Ceramic veneers have become a mainstay of aesthetically oriented dental practices. They provide a conservative option to restore or enhance a patient’s dental and facial appearance with far less tooth removal compared with full coverage restorations.1 Available data indicate that veneers demonstrate high long-term success,2-5 and even recover the original strength of the supporting teeth.6 Preparation protocols have evolved to optimize aesthetics, reduce preparation complexity, increase retention and minimize tooth reduction. In addition, current bonding agents result in highly retentive restorations that reduce the need for technically complex, mechanically retentive elements in preparation design.
CASE REPORT
Diagnosis and Treatment Planning
 |
 |
|---|---|
|
Figure 1. Preoperative photo of patient’s smile. Note unaesthetic appearance. |
Figure 2. Retracted preoperative view. |
 |
 |
|
Figure 3. Diagnostic casts allowed for a more exacting evaluation. |
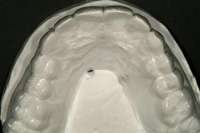
Figure 4. From the occlusal perspective, the maxillary incisors were found to be canted to the distal. |
 |
 |
| Figure 5. Tooth dimensions were accurately measured with a digital caliper. |
Figure 6. Diagnostic wax-up, duplicated in stone, served as the blueprint for the definitive restorations. |
 |
|---|
|
Figure 7. A clear vacuum-formed matrix from the cast of the diagnostic waxing served as a guide to crown lengthening procedures and to gauge preparation depth. |
Critical to patient satisfaction with definitive veneers is the dentist’s thorough evaluation of the patient’s motivation for seeking treatment, and an understanding of the patient’s own vision of the anticipated result.7 An oral examination, including the necessary radiographs and a determination of the feasibility for achieving the desired result, should follow the initial discussion.
Preoperative Referrals to Specialists
 |
|---|
|
Figure 8. Crown lengthening dramatically resulted in more proportionate tooth dimensions and corrected the “gummy” appearance. |
Orthodontics and periodontics are often adjunctive specialties prior to rehabilitation with veneers. Coordination between these specialists and the restorative dentist (or prosthodontist) should begin early in the process to plan for ideal spacing, tooth size and proportions. Aesthetic correction might be completed entirely by orthodontic treatment and is the treatment of choice for misaligned teeth.8 Disproportionately small teeth resulting in diastemas, peg lateral incisors, discolored teeth, worn teeth and unaesthetically shaped teeth are not amenable to orthodontics alone, and veneer restorations may be necessary for aesthetic refinement.9 Periodontal procedures should also be considered to improve tooth proportions. This can be done primarily by crown lengthening10 to reduce a gummy smile or to balance gingival architecture (Figure 8). These specialists should be part of the interdisciplinary team and their treatment must be completed, and the tissue matured, before restorative therapy begins.
Bur Selection: Understanding Bur Dimensions
 |
|---|
|
Figure 9. PriestPros Crown, Bridge, and Veneer Kit LD 0146 (KOMET USA). |
Standardized restorative protocols are the keys to efficiency and for consistently achieving successful ceramic veneers. Over years of refining preparation techniques, the author has assembled a small but effective set of diamond burs (PriestPros Crown, Bridge, and Veneer Kit LD 0146 [KOMET USA]) that is applicable to patients’ diverse veneer and crown indications (Figure 9). Rather than selecting individual burs and arranging them in a bur holder for each patient, several of these preset and autoclavable bur kits are available for immediate use. The kits consist of 3 super-coarse, tapered, rounded shoulder diamonds (T5856.018, 016, and 014) and 3 finishing diamonds of the same shape (8856.018, 016, and 014). Two football-shaped diamonds, coarse (6379.023), and fine (8379.023), are also included for palatal or occlusal reduction during crown preparation.
- Worn, aged teeth often require less tooth preparation than younger teeth.
- Misaligned teeth require more or less preparation depth predicated upon the anticipated tooth form and position of the planned restorations.
- Alternations in widths and heights of existing teeth vary the amount of preparation required.
 |
|---|
|
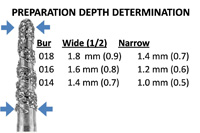
Figure 10. By knowing each bur’s widest and narrowest diameters, from shank to tip, the dentist can prepare specific depths for each individual tooth. |
By planning the anticipated form of the final restorations, knowledge of each bur’s widest and narrowest diameters from shank to tip allows the dentist to prepare specific depths for each individual tooth (Figure 10). It should be noted, however, that regardless of the technique used, some subjectivity remains regarding preparation depth.12 By knowing bur diameters, if the preparation depth needed in the incisal half is 0.7 mm, the T5856.014 bur is 1.4 mm at its widest dimension. Preparation to one-half the depth of that bur provides the requisite 0.7 mm.
Tooth Preparation Protocol
A cast of the diagnostic wax-up, a vacuum-formed matrix, and a silicone matrix should be accessible during tooth preparation. The wax-up and vacuum matrix aid in tooth preparation depth, and the silicone matrix is used for making a provisional restoration. In the patient example illustrated herein, all attempts have been made to be as conservative as possible, but minimal/no-prep veneers for all the involved teeth would not result in an optimal aesthetic result. The teeth were already facially prominent and the winged central incisors required increased tooth reduction on the distal aspects.13,14 Absolute gingival health was of functional and aesthetic importance for this patient, since she presented with a high smile line. A gingival finish line, therefore, was required to ensure smooth tooth-veneer transitions for optimum gingival health and color.15,16
 |
 |
|---|---|
|
Figure 11. Tooth preparation began on the facial surface of the maxillary central incisor with the T5856.018 diamond bur. |
Figure 12. Depth cuts were shallow on the mesial aspect and progressively deepened towards the distal. |
 |
 |
|
Figure 13. Depth cuts were blended mesiodistally and gingivoincisally, and then the proximal extensions were completed with the T5856.014 thin tapered rounded-shoulder diamond bur. |
Figure 14. Incisal reduction, predicated on the anticipated incisal length, was initiated with the T5856.018 super-coarse, large bur and blended over the incisal preparation for a smooth transition. |
 |
 |
|
Figure 15. Finishing diamonds of the same sizes were used to finish the preparations. |
Figure 16. Preparation for smaller teeth, like lateral incisors, was initiated with the smaller T5856.014 diameter diamond burs. |
 |
 |
| Figure 17. For posterior teeth, the chamfer preparation was extended one-half the distance down the palatal incline of the buccal cusp. |
Figure 18. Preparation depth was checked with the vacuum matrix from the cast of the diagnostic wax-up. |
 |
|---|
|
Figure 19. A single continuous piece of retraction cord was placed before impression making. |
Preparation of the teeth is illustrated in Figures 11 to 17. The larger T5856.018 diamond was used first to begin preparation of the central incisors. Several depth cuts from gingival to incisal were made predicated on the anticipated position of the veneers. These depth cuts were then blended together both mesiodistally and incisogingivally. Using the diamond’s diameter as a guide, approximately 0.4 mm enamel was removed from the mesioincisal aspect of the central incisors and 0.8 mm from the distoincisal aspects. Thin super-coarse T5856.014 diamonds were used to accomplish proximal reduction between teeth to avoid over preparation. Incisal reduction was completed next based on the anticipated incisal edge length to allow 1.5 mm thickness of porcelain.11 The incisal preparation should be a butt joint at a right angle to the palatal surface of the tooth and should transition smoothly from the incisal to the facial contour of the preparation.
Provisional Veneer Restorations
 |
 |
|---|---|
|
Figure 20. Bis-acryl resin was injected into the silicone matrix then seated intraorally for the prescribed amount of time. |
Figure 21. Metal-impregnated rubber wheels and knife-edge disks were used to finish the provisional restoration. |
A silicone matrix of the diagnostic wax-up was used for fabrication of the provisional veneer restorations because it provides more detail than a typical vacuum-formed matrix.17 A bis-acryl resin (Structure Premium [VOCO]) of appropriate shade was injected into the matrix (Figure 20), seated over the preparations and removed in one piece after complete setting. Flowable composite resin (GrandioFlo [VOCO]) was then used to fill in any voids and the provisional restoration was trimmed with a rubber polishing knife-edge disc and wheel (Universal Polishers 9627 and 9554 [KOMET USA]) (Figure 21), and then finished with a wet slurry of flour of pumice. Self-etching cement (RelyX Unicem [3M ESPE]) was used to seat the provisional veneers (Figure 22).18
Delivery of the Definitive Restorations
 |
 |
|---|---|
|
Figure 22. The provisional restoration was seated with self-etching cement. |
Figure 23. Anterior dies demonstrated a transition over the incisal edge to a butt joint and the premolar illustrated a continuation of the chamfer over the buccal cusp. |
 |
 |
|
Figure 24. Precise fitting feldspathic veneers were predicated on the original diagnostic waxing. |
Figures 25. Proportionate veneers with a rejuvenated color contributed to the patient’s enhanced smile. |
 |
 |
|
Figure 26. Gingival health was maintained by using a small gingival chamfer to create a seamless tooth and ceramic interface. |
Figure 27. Following occlusal refinement, the margins blended smoothly with the palatal tooth structure. |
Dies were sectioned and finish lines demarcated. Anterior dies demonstrated an incisal butt joint extending to the palatal surface and chamfers on the occlusal cusps were evident on posterior teeth (Figure 23). An implant replaced the maxillary left second premolar. The dies illustrate smooth, confluent finish lines devoid of sharp angles and depict the differences in anterior and posterior tooth preparation. The transition over the incisal edge of an anterior tooth (canine) rounds over the incisal edge to a butt joint, whereas the transition for a posterior tooth (first premolar) continues smoothly from the proximal to the occlusal aspect as a chamfer. Preparation design facilitated feldspathic veneers that precisely fit the dies (Figure 24).
CONCLUSION
Ceramic veneers are an integral part of a restorative dentist’s treatment portfolio that can make a dramatic difference in a patient’s smile and self-esteem. Clinicians, however, are faced with the objective of removing as little tooth structure as possible without compromising the anticipated aesthetic outcome. Understanding the patient’s specific aesthetic needs is the first key to treatment success. A thorough evaluation of the patient’s dentition by direct examination, by digital images and following diagnostic waxing then set the stage for tooth-specific veneer preparation. Familiarization with the diameters of preselected diamond bur kits provides dentists with the means to remain conservative while preparing each tooth to the appropriate depth for the planned veneer. The resulting veneer restorations should provide optimum aesthetics, healthy periodontal tissues, and predictable longevity.
Acknowledgement
I gratefully acknowledge the technicians of Georgia Dental Laboratory and their commitment to prosthetic excellence.
References
- Edelhoff D, Sorensen JA. Tooth structure removal associated with various preparation designs for anterior teeth. J Prosthet Dent. 2002;87:503-509.
- Dumfahrt H, Schäffer H. Porcelain laminate veneers. A retrospective evaluation after 1 to 10 years of service: Part II—Clinical results. Int J Prosthodont. 2000;13:9-18.
- Fradeani M, Redemagni M, Corrado M. Porcelain laminate veneers: 6- to 12-year clinical evaluation—a retrospective study. Int J Periodontics Restorative Dent. 2005;25:9-17.
- Layton D, Walton T. An up to 16-year prospective study of 304 porcelain veneers. Int J Prosthodont. 2007;20:389-396.
- Magne P, Perroud R, Hodges JS, et al. Clinical performance of novel-design porcelain veneers for the recovery of coronal volume and length. Int J Periodontics Restorative Dent. 2000;20:440-457.
- Magne P, Douglas WH. Porcelain veneers: dentin bonding optimization and biomimetic recovery of the crown. Int J Prosthodont. 1999;12:111-121.
- Javaheri D. Considerations for planning esthetic treatment with veneers involving no or minimal preparation. J Am Dent Assoc. 2007;138:331-337.
- Spear FM. The esthetic correction of anterior dental mal-alignment: conventional vs. instant (restorative) orthodontics. J Calif Dent Assoc. 2004;32:133-141.
- Lowe E, Rego J, Rego N. Minimally invasive dentistry combining orthodontic therapy and single-unit restoration. Pract Proced Aesthet Dent. 2008;20:273-278.
- Lee EA. Aesthetic crown lengthening: classification, biologic rationale, and treatment planning considerations. Pract Proced Aesthet Dent. 2004;16:769-778.
- Magne P, Belser UC. Novel porcelain laminate preparation approach driven by a diagnostic mock-up. J Esthet Restor Dent. 2004;16:7-18.
- Cherukara GP, Davis GR, Seymour K, et al. Dentin exposure in tooth preparations for porcelain veneers: a pilot study. J Prosthet Dent. 2005;94:414-420.
- Lerner JM. Conservative aesthetic enhancement of the maxillary anterior using porcelain laminate veneers. Pract Proced Aesthet Dent. 2006;18:361-366.
- Spear FM. Treatment planning materials, tooth reduction, and margin placement for anterior indirect esthetic restorations. Inside Dentistry. 2008;4:54-60.
- Christensen GJ. Thick or thin veneers? J Am Dent Assoc. 2008;139:1541-1543.
- DiMatteo SM. Prep vs no prep: the evolution of veneers. Inside Dentistry. 2009;5:72-79.
- Cutbirth ST. Provisionalization for porcelain veneers using bis-acrylate and polyvinylsiloxane matrix. Pract Periodontics Aesthet Dent. 2000;12:308-312.
- Gürel G, Bichacho N. Permanent diagnostic provisional restorations for predictable results when redesigning the smile. Pract Proced Aesthet Dent. 2006;18:281-286.
Dr. Priest maintains a private prosthodontic practice in Hilton Head Island, SC. He is a Diplomate of the American Board of Prosthodontics and a Fellow of the American College of Prosthodontists and the International College of Dentists. A former professor in graduate prosthodontics at Emory University, he lectures nationally and abroad on topics including implant dentistry, advanced restorative dentistry, and aesthetic excellence. He is a regular contributor to many acclaimed dental journals. Since 2005, Dentistry Today has recognized him at a leader in continuing education. He can be reached at drgeorge@priestpros.com.
Disclosure: Dr. Preist has received financial support for this manuscript from KOMET USA. He also receives financial support from VOCO America.








