss all day long, or even see the dental hygienist every 3 months; yet this may not be enough to prevent the return of periodontal pathogens. Without these pathogens removed, bone loss is likely to continue. Other clinical studies have shown that even with the supragingival environment as the single source for colonizing bacteria, a complex subgingival microbiota can develop within one week.6
You can strengthen your case for preventive care even more when your patient is aware that oral health affects the whole body. Countless studies have emerged during recent years suggesting a strong link between periodontal health and systemic health. For example, when patients with Crohn’s disease receive the appropriate treatment for periodontal disease, research reports a decrease in the enzymes that would normally increase inflammation in the sulcus—and the body.7 In addition, much research states that when a patient with type 2 diabetes mellitus is diagnosed with periodontal disease, nonsurgical periodontal therapy was associated with improved glycemic control.8 The role of the dental hygienist becomes extremely valuable when patients’ teeth are not merely “cleaned.” Scaling, root planing, and various adjunct chemotherapeutic intervention along with lasers can improve a patient’s oral health8,9 and thus may actually help a patient live a longer, healthier life.
Your chances of getting a yes to nonsurgical periodontal therapy and routine SPT appointments will increase when patients understand the vital link between their oral health and systemic health. On that note, what’s even more effective is to share science’s good news. Decades of research and advances in periodontal therapy have proven that the majority of patients who receive routine preventive care can retain their dentition throughout their lifetimes.10 Many patients who do routine, long-term, supportive, nonsurgical therapy can maintain optimal gingival health that is free from reinfection.
If you have your patients’ attention at this point, they will probably want to know how often they need to come in for periodontal therapy. Although each patient will need an individualized treatment plan, dental hygiene appointments for routine preventive care will ideally range from 2- to 6-month intervals.11 Presenting the scientific evidence to patients takes good communication, and their understanding will leap forward, giving them a reason to sit up, listen, and take action, saying, “Yes!” to case acceptance of nonsurgical periodontal treatment.
LEAVE A LASTING IMPRESSION WITH STELLAR PATIENT EDUCATION
Now, you must bridge the gap between the hard science and your patients. So that you don’t overwhelm patients with heaps of unorganized scientific facts from your stream of consciousness, use a 3-step approach to present the information in support of your argument to partake in routine supportive periodontal therapy.
First, give patients the disease facts, focusing on tooth/bone loss and systemic health. This is also a good time to discuss risk factors for periodontal disease. Effectively communicate using words your patients will understand when you talk about the periodontal disease process. Not only is tooth loss a fact in their future, but also their health and longevity is at stake if they do not follow the appropriate treatment plan. Back up your facts with brochures, posters, iPad apps, etc, to show patients the importance of optimal oral health in relationship to their total overall health. Mention the risk factors and systemic disease links and highlight their specific risk factors in the information they will take home with them. Explain the complications that arise when periodontal health declines—and explain how easily this can happen without proper treatment and regular supportive periodontal therapy.
Second, when a diagnosis is established that calls for something other than a prophy, take the time to describe the treatment plan with your patients. Outline the treatment process with patients, step by step. You might even share with them a visual aid that shows the drastic difference between a prophy and periodontal therapy, or healthy versus diseased gums, such as the chart12 in Table 2 (Figures 1 to 13). To enhance an engaging communication process, ask open-ended questions, such as, “How do you feel about this treatment approach?” and “What are your concerns?” Then, invite the patient to ask questions. This is all part of the buy-in.
Finally, explain that periodontal disease is episodic and what that means.13 Tell patients that from this point forward, they need to return every 12 weeks, or at frequent, appropriate intervals when SPT is required. Explain that patients may appear healthy for many years after completing scaling and root planing, but the disease process can return at any time. Occasionally, patients may need to go from supportive periodontal therapy back to scaling and root planing. This is an example of the episodic process of periodontal disease, specifically when patients have certain risk factors.
Even with a 3-step approach, talking science isn’t always easy, but there are some creative ways to deliver a powerful message to your patients. Begin by sitting down as a team to discuss and understand the various personality styles of your patients. Then, develop scripts and practice a dialogue between the hygienist and various types of patients. Understand what words are important to your various types of patients and what may be considered hot buttons for your patients. For example, words such as “irreversible,” “tooth loss,” “bone loss,” “pus,” etc, are likely to grab their attention. Remember to take out words such as “cleaning” from your vocabulary with patients, and use words such as “preventive care,” “supportive therapy,” or “periodontal maintenance.” Know the various types of words you can use with your individual patients, their health IQ, and their different personality styles when you communicate with them.
Know what motivates your patients. For instance, cosmetic issues are a huge motivator for many. If these patients understand that tooth loss or unsightly teeth and gums are in store for them, they might ask you to schedule an appointment right away. Other patients are motivated by health issues, so one of your scripts might be for the “health-conscious person.” Another example is the patient motivated by money. At first, suggesting periodontal therapy may sound counter-productive to this kind of patient, but if you take a preventive angle, you can explain that the patient will save a lot of money in the long run by avoiding costly surgeries and other systemic health complications that may require numerous doctor appointments, pharmaceuticals, and even hospital visits.
Also take time with your team to list all the possible reasons a patient might say no. Then, brainstorm creative ways to counter the argument from your patient. Brainstorm as many personality types as you can, what motivates them, and push those buttons with them. After writing your scripts, practice with each other before you begin this new method of effective communication.
Alongside your script writing, brush up on your scientific knowledge and your ability to deliver it in everyday language. Have each member of the hygiene team bring in information about periodontal disease, risk factors, the oral health-systemic link, etc, and present a few key findings in 5 minutes or less, without looking at notes. Remember, you’re practicing for face time with a patient in a conversational situation. If you have only one hygienist, ask other teammates to participate in this exercise. Set a goal for everyone on the team to understand and embrace how treatment of periodontal disease can benefit a patient and mitigate various risk factors.
Many patients relate well to understanding the science. Some patients will want to know all the details about the disease, the treatment, and cause of this oral health challenge. Because of this, it can be valuable to have the hygiene team educate the entire team about subgingival recolonization of bacteria. Your team may want to spend some time with your local periodontist to learn about how subgingival microflora changes over time. At the same time, you can learn what your local periodontist expects from your office, when to refer, and when the periodontist wants to see a patient. This is another relationship-building opportunity. Set a goal for everyone on the team to truly understand the science and the oral-systemic link. Bottom line: every team member needs to be able to effectively explain the periodontal process and treatment goals to patients.
In addition, take time with your team to discuss your current patient needs. Create various scenarios, including real-life patient situations, and role play as a team. In this exercise, evaluate and discuss your team’s strengths and weaknesses in communicating the appropriate information. Practice until you are certain your communication skills will help patients understand what they need to do to be healthy and what it takes to get a yes to case acceptance.
The takeaway: You can educate your patients to a higher oral health IQ when you follow these suggestions—and you will get more patients to answer yes to the correct treatment plan. As a result, you will spend less time doing nonproductive scaling and have more time for other services that add profits to the practice and wow your patients. This is the true value of a dental hygiene appointment and providing more than “just a cleaning.”
| Table 2. Healthy Periodontium Versus Diseased Periodontium14 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
BREAK THROUGH THE FINANCIAL BARRIERS
The expense of completing treatment, for many patients, is the biggest obstacle to moving forward with treatment. Many insurance plans do not cover the periodontal maintenance appointment at less than 6-month intervals. Here is a secret, though, that will unlock the door to successfully getting a yes from a patient: Most people will find a way to buy what they really want. People talk left and right about these “hard economic times,” yet many of these same people carry smartphones, dine out regularly, and participate in expensive hobbies, such as skiing, golf, fly fishing, etc. I am not suggesting that true financial struggles do not exist for some people, but you may be surprised what people can pull out of the woodwork when they consider a certain financial item to be high priority.
How do you get patients to move their scaling, root planing treatment, and their SPT visits high up on their financial priority list? Effective communication skills will help you overcome patients’ financial barriers to accepting nonsurgical periodontal treatment, as well as your other treatment recommendations. Nonsurgical periodontal therapy can be very costly, so be prepared to take time with the patient to discuss the financial aspects privately. This is the perfect time to introduce the patient to your financial coordinator. Perhaps your office has several payment plans available to offer patients. These can create an easier opportunity to get them to say yes to scheduling treatment.
 |
 |
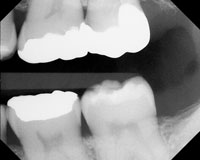
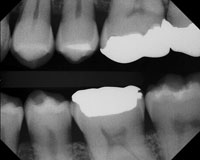
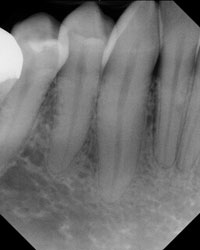
| Figure 14. First in a series of bite-wing x-rays. | Figure 15. Advanced bone loss on maxillary arch and mandibular arch, including furcation area of lower molar. |
 |
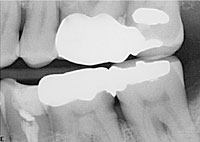 |
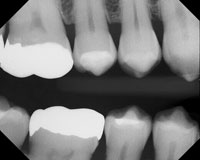
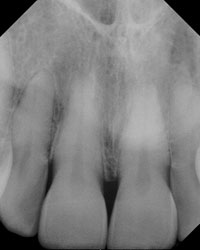
| Figure 16. Horizontal and vertical bone loss on maxillary arch; horizontal bone loss on lower molars. | Figure 17. Bone loss on maxillary arch between bicuspids and molar, in addition to mandibular march between first and second molar, distal on the second molar, and in furcation area of the second molar. |
Although not every patient will say yes to his or her treatment plan at the time it is presented, always schedule another time to follow up. For example, the auxiliary at the front desk should ask, “Mrs. Jones, may I call you on Thursday [no more than 2 days later] to follow up with your treatment plan?” If Mrs. Jones declines, ask when would be a good time to follow up. If all else fails, the front desk auxiliary needs to schedule a date in a week or 2 and write it on the office calendar to follow up. When follow-ups do not occur, these patients get lost in the system until their next dental hygiene appointments—possibly 6 months away or even a year, if they are prone to skipping and canceling hygiene appointments. Remember, always create value around the benefits of treatment, why patients need treatment completed sooner rather than later, and how it will personally benefit them.
Finally, pictures are worth a thousand words. While patients are in the treatment room or the consult room, show their radiographs as a visual when discussing their treatment. Point out the calculus and bone loss (Figures 14 to 17). If you have an intraoral camera, take a picture of bleeding and staining, calculus, and any suppuration. Use these intraoral photographs to show patients their areas of disease. If you don’t have the technology to provide photos, give patients a hand mirror and show them where their gums are bleeding or exactly what is happening in the oral cavity. Perhaps the one fact to surely get patients’ attention is the potential for tooth loss. Show them actual tooth mobility if it exists. Visuals can be a powerful and emotional tool. This may be the catalyst you need, causing patients to encounter an emotional belief that a change in their oral condition is necessary. They are more likely, now, to schedule treatment.
REAP THE REWARDS OF YOUR HARD WORK
Dental hygienists have an important role in prevention of disease. This role can create a sense of purpose that takes the burn out of showing up for “just a job.” Dental hygienists who take pride in educating patients about their oral healthcare needs, support patients to establish preventive goals, and educate patients about their home care preventive routines establish trusting relationships with their patients and appear to greatly enjoy their careers.
Meanwhile, the members of the dental team feel the financial rewards when the practice begins tapping into that gold mine right under their feet. Suddenly, the stress of losing jobs, pay cuts, downsizing, or even closing the practice begins to lift. If you’re lucky, you may even see pay raises and bonuses that have been nonexistent since the economic downturn. Perhaps there will even be enough wiggle room to hire that much-needed hygiene assistant.
What creates success is passion and excitement. When the team is passionate and excited to see oral changes go from negative to positive, this enthusiasm flows into patients’ attitudes as well. Patients will become passionate and are more certain about returning for routine preventive care and periodontal maintenance appointments in the future. I wish you the best of luck in educating your patients and getting them in the front door for the treatment they most need!
References
- American Academy of Periodontology. Types of gum disease. perio.org/consumer/2a.html. Accessed February 1, 2012.
- American Academy of Periodontology. Periodontal disease fact sheet. perio.org/consumer/disease_facts.htm. Accessed February 1, 2012.
- National Institute of Dental and Craniofacial Research. Personal and provider approaches to oral health. In: Oral Health in America: A Report of the Surgeon General. nidcr.nih.gov/datastatistics/surgeongeneral/sgr/chap8.htm. Accessed February 1, 2012.
- Offenbacher S, Barros SP, Singer RE, et al. Periodontal disease at the biofilm-gingival interface. J Periodontol. 2007;78:1911-1925.
- Mousquéegs T, Listgarten MA, Stoller NH. Effect of sampling on the composition of the human subgingival microbial flora. J Periodontal Res. 1980;15:137-143
- Quirynen M, Vogels R, Pauwels M, et al. Initial subgingival colonization of ‘pristine’ pockets. J Dent Res. 2005;84:340-344.
- Stein JM, Lammert F, Zimmer V, et al. Clinical periodontal and microbiologic parameters in patients with Crohn’s disease with consideration of the CARD15 genotype. J Periodontol. 2010;81:535-545.
- Lang NP, Tonetti MS, Suter J, et al. Effect of interleukin-1 gene polymorphisms on gingival inflammation assessed by bleeding on probing in a periodontal maintenance population. J Periodontal Res. 2000;35:102-107.
- Drisko CH. Non-surgical pocket therapy: pharmacotherapeutics. Ann Periodontol. 1996;1:491-566.
- Hancock EB, Newell DH. Prevention strategies and supportive treatment. Periodontol 2000. 2001;25:59-76.
- Cohen RE; Research, Science and Therapy Committee, American Academy of Periodontology. Position paper: periodontal maintenance. J Periodontol. 2003;74:1395-1401.
- Socransky SS, Haffajee AD, Goodson JM, et al. New concepts of destructive periodontal disease. J Clin Periodontol. 1984;11:21-32.
- Wilkins EM. Clinical Practice of the Dental Hygienist. 10th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2009.
Ms. Seidel-Bittke is an international speaker, author, and one of Dentistry Today‘s Leaders in Dental Consulting. She is president of Dental Practice Solutions, a dental practice management business specializing in patient-centered solutions, uncovering hidden office potential and maximizing profits. Ms. Seidel-Bittke seamlessly combines her sharp knowledge of the latest dental hygiene science, financial savvy, and her knack for solving the toughest dilemmas of the dental team to put even the most struggling dental practices on the fast track to success. She can be contacted at (888) 816-1511, via e-mail at info@dentalpracticesolutions.com, or via the Web site dentalpracticesolutions.com.
Disclosure: Ms. Seidel-Bittke is owner of Dental Practice Solutions.